Congenital Heart Disease in Obstetrics

Take home messages
- Cardiac disease is the commonest cause of maternal mortality in the UK
- Don't forget the work's not done when baby is out - women can deteriorate hours to days after delivery
- By understanding the pathophysiology, you can titrate your fluids, pressors and inotropes to optimise the woman's (and baby's) outcome
Today on labour ward we had a young woman present for induction of labour, with congenital pulmonary stenosis who had undergone balloon dilatation of the valve as a baby.
In the grand scheme of things, I'm not all that experienced when it comes to obstetric anaesthesia, even less so when it comes to anaesthetising pregnant women with congenital valvulopathy, so I figured a post might be worthwhile.
Because I was frankly terrified.
The catch-all answer is that parturients with significant congenital heart disease probably need managing in a specialist centre.
But there are a lot of women in the mild-to-moderate zone - (0.8% of all pregnancies are affected by congenital heart disease in some way or another) - who don't need immediate specialist input, but will trundle into your DGH and require you as the anaesthetic registrar to be able to appreciate the nuances of their physiology to optimise their perioperative care.
Most of the time, the answer is...
- Vaginal delivery with low-dose regional analgesia, such as an epidural, and careful fluid management
Oh, and knowing when to call for specialist help.
For our lady she had been essentially asymptomatic since her valvular dilatation at 18 months of age and had a good exercise tolerance with no significant other comorbidities.
She had also had a transthoracic echo during this pregnancy that was reassuring, with LVEF 62%, no significant RV dilatation or hypertrophy and a pulmonary valve max velocity of 3.2m/s, placing her gently into the 'moderate' zone.
The plan agreed by cardiology and obstetric anaesthetist
- Can proceed with normal vaginal delivery as desired by the patient
- Early epidural and short second stage
- Spinal, CSE and General anaesthesia all viable possibilities
- Key is to avoid significant haemodynamic fluctuations, and ensuring patient is well filled
This lady ended up having an early epidural before artificial rupture of membranes, and went on to deliver successfully without any immediate issues.
Phew.
A quick recap of some of the haemodynamic changes seen in pregnancy
- Total blood volume increases by 30-45%
- Cardiac output increases by 30-50%, highest in the second trimester
- Heart rate rises, peaking at about 25% higher than baseline in third trimester
- Systemic vascular resistance is dramatically reduced by progesterone, leading to an overall reduction in blood pressure, particularly in early pregnancy
It seems to be that between 24-32 weeks is the time you're likely to see symptoms of women who are not tolerating these haemodynamic changes.
What are the highest risk congenital heart problems for women in pregnancy?
- Any cyanotic heart disease
- Severe left ventricular impairment
- Pulmonary hypertension*
- Left ventricular outflow obstruction
- Any substantial aortic disease
- Mechanical valves
*Cardiac output in pulmonary hypertension is dependent on preload, and trying to valsalva a baby out of the pelvis tends to interfer with this a smidge.
Out of the valve-specific pathologies, mitral stenosis is generally the most troublesome due to the increased risk of pulmonary oedema, and these women should be managed in specialist centres.
What are the antenatal care priorities?
As you might imagine the key is early identification. It's scary that most of the pregnant woman who die were not labelled as 'high risk' before they went into labour.
When women with congenital heart disease become pregnant, early MDT input is needed including a cardiologist, ideally a congenital cardiologist. Which sounds a bit like someone born to be a cardiologist, but apparently that's the phrase.
Then you're looking at trying to establish the level of risk involved, and how that risk can best be mitigated.
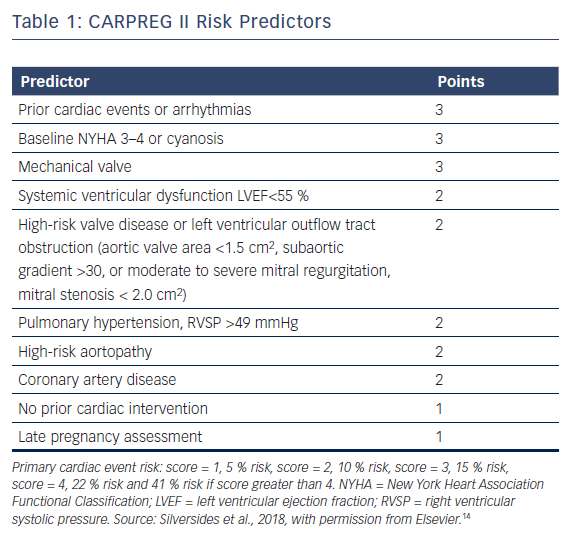
Do you know any relevant severity scoring systems?
