Shock

Podcast Episode
What is shock?
Shock is defined as inadequate perfusion of blood to the tissues, meaning that end organs such as the brain and kidneys aren’t getting enough blood to function properly, and so they start to fail.
The usual clinical finding is an unwell patient with a low blood pressure.
If you think of the whole system in terms of simple plumbing then it becomes really easy to understand and you can then work out how best to go about fixing it.
Your heart is a pump
Averaging around 60-100 beats per minute for the entirety of your life, your heart works continuously, squeezing blood first to the lungs then round to the rest of the body, including your brain and kidneys, which are the end organs that we’re going to focus on in this scenario.
You have the pump, you have pipes full of fluid, the blood, and you have the end organs themselves.
You also have pipes going off in all different directions to other bits of the body such as, the skin, muscle, fat, fingers and toes.
The key to understanding shock is one simple equation:
The thing we really care about is blood flow to the brain and organs, which is most accurately represented by cardiac output, but that’s rather tricky to measure directly, so we use blood pressure as a surrogate measure of flow instead.
But clearly from this equation we can see that both cardiac output and systemic vascular resistance can affect the blood flow, and understanding this is key when you’re figuring out how best to manage a patient with shock.
Now clearly, in a system with:
- a pump
- fluid
- and pipes
...there are immediately a number of ways this system can fail, and we’ll look at each one in turn.
There’s not enough fluid
This is the simplest scenario. The pump is working fine, the pipes are all clear and the blood is being supplied to the right organs, however there simply isn’t enough fluid in the system for it to be effective.
In fact, what we often see is the pump is working more than fine - it’s working overtime with a huge tachycardia to try and compensate for the fact that so little blood is available for it to pump.
We see this in severe dehydration and it’s called hypovolaemic shock. There isn’t enough volume in the system to work, and we need to fill the patient up with fluid.
Easy enough.
The natural extension of this scenario is when there’s not enough fluid because the patient is bleeding, i.e. there’s a leak in the piping somewhere. This is haemorrhagic hypovolaemic shock.
So filling up the patient with fluid is going to temporarily help, assuming you can reintroduce fluid faster than it leaks out, and it will temporarily give you a better looking blood pressure on the monitor.
But if you don’t fix the leak, then you’re just masking the problem, and even worse, you’re replacing the patient’s blood, with all of it’s wonderful oxygen carrying capacity, sugar and clotting factors, with salty water that is only going to make the whole problem a lot worse in the long run.
The patient in haemorragic shock needs two things
Firstly, we need to turn the tap off. The bleeding to be stopped, either with
- Drugs to promote vasospasm such as adrenaline
- Drugs to promote clotting such as tranexamic acid and clotting factors
- Physical intervention like direct pressure, suturing, damage control surgery or blocking off the culprit artery, (which is called artery embolisation, and sometimes used for major obstetric haemorrhage to stop bleeding from the uterus).
Secondly, we need to fill them back up with the good stuff
- Packed red blood cells
- Platelets
- Fresh frozen plasma
- Also specific clotting factor complexes and cryoprecipitate
Blood products are far better than crystalloid fluid. In some circumstances during surgery you can even suction up the patient’s own lost blood, filter and clean it, and give it back to the patient, and this is called cell salvage.
The fluid is going to the wrong place
So what if the pump is working fine, and there’s enough fluid in the system, but it’s being sent to the wrong places?
Instead of channeling down the main supply pipes to the important organs, for some reason it’s diverting off down all these other routes to the skin, muscle, fat and limbs. As a result the blood pressure is dropping because there’s not enough resistance in the system for the heart to squeeze enough blood pressure to the brain and kidneys.
This is distributive shock and it’s what we see classically in anaphylaxis and sepsis.
Widespread inflammatory mediator release causes vasodilatation or relaxation of these little blood vessels, which drops that all important resistance and allows the blood to divert away from the important organs.
These patients are often hot and flushed, because their warm, oxygenated blood is being diverted near the skin.
