Ayre's T Piece
In 1937 Dr Philip Ayre used his namesake breathing system for the first time.

The whole contraption consists of a single light metal tube 1 cm in diameter, 5 cm in length with a side arm.
That's it.
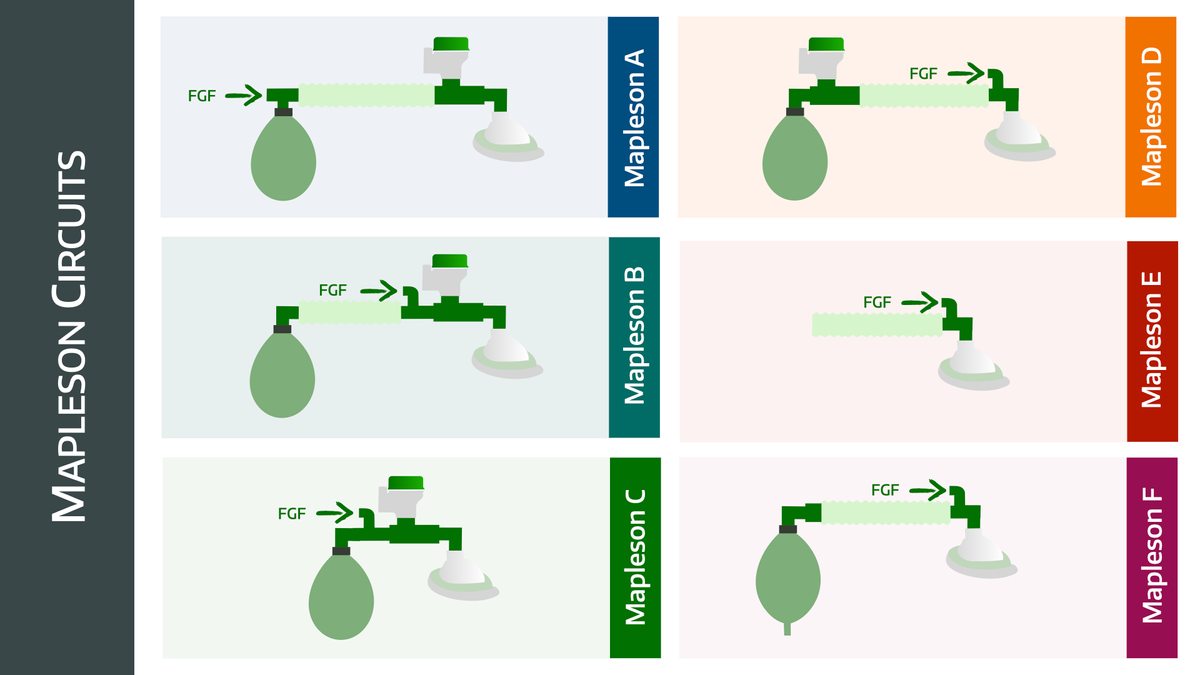
One limb of the device is sized to fit the ETT tube for the patient. Fresh gas enters the system through the side arm and the expired gas is vented into the atmosphere and there is no rebreathing.
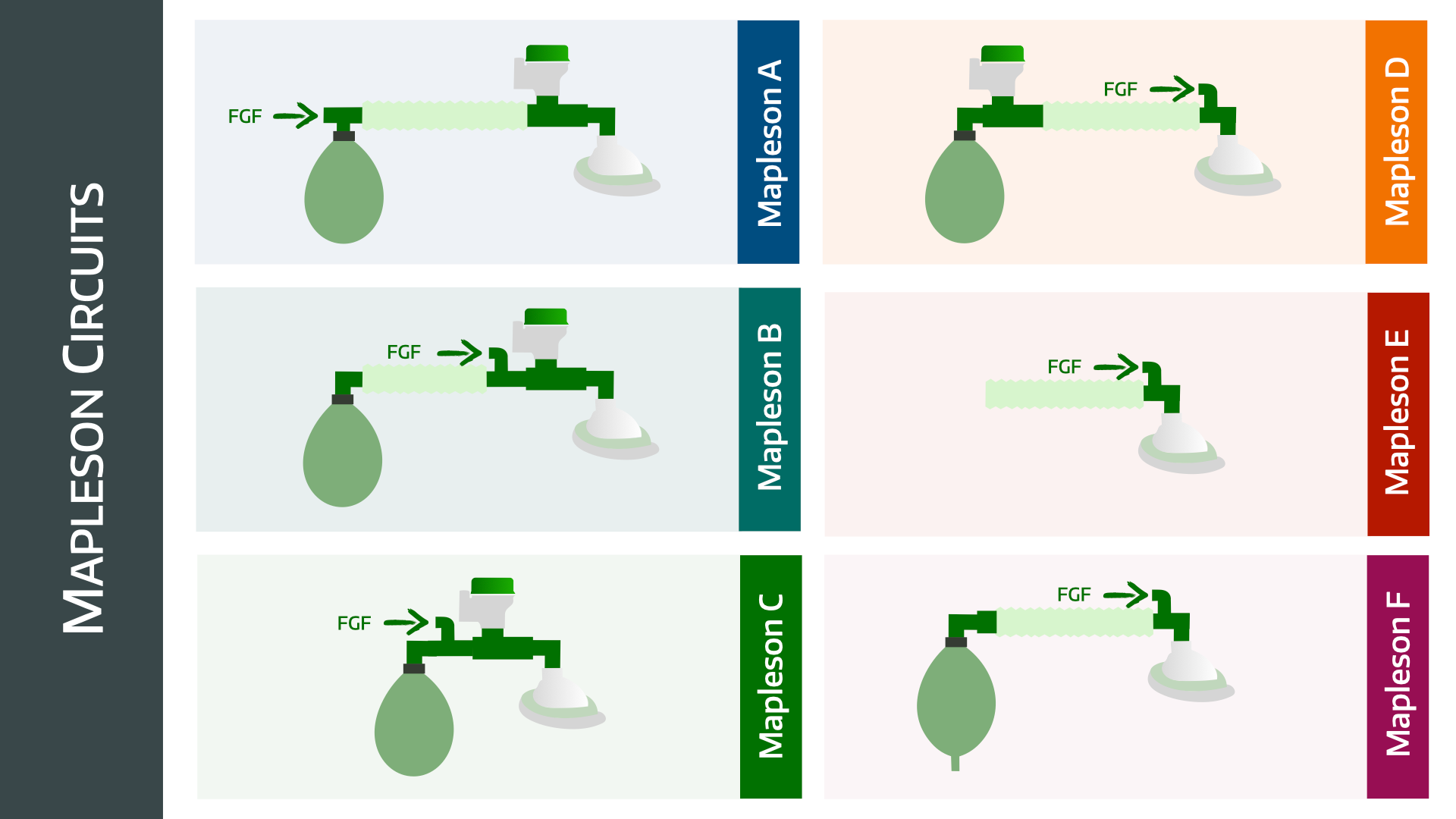
