Opioids
What is an opioid?
- A drug that acts on opioid receptors
- Opiates are a subset of opioids, which occur naturally, such as morphine
- They are commonly used to treat acute pain, and also as co-induction agents for general anaesthesia
- They are also used in regional anaesthesia techniques such as epidural and spinal blocks
- Side effects include nausea and vomiting, respiratory depression, pruritus, constipation and confusion
Objectives
- Recall the pertinent chemical, pharmacokinetic and pharmacological properties of Fentanyl, Alfentanil, Remifentanil, Morphine and Diamorphine
- Compare and contrast the properties of these drugs and their clinical uses in anaesthetic practice
- Use this knowledge and understanding to select an appropriate opioid for use at induction, for regional anaesthesia, for Awake Fibreoptic Intubation and for intra/post-operative analgesia in various clinical scenarios
Why do we use opioids?
Indications for opioids include
- Analgesia
- Anxiolysis
- Cough suppression
- Treatment of diarrhoea
What effects and side effects do opioids have in common?
Respiratory
- Respiratory depression
- Reduced sensitivity to hypoxia and hypercapnoea
- Suppression of laryngeal reflexes
- Chest wall rigidity
Cardiovascular
- Bradycardia
- Hypotension
Neurological
- Analgesia
- Anxiolysis
- Drowsiness
- Miosis
GI/GU
- Emetogenic
- Constipation
- Sphincter of Oddi spasm
- Urinary retention
Side effects
- Histamine release
- Bronchospasm
- Urticaria and pruritus
- Hypotension
- Dependence
- Tolerance, dependence and addiction can develop with chronic use
Morphine
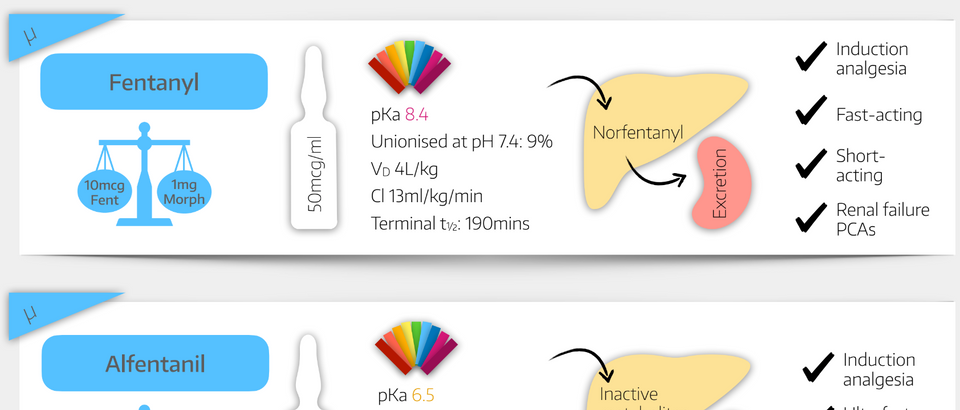
Fentanyl
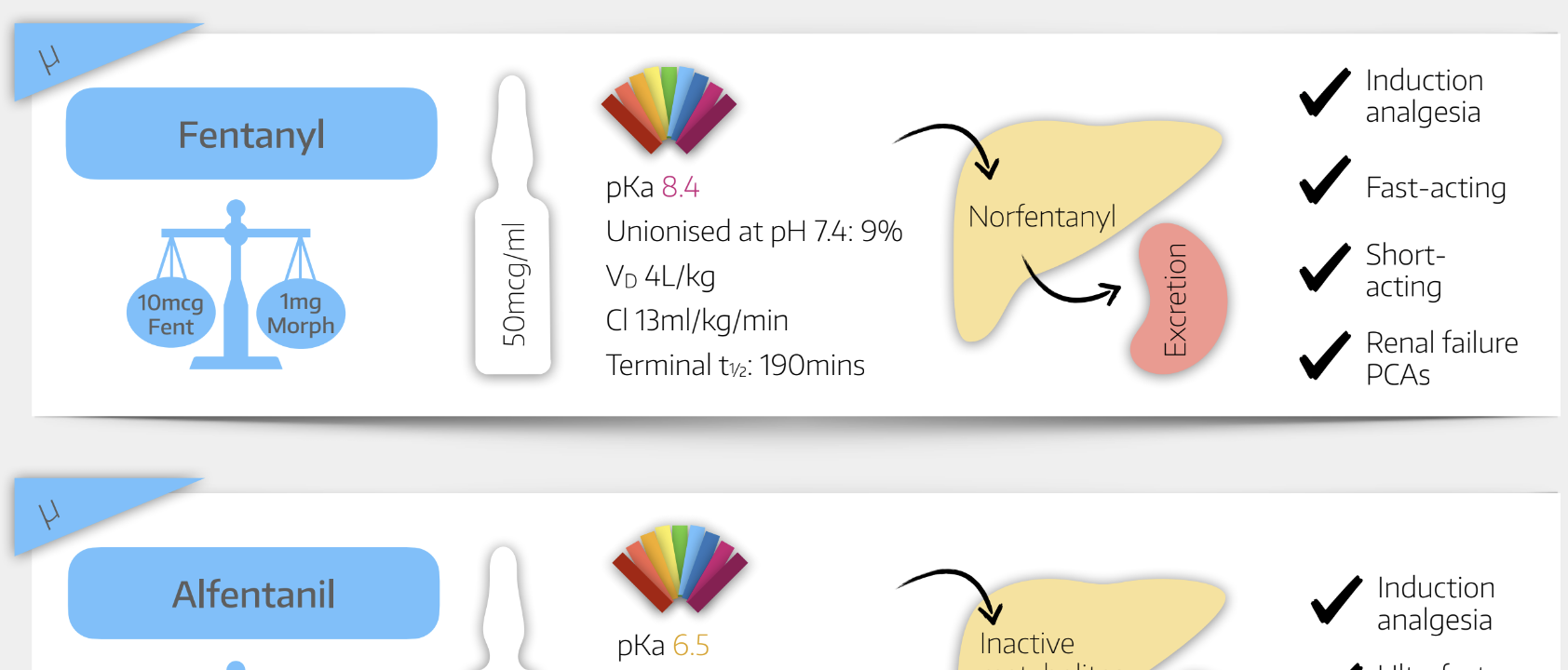
Alfentanil
Remifentanil
Diamorphine
What you need to know
- Diamorphine = Heroin = Diacetylmorphine
- Diamorphine has no intrinsic activity at opioid receptors
- Once it is deacetylated, it can exert its effect in the form of morphine
- 1mg Diamorphine = 2mg Morphine
- Diamorphine is much more lipid-soluble than morphine, making it ideal for use in neuraxial anaesthesia (spinal / epidural) where barriers such as the dura need to be crossed in order for it to exert its effect
Example OSCE/SOE question:
Tell me about diamorphine
Class and uses
- Diacetylated morphine derivative prodrug
- Metabolised to 6-monoacetyl morphine and morphine
- Used for analgesia, premedication and anxiolysis
Presentation and dose