Now if we just look at the pipes between the heart and the important organs, then it looks a bit like hypovolaemic shock, because in these pipes, there’s not enough fluid, but in the system as a whole, there definitely is, it’s just all in the wrong place, being diverted to the peripheries.
This is an important distinction to make because it dramatically affects our management.
If we treat this like hypovolaemic shock, by piling a load more fluid in, then we rapidly encounter a problem.
Temporarily, we will see a slight increase in the blood pressure because for a short while we’ve increased the circulating volume in the important pipes.
However this fluid will rapidly distribute to the wrong areas as well, and we end up back where we started, but this time the patient has fluid overload in the skin, muscle, fat and limbs, and this is why patients with severe sepsis and anaphylaxis become swollen and oedematous. In severe cases it can collect in the lungs as well and cause pulmonary oedema, so we need to be judicious with our fluid management.
The key here to the management is to increase the resistance in those peripheral vessels, and divert blood back to the major organs. If we refer back to our original equation of blood pressure = cardiac output multiplied by systemic vascular resistance, it’s clear that if our cardiac output is fine, but we have low resistance, then the blood pressure will be low as well. If we then increase the resistance, we bring the blood pressure up with it.
We see this in our two classic examples:
- Adrenaline in anaphylaxis
- Vasopressors in sepsis
These powerful drugs induce vasoconstriction by stimulating the vascular smooth muscle to contract, and it does this more in the peripheral small blood vessels, diverting the blood back to the important organs that we want to support. Clearly, this will impact on blood supply to the fingers and toes, and is certainly something to be mindful of, as patients on prolonged infusions of multiple vasopressors will invariably develop ischaemic digits and may require amputation in the worst cases.
The pump fails
Simple concept, your pump isn’t pumping.
For whatever reason the pump in the system isn’t moving the fluid around the body effectively, so the blood becomes stagnant in the pipes, the organs don’t receive enough flow, and you end up with these organs, the brain and kidneys, starting to fail because they simply aren’t receiving enough flow to provide the oxygen and fuel required to function.
Fluid then backs up in your inferior vena cava and your capacitance vessels, because it isn’t being pushed forward effectively into the arterial system.
This pump failure is called cardiogenic shock, and it’s what we see in heart failure, or in a heart attack or myocardial infarction. A part of the heart muscle’s blood supply is cut off by a clot or a thrombus, and that muscle dies or starts dying. The pumping function of the heart decreases, and you go into cardiogenic shock.
There’s enough fluid in the system, so giving more fluid isn’t going to help these patients. In fact, it’s going to make it much worse, because the pump is already struggling to manage the fluid that is already there, so adding more is simply going to overload it, and the fluid will leak out into the lungs and the tissues, causing the oedema that we see in heart failure patients.
Equally, a vasopressor that squeezes the blood vessels to increase resistance is also useless, because it will simply increase the resistance faced by the failing pump, making the heart fail even further.
If you think about what your classic cardiac patient looks like, they’re cold and clammy, and drenched in sweat. This is because they’re in sympathetic overdrive, as the damage to the heart causes an enormous release of adrenaline. This natural adrenaline causes the vasoconstriction, so these patients are already maximally vasoconstricted.
That part of the equation - the systemic vascular resistance - is very high, it’s the cardiac output that’s low.
What needs to happen is we need to increase the pump function, and boost the cardiac output. This can be achieved in a number of ways:
- We can treat the root cause of the problem. We can unblock the coronary artery causing the heart attack, restore the blood supply to that muscle and get the heart pumping better. This is called PCI or percutaneous coronary intervention
- We can bypass the blockage by plumbing another bit of blood vessel from somewhere else onto the coronary artery, diverting blood around the obstruction to the muscle that’s not being supplied. This is a cardiac bypass
- We can help the heart pump with a mechanical pump implant, or a left ventricular assist device - if you’ve seen the episode of Gray’s anatomy where they cut the dude’s LVAD wire to get him a transplant sooner, that’s what they’re referring to.