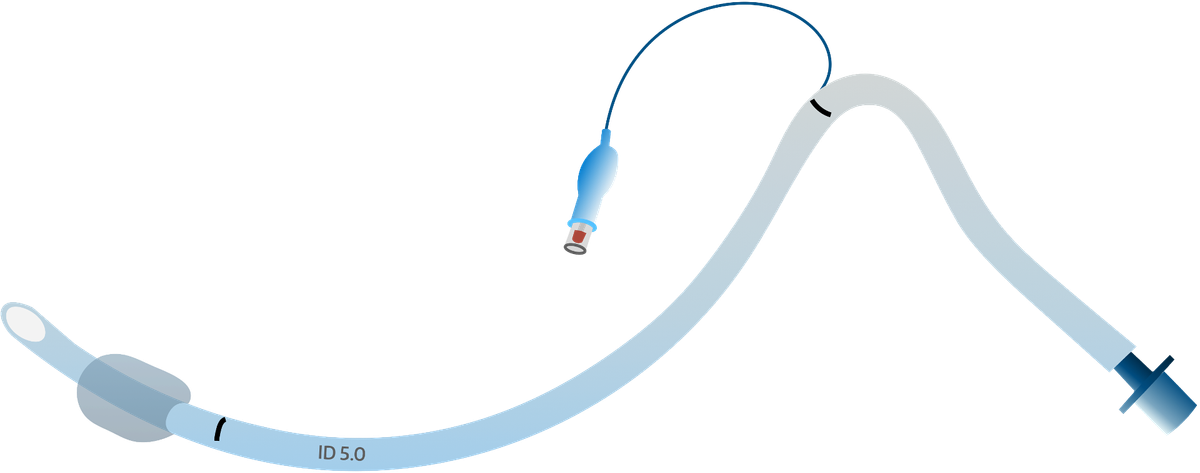
If you then stick a bit of corrugated reservoir tubing onto the exhaust end, you have yourself a Mapleson E system.
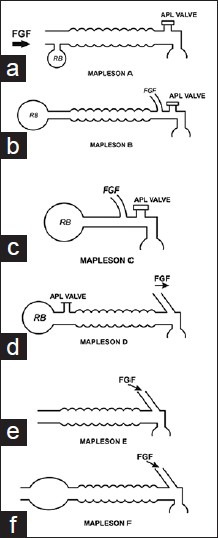
Not wanting to be out-done, Dr Gordon Jackson-Rees then added a double ended bag to the end of the reservoir tube in 1950, which allowed the anaesthetist to monitor respiration more effectively and provide intermittent positive pressure ventilation or CPAP where necessary.