- Tablets 10mg
- White powder for injection
- 5, 10, 30, 100 or 500mg vials of diamorphine hydrochloride
- 0.1-0.4mg intrathecal dose
- up to 3mg epidural dose
- up to 10mg IV for severe dyspnoea in pulmonary oedema
- Can also be given intrathecally or via the epidural route
Mechanism of Action
- μ receptor full agonist
Effects and side effects
Respiratory
- Respiratory depression
- Respiratory rate particularly affected
- Reduced sensitivity to hypercapnoea and to a lesser extent to hypoxia
- Suppression of laryngeal reflexes
- Chest wall rigidity
- Possibly via interaction with dopamine and GABA in the substantia nigra
Cardiovascular
- Bradycardia
- Hypotension
Neurological
- Analgesia
- Better for visceral pain than sharp pain
- Anxiolysis
- Drowsiness and sedation
- Triggers the most euphoria of all the opioids hence its addictive nature
- Miosis
- Stimulates the Edinger–Westphal nucleus
GI/GU
- Emetogenic
- Constipation
- Sphincter of Oddi spasm
- Urinary retention
Endocrine
- Inhibits ACTH release
- Increases ADH release
Side effects
- Histamine release
- Bronchospasm
- Urticaria and pruritus
- Particularly after epidural and intrathecal injection
- Hypotension
- Dependence
- Tolerance, dependence and addiction can develop with chronic use
Pharmacokinetics
Absorption
- Highly lipid soluble so well absorbed from the GI tract but significant first pass metabolism
- pKa 7.6 so 37% unionised in the blood
- Bioavailability of 30%
- Significant first pass metabolism
- Peak effect after 10mins when given IV
- 30mins when given IM
Distribution
- Higher lipid solubility than morphine makes it faster acting and safer for intrathecal injection, with reduced risk of cranial spread and delayed respiratory depression
- 40% protein bound
Metabolism
- Ester hydrolysis in plasma, liver and brain to 6-monoacetylmorphine and morphine
- Half life of 5 minutes
Excretion
- Renal excretion of all metabolites, which accumulate in renal failure
Side effects
Tell me about naloxone
Opioid antagonist at three opioid receptors, used for reversal of opioid overdose or toxicity
- μ is main target
- κ
- δ
Effects
- Hypertension
- Pulmonary oedema
- Arrhythmias
Dose
- 1-4 μg/kg IV
- Short duration of action of 30 mins
A really useful reference
Download our free opioid summary pdf
Everything you need to pass the Primary FRCA

Purchase our premium study tools here, or subscribe and get them for free