- We can pace the heart with electrical impulses to make it contract harder, as seen in temporary or transcutaneous pacing
- And finally we can use inotropes, which are drugs that cause the force of contraction of the heart to increase, usually by increase concentration of calcium within the heart muscle, and these include drugs such as dobutamine and levosimendan
- Note how inotropes are different to vasopressors. Inotropes increase contractility of the heart, and increase cardiac output, while vasopressors squeeze the blood vessels and increase systemic vascular resistance. People often use the term interchangeably, but they’re very different drugs.
So we’ve talked so far about:
- Hypovolaemic shock - in which case we need to fill them up with fluid or blood, and fix any bleeding
- Distributive shock - where the fluid is being pumped to the wrong place, as seen in sepsis and anaphylaxis, which we can initially help with a bit of fluid, but mainly need to treat with vasopressors
- Cardiogenic shock - or pump failure, where we need to either support the heart, or increase cardiac output with inotropes like dobutamine
The last category of shock is obstructive shock.
Obstructive Shock
This is a blockage in the pipes.
Due to the high blood flow in the aorta, and rapidly decreasing vessel size in the arterial system, it is spectacularly uncommon to see a blockage occur that causes shock just by impeding systemic arterial blood flow.
The one caveat would be during interventions such as REBOA or using an intra-aortic balloon pump, in which case the aorta can be obstructed either on purpose or accidentally by a balloon, but clearly this is not something that occurs naturally.
However we need to remember that the heart has a dual circulation, and that all blood flow to the left side of the heart needs to come from the right side of the heart, via the lungs.
Now this blood flow to the lungs is much lower pressure, and therefore much more susceptible to blockage, and this is what we see in a case of pulmonary embolism. A wedge of blood clot, usually from a thrombus that forms in the deep veins of the leg or pelvis, breaks off and embolises through the right side of the heart to the pulmonary circulation, where it gets lodged in one of the blood vessels.
Now this happens all the time
But on a very small scale, and one of the many functions of the lungs is to act as a bit of a filter for debris in the blood, as the fragments of clot get lodged in the tiny capillaries and taken out of the circulation.
Blocking a capillary or two has essentially zero impact on the blood flow as a whole, so you don’t even notice it.
However if you have a large enough clot break off, it will get lodged in a much larger vessel.
The largest clots will cause a saddle embolus which literally blocks off both the right and left pulmonary arteries and can cause near total obstruction of blood flow to the lungs.
Submassive PE with saddle embolus, RV/LV 1.5. Corked thrombus (aka ex-DVT) in the @InariMedical #Flowtriever extracted through IVC into the Dryseal sheath. Ability to maintain wire access extremely useful. On table improvement in PAP: 68/11–>26/6. #noICU #notPA #noCTEPH pic.twitter.com/lUVuWfKALR
— Raj Khalsa, MD (@IRKhalsa) August 28, 2020
Clearly if we are sending no blood to the lungs, then no blood is returning to the left side of the heart, and therefore no blood is being pumped around the body. This is why we see the classic presentation of sudden shortness of breath, low blood pressure and collapse in patients with massive pulmonary embolism.
Let’s look at our equation again.
Blood pressure is low, because cardiac output is low - there’s no flow.
Systemic vascular resistance could be high or low, it doesn’t really matter because the central vascular resistance is so overwhelmingly high that equation falls apart.
- There’s no benefit to giving fluid, there’s usually enough in the system, they just need that obstruction sorting out
- Increasing systemic vascular resistance also isn’t going to help as the resistance is high enough already - They just need that blockage unblocking
- You could give them inotropes to improve the contractility of the heart, but again, the cardiac function may actually be pretty good, there’s just a blockage that needs taking out.
These patients can have thrombolysis drugs to break down the clot, such as alteplase which dissolve the clot, or they can undergo a mechanical thrombectomy which is an interventional radiology procedure to physically remove the clot.
You can have a combination of all of the above
As always with anything in medicine there are no hard and fast rules, and you can have a combination of any or all of the above examples.