This was then later further modified by closing the end of the bag, and adding an APL valve, as in the image below.

What are the features of an ideal breathing system?
- Able to deliver intended inspired gas mixture
- Efficient and allow low fresh gas flow
- Protects patients from barotrauma
- Easy and safe to use, reliable and idiot proof (say fail safe in the exam)
- Low dead space
- Effectively eliminate CO2 and waste gasses
- Efficient for both adults and children
- Efficient for spontaneous and controlled ventilation (low fresh gas flow)
- Low resistance, with minimal length, large internal diameter and no sudden curves or changes in diameter
- Cheap to make, compact and lightweight
- Allow for the warming and humidification of inspired gases
What breathing systems could you use for an 8kg 7 month old baby?
- Ayre's T-piece (Mapleson E)
- Ayre's T-piece with Jackson-Rees modification (Mapleson F)
- Humphrey ADE system (E mode is similar to T-piece)
- Paediatric circle system (if child is over 5kg)
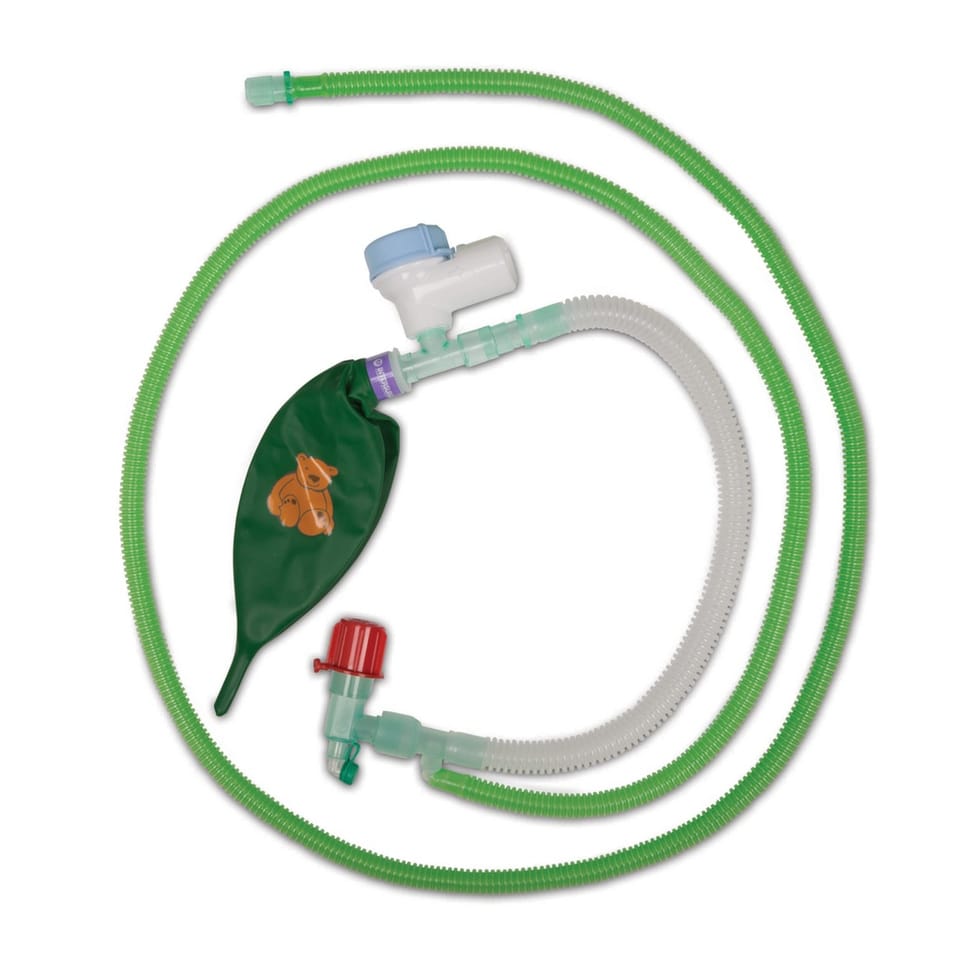
Here's a schematic of a Mapleson E breathing system
Mapleson E system is derived from Ayre's T piece configuration by simply adding a bit of tubing to the expiratory part of the circuit.
What are the components of an Ayre's T-piece?
- FGF inlet
- Expiratory limb
- Reservoir tube
The amount of tubing at the patient end (such as an HME filter etc) will determine the amount of dead space.
