Awake Tracheal Intubation
Podcast Episode
Take home messages
- Awake intubation is seriously underutilised in the UK, and we should probably be using it more to ensure we're well skilled when we really need it
- For the exam, you need to know the indications, technique and contraindications inside out
Intubation is scary
The thought of rendering a stranger unconscious, and possibly paralysed, before popping a plastic tube between their vocal cords and breathing for them is rather daunting, and that's on a good day when you can intubate them in a traditional manner.
But every so often along comes a challenge.
Not everyone is safe to undergo the traditional asleep oral tracheal intubation, either under direct laryngoscopy or videolaryngoscopy, and we need to employ another tactic.
Enter awake tracheal intubation.
The idea here is that we keep the patient conscious (or slightly sedated) and breathing for themselves. That way if we find we can't introduce a tracheal tube safely between the cords, we haven't just lost their airway and potentially done a rather large amount of harm.
Who's not safe to have a conventional asleep intubation?
Anyone you suspect will be very difficult to intubate or to ventilate, whether that is with a facemask, supraglottic airway device, or laryngoscope, and there are many factors that can be used to predict whether a patient is likely to be tricky to manage.
Some examples include:
Difficult facemask ventilation
- Obesity
- Craniofacial abnormalities
- Big beard
Difficult laryngoscopy
- Neck stiffness
- Oropharyngeal Tumour
- Distorted anatomy
- Trauma or burns
If you're stuck for an answer in the exam, then saying 'previously difficult' intubation or ventilation will almost certainly get you a mark.
For a more complete list, scroll down to the questions in the members area, or the references listed below.
But there's an issue.
It's rather tricky to persuade even the most obliging of customers to tolerate a tube tickling the most sensitive part of their anatomy. The cough reflex, after all, is probably the most powerful reflex we have, and for good reason - it's lifesaving.
So we need to achieve two things:
- A calm, cooperative patient who will allow us to spend a few minutes fiddling about in their upper airway
- A desensitised pharynx and vocal cords to prevent this cough reflex from screwing up the whole plan
To achieve this, we usually combine some form of conscious sedation and topicalisation, which you can see detailed in the video below.
A TikTok how-to guide
@airwaytrainingqeqm Awake Tracheal Intubation Training @ EKHUFT/ QEQM
♬ An emotional and happy song (long) - bunka
If the video does not load correctly, click here
What does the Difficult Airway Society recommend?
- Awake tracheal intubation must be considered in the presence of predictors of difficult airway management.
- A cognitive aid such as a checklist is recommended before and during performance of awake tracheal intubation.
- Supplemental oxygen should always be administered during awake tracheal intubation.
- Effective topicalisation must be established and tested. The maximum dose of lidocaine should not exceed 9 mg.kg−1 lean body weight.
- Cautious use of minimal sedation can be beneficial. This should ideally be administered by an independent practitioner. Sedation should not be used as a substitute for inadequate airway topicalisation.
- The number of attempts should be limited to three, with one further attempt by a more experienced operator (3 + 1).
- Anaesthesia should only be induced after a two-point check (visual confirmation and capnography) has confirmed correct tracheal tube position.
- All departments should support anaesthetists to attain competency and maintain skills in awake tracheal intubation.
A few different options
Once you have a patient who is comfortably sedated, and still breathing, with nicely numb vocal cords, you have a couple of different options for how you actually insert the tube into the trachea.
Awake Videolaryngoscopy
This is just like your normal video-assisted intubation, except you have to remember the patient is still awake.
It is a rather strange experience, when you're used to performing laryngoscopy with the patient firmly asleep, especially when they try and talk to you and you see their vocal cords flapping around wildly on the screen.
It certainly has its place, however there are clearly occasions when it's not going to work so well, such as severely limited mouth opening, and it's not as commonly employed as our second technique.