Cardiac tamponade is sort of an obstructive and sort of a cardiogenic type picture. It’s probably more an obstructive shock. A collection of fluid rapidly accumulating in the pericardium causes compression of the heart, preventing it from expanding during diastole. It can contract without too much trouble, but when it tries to relax and expand to fill with blood during diastole, it cannot fill effectively, making the next contraction much smaller volume and a low cardiac output.
The treatment here is to drain the tamponade fluid or remove the clot if it’s clotted blood in the pericardial sac.
drug induced hemopericardium
— Zouheir Bitar (@zbitarsonoicu) April 29, 2023
A 74-year-old lady with Af on dabigatran was admitted with hypotension. No GI hge, no hematuria
echocard showed large pericardial effusion pic.twitter.com/8qChPLLSdB
Now you could argue this is cardiogenic shock because the pump is failing, but you could also argue it’s an obstructive picture because there is a physical obstruction preventing the heart from relaxing - the heart would work fine if that obstruction weren’t there.
So you can appreciate that there’s nuance as to how things are classified. But as long as you understand there are different types and different pictures of shock, then you’ll be able to appreciate that you need to adjust your management depending on the individual patient situation.
A lot of people will just memorise, ‘if low blood pressure, give fluid’, and while that will work a lot of the time at least temporarily, you need have an understanding of the underlying cause of the low blood pressure to treat it effectively.