- CARPREG risk score by the WHO
- ZAHARA (Dutch scoring system) predictor of maternal CVS problems
The mortality risk in severe cases, such as Eisenmenger's syndrome, can be as high as 50%.
Main concerns during labour
- IV access can be difficult if oedematous or many previous admissions
- Standard monitoring of pulse oximtery and NIBP is usually sufficient
- Fluid ins and outs are really important to keep track of
- If any rhythm concerns then ECG monitoring as well
- Invasive blood pressure monitoring if known ventricular dysfunction
- If severe heart failure consider CVP but probably shouldn't be doing this in a DGH...
Problems during and after labour
- Large autotransfusion of blood from uterus, and resorption of tissue oedema can cause volume overload
- Blood pressure, heart rate and cardiac output all increase during labour
- Pain, hypercapnoea, hypoxia and acidosis caused by labour will increase pulmonary vascular resistance
- Venous embolism can be seriously bad news if there is a right to left shunt
This added fluid load and cardiovascular stress can cause women with congenital heard disease to decompensate rapidly
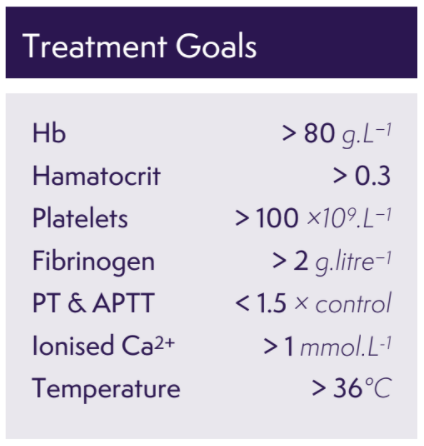
How do I manage bleeding?
Carefully.
The priority as always is delivery of oxygen to brain and vital organs, so manage haemorrhage as you would, with this goal in mind.
Things to be aware of are the effects of the specific interventions you might employ that could make your (and the patient's) life more difficult:
- Ergometrine should probably be avoided where possible due to the haemodynamic instability and high blood pressures it can cause
- Oxytocin needs some thought and risk/benefit analysis
Again, oxytocin is ideally avoided as it causes a drop in systemic vascular resistance and tachycardia, as well as fluid retention, which is suboptimal in significant cardiac disease. But if a small dose is given very slowly, it might be significantly preferable to ongoing haemorrhage with the associated fluid and blood product overload in attempting to manage it without oxytocin.
Remember patients with a fixed cardiac output tolerate haemorrhage very badly indeed.
- If your woman has a metallic valve then hopefully she has been anticoagulated, ideally with unfractionated heparin, and even more hopefully it was stopped 4-6 hours before anything important kicked off
- Blood products should generally otherwise be given targeting your standard parameters for major obstetric haemorrhage, just be cautious about fluid overload
Why we like epidurals
They're fairly simple, fun to do and they take away pain, what's not to love?