Explain how the Ayre's T-piece works
- Patient inhales fresh gas from the reservoir tube which has filled with fresh gas flow
- The patient then exhales into the reservoir tube
- This exhaled gas mixes with the fresh gas that's continuously fed into the system at the patient end
- During the expiratory pause, fresh gas washes the expired gas out of the reservoir tube and fills it with new fresh gas for the next breath
How can you do controlled ventilation with an Ayre's T-piece?
- For spontaneous ventilation, the patient inhales and fresh gas flow is drawn in through the side port
- The patient then exhales through the expiratory limb tubing
- To provide controlled ventilation, the expiratory limb can be intermittently manually occluded
- This will cause pressure to increase and the lungs to inflate
Clearly this cannot be done by a ventilator, but it allows the anaesthetist to provide a bit of support if the patient stops breathing or isn't taking adequate breaths.
Describe the movement of gas during the expiratory pause with a Mapleson E system.
- During inspiration, the patient inspires fresh gas from the fresh gas inlet as well as the reservoir tube
- During expiration, the patient exhales into the reservoir tube, which vents into the atmosphere, dragging along with it some fresh gas which is continuously flowing into the reservoir tube
- During the expiratory pause, the expired gas in the reservoir tube is pushed out by newly arriving fresh gas flow
- The faster the fresh gas flow, the better this is achieved
- To prevent dilution of fresh gas flow by the patient inhaling air through the reservoir tube, the reservoir tube needs to be greater in volume than the patient's tidal volume
What fresh gas flow rate is required?
- When spontaneously breathing, to prevent re-breathing you need to supply around 2-3 times the patient's minute ventilation
- For controlled ventilation with a reasonable expiratory pause, then you need 1.5 - 2x the patient's minute ventilation to avoid rebreathing
These are general guides, and need to be adjusted for the individual. If there's evidence of rebreathing, then you need to increase the fresh gas flow rate.
What are the disadvantages of the Ayre's T-piece?
- Not always possible to scavenge wasted gas
- If the reservoir tube is small and the minute ventilation high, then room air can be entrained
- If the reservoir tube is too big then there can be rebreathing
- Inefficient during spontaneous respiration (needs high fresh gas flow)
When would you use a Mapleson F system?
- Children up to 25-30 kg
- To apply CPAP to a non-dependent lung during one-lung ventilation
What are the advantages of the Jackson-Rees modification?
- Low resistance with no valves
- Compact and portable
- Works for spontaneous and assisted ventilation
- Can apply CPAP
- Helps monitor tidal volume and rate of spontaneous respiration
@anaestheasier ♬ original sound - Anaestheasier
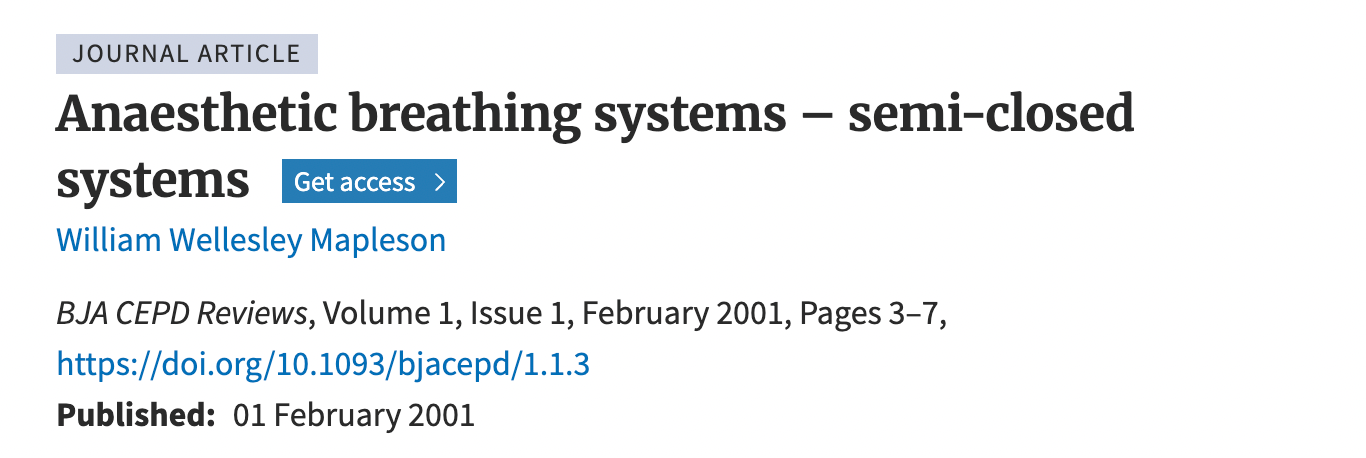
Here are all the Mapleson systems
Here's our post on breathing systems
Other airway equipment posts
References and Further Reading