It may be a mixed picture
You might have a patient with acute heart failure, but it may be that the heart failure was triggered by a urinary tract infection. So they may have an element of cardiogenic shock from the acute heart failure, but also a bit of distributive shock from their sepsis.
Equally a patient who has lost a lot of blood and is still actively bleeding, it may be that they’re hugely acidotic and have myocardial dysfunction from that, and they’ll have an element of cardiogenic shock on top of their hypovolaemic shock, so it’s important to look at your patient and assess what type of shock you think is predominating, and whether there’s a mixture, and make sure you’re addressing them appropriately.
Measuring shock
Now the way we measure shock, or grade it, depends on how much blood volume we think they’ve lost in the case of hypovolaemic or haemorrhagic shock, either as an absolute volume or as a percentage of their total circulating volume. We can also look at what organ dysfunction is present, and the organs that we look at are
- heart
- brain
- kidneys
If you look up ‘grading of shock’, you’ll notice that it has classes 1 - 4.
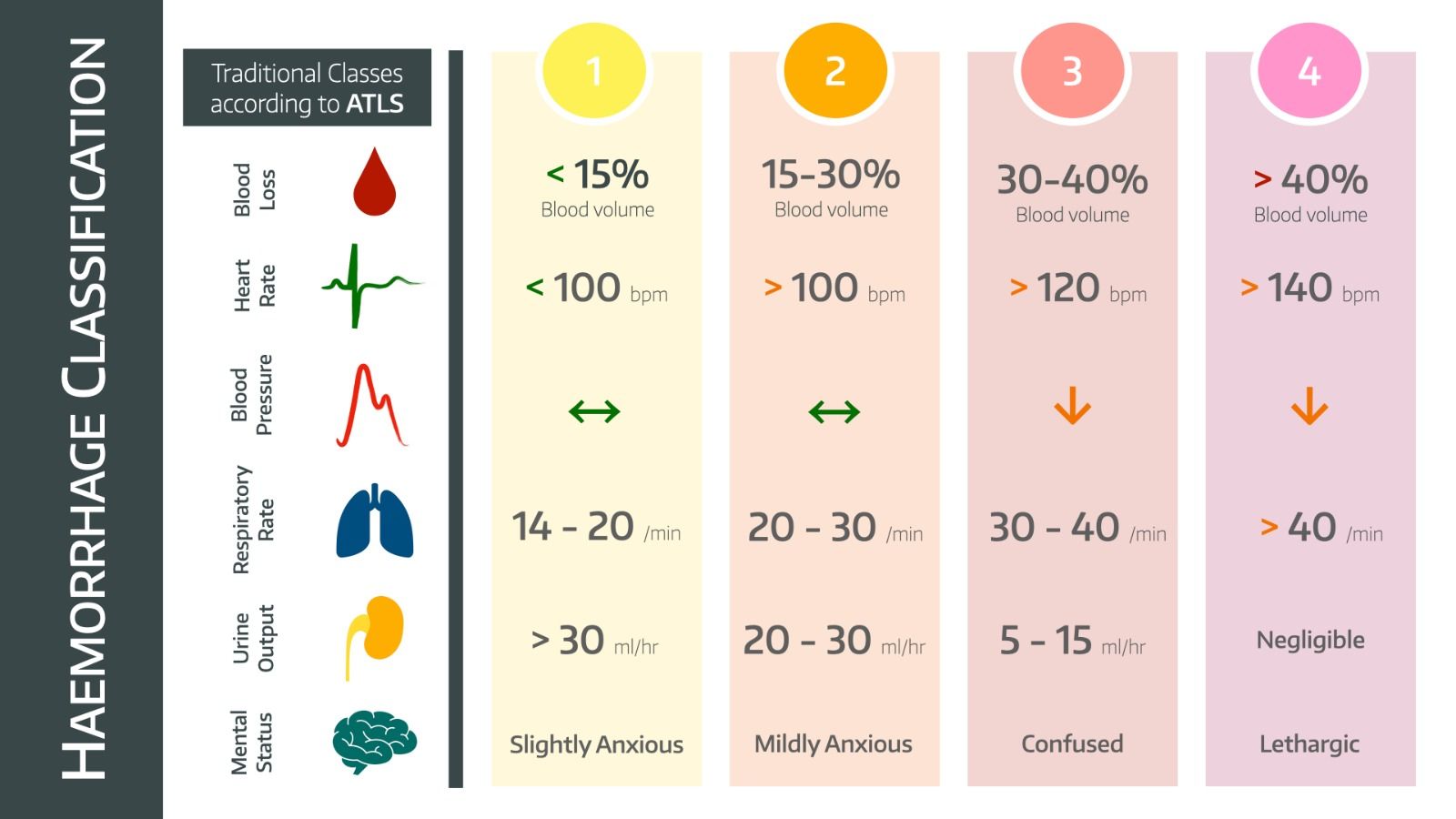
Remember young people can compensate very effectively for blood loss, so can lose a substantial volume before showing any signs. Be very aware of a patient with a normal blood pressure but who is bleeding and tachycardic.