Yes of course there are risks associated with needles near important nerves, but when perfomed as instructed, epidurals represent a safe and highly effective way to not only provide powerful analgesia to the exhausted labouring woman, but can also improve cardiovascular outcomes as well.
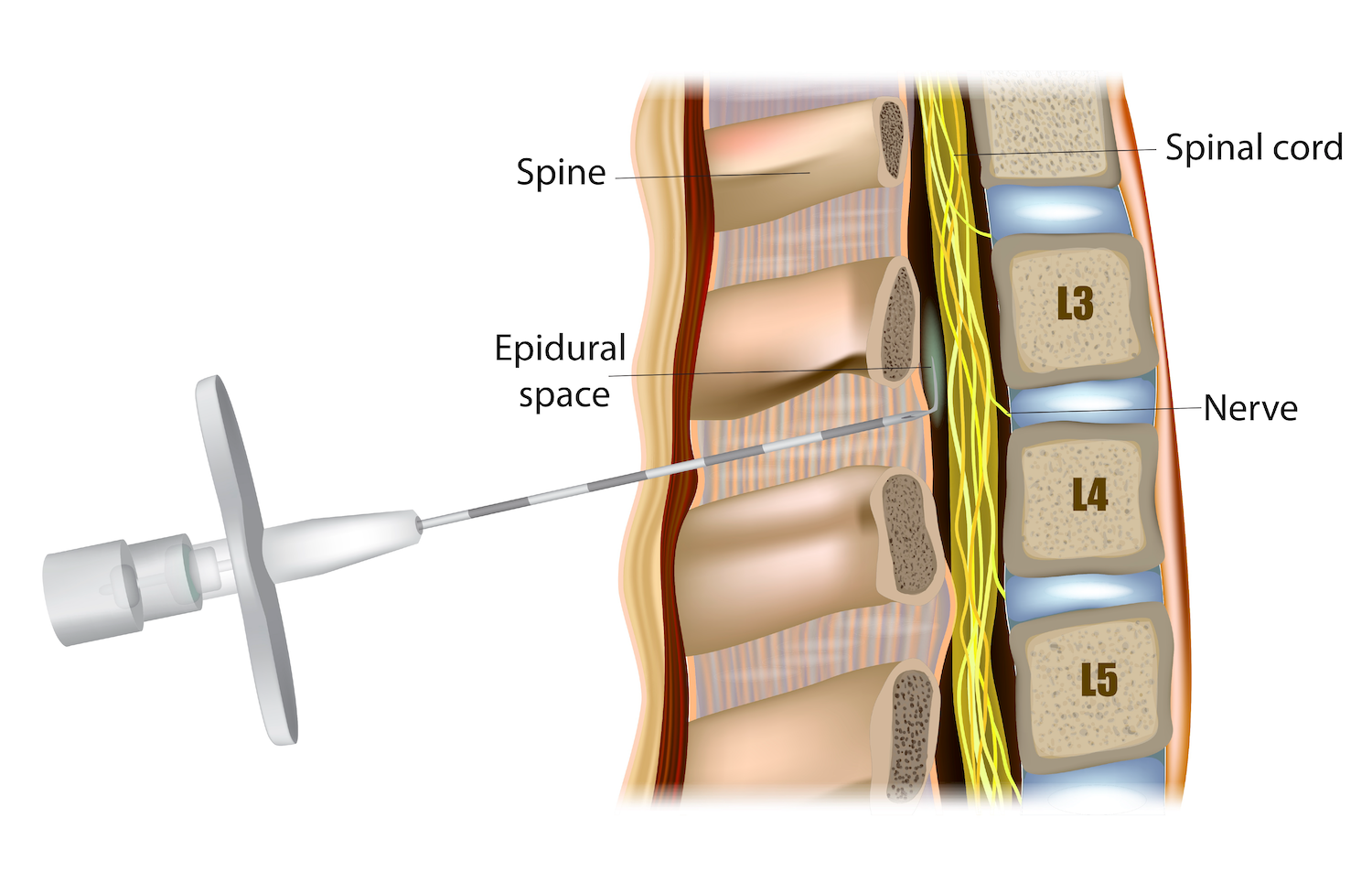
Things an effective epidural can achieve
- Reduced sympathetic stimulation, and blood pressure, as a result of pain
- Reduced heart rate and myocardial oxygen demand
- Vasodilatation and reduction of systemic vascular resistance
- Facilitates assisted delivery to reduce the amount of pushing, and therefore the amount of IVC compression
- Can be used for Caesarean section, avoiding the haemodynamic volatility associated with spinal or general anaesthesia
- Sleep - which is just generally helpful all round
Are there any risks of congenital heart disease to the baby?
Apart from the obvious foetal risks associated with maternial cardiovascular instability, in approximately 25% of pregnancies with heart disease, babies may have:
- Premature delivery
- Small size for gestation age
- Respiratory distress
And children are at a higher risk of having congenital heart problems themselves as well.
Which cardiovascular drugs can cause issues in pregnancy?
- ACE-inhibitors - Craniofacial defects and oligohydramnios
- β-blockers - Intra-uterine growth restriction, neonatal hypoglycaemia and bradycardia
- Warfarin - Teratogenic and risk of foetal bleeding
What about afterwards?
Around half of maternal deaths from heart disease occured in the six weeks after baby was born.
Post-operative monitoring and follow up is really important. How long a woman stays in hospital and when they are reviewed is very individual, and will depend on the pathophysiology, severity and how the labour and delivery went.
Useful Tweets and Resources
- Check out this Anaesthetic Tutorial of the Week on cardiac disease in pregnancy
- If you're looking for some practice CRQs, check out these wonderful examples by our colleagues over at FRCA-revision.com
🎙New Episode 🚨!! “Episode 172: A Pregnant Patient with Congenital Heart Disease” — We welcome a panel of experts to discuss the management of a pregnant patient with congenital heart disease, & the preop evaluation, ob management, & postop care. @jwolpaw https://t.co/udBOys6YYQ
— ACCRAC Podcast (@accracpodcast) May 1, 2020
⚠️Canadian Cardiovascular Society: Clinical Practice Update on❤️Management of the #Pregnant Patient #CardioObstetrics #WomenHeartHealth #CardioEd
— Diego Segura-Rodriguez (@SeguraCardio) July 2, 2021
🔸#ValvularHeartDisease, Cardiomyopathy, Ischemic heart disease, #Arrhythmias, Aortic disease, Congenital heart disease, PH
@CJC_JCC pic.twitter.com/zFRO4JJUvr
References and Further Reading

Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