So you can see from our original equation that by working out the cause of your shock you can work out why someone’s blood pressure is low, and assess the severity by looking at their end organ function, particularly brain and kidneys.
And hopefully you’ll have a bit of a better idea of how to go about fixing it.
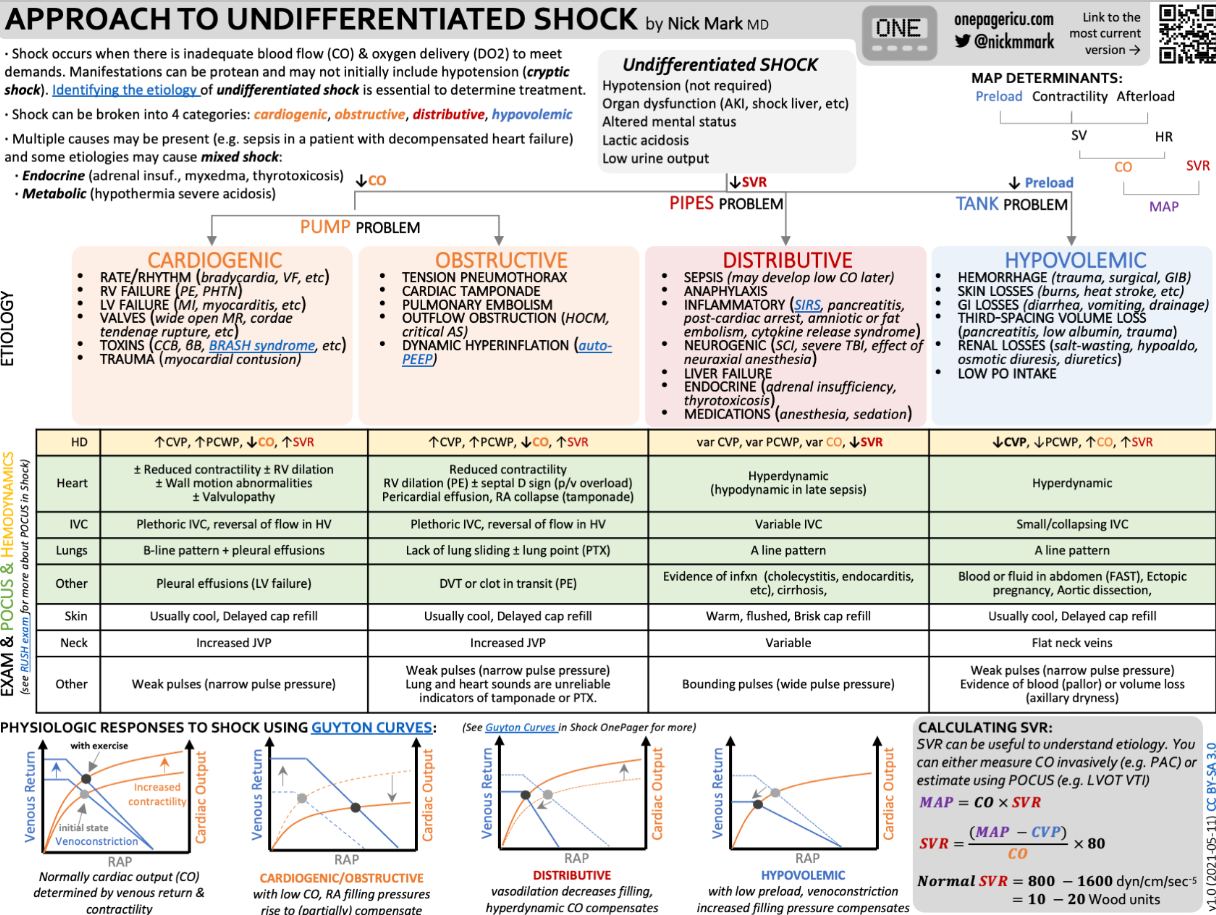
An amazing infographic
If you're not familiar with the genius of Dr Nick Mark over at ICU one pager then you're missing out. He produces fabulously informative and beautiful summaries of high yield topics in a memorable and approachable way - we recommend them highly!
You can follow Dr Nick Mark here
Lots more useful stuff
✅Guidelines for choice of fluids in #ICU pts
— Yuki Kotani, MD | 小谷 祐樹 (@YukiKotani5) September 29, 2022
🤝24 experts from societies of anesthesia/intensive care medicine and emergency medicine🇫🇷
4 settings
▶️sepsis
▶️hemorrhagic shock
▶️acute brain injury
▶️peripartum period
🔗https://t.co/wpfLPP350P#FOAMcc #cardiovascular pic.twitter.com/IGY4GAkrY8
The RePHILL Trial;
— TheResusRoom (@TheResusRoom) April 4, 2022
Are blood products superior to saline for prehospital haemorrhagic shock?https://t.co/JllNsEB79dhttps://t.co/ipr8fDYKCihttps://t.co/RNpmm817fz #FOAMed pic.twitter.com/I3iP5f02lZ
🆕ICU #OnePager about #LVADs in collaboration with @EricLawson90!
— ICU OnePager (@OnePagerICU) July 2, 2022
🫀 What is a left ventricular assist device (LVAD)?
⚙️How do they work?🩸What can go wrong?
Hint: This is one time its OK to not have a pulse!https://t.co/orXELGISpf pic.twitter.com/Qwdq9uFzOc