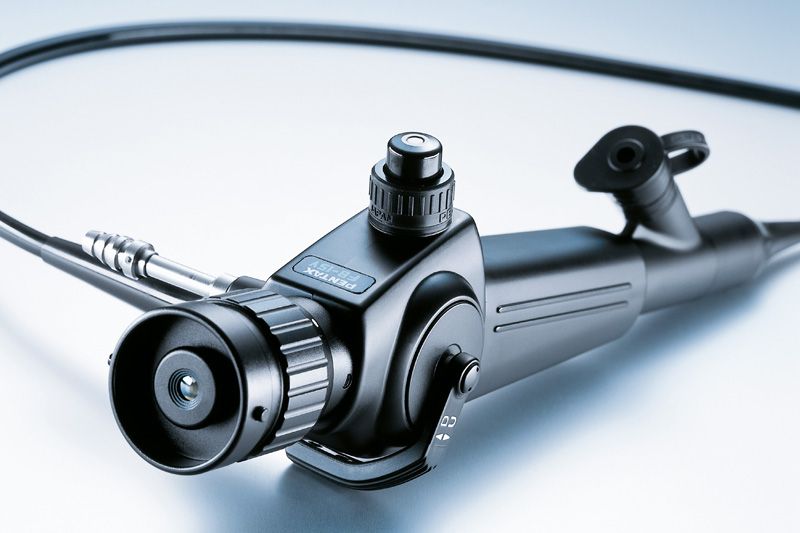
Awake Fibreoptic Tracheal Intubation
First performed by Dr Peter Murphy in 1967, who hopefully cleaned his surgical choledochoscope before shoving it down someone's windpipe, this technique has reigned supreme when it comes to difficult intubation - and for good reason - it works.
A Case Study
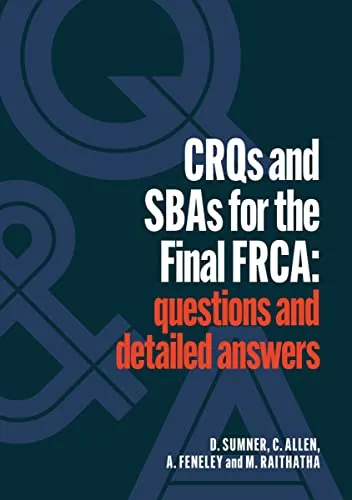
This case has been kindly donated by Sumner et al. from their wonderful book "CRQs and SBAs for the Final FRCA: questions and detailed answers", the link for which you can find in the resources section at the bottom of this post.
A 69 year old woman presents for an elective right hemi-colectomy for colon cancer. Her past medical history includes rheumatoid arthritis, with limited neck movement. Upon review of her previous anaesthetic charts, you notice she has a ‘known difficult airway’.
Question 1
List two indications, for one mark, and four contraindications, for two marks, for awake fibre-optic intubation.
Indications:
- Known or predicted difficult airway
- High risk of aspiration
- Inability to access pre-tracheal or cricoid region
- Cervical spine instability needing in-line stabilisation
In terms of contraindications, there are only really two that are absolute:
- Patient refusal
- Allergy to any of the agents intended for use
All other contraindications are relative and include:
- Blood in the airway
- Coagulopathy, if using the nasal route
- Peri-glottic masses or stridulous patients where you think the scope is simply not going to be able to pass the obstruction, in which case you may be considering awake surgical tracheostomy
Question 2
Name six terminal nerves that have to be blocked, via direct injection or topicalisation, to provide anaesthesia for an awake fibre-optic intubation.
- Anterior ethmoidal nerve
- Greater and lesser palatine nerves
- Glossopharyngeal nerve
- Tonsillar nerve
- Lingual nerve
- Superior and recurrent laryngeal nerves
Question 3
What is the maximum dose of lidocaine that can be used for topicalisation of the airway?
- 9 ml/kg of lidocaine for mucosal administration
- 3mg/kg for subcutaneous
- 7 with adrenaline
I remember li-do-caine has three syllables, and li-do-caine-ad-ren-a-line has seven.
Question 4
What is the quantity of lidocaine contained with in the co-phenylcaine spray used for nasal airway topicalisation?
- 2.5 ml of co-phenylcaine contains 125mg of lidocaine and 12.5mg of phenylephrine which is your vasoconstrictor.
- Each spray is 100 microlitres and therefore delivers 5mg of lidocaine and 0.5mg of phenylephrine.
Question 5
According to the 2020 Difficult Airway Society or DAS guidelines for awake fibre-optic intubation, what are two options available for sedation?
Here you have a few options to choose from:
- Remifentanil can be used as a TCI or target controlled infusion using the Minto model, aiming for an effect site concentration of between 1 and 3 ng/ml
- Propofol can be used as a TCI infusion as well, but remember not as a bolus as you’ll likely drop the patient into too deep a plane of anaesthesia and risk apnoea, which we’re trying to avoid
- Dexmedetomidine
- Midazolam 0.5-1mg if there is a second anaesthetist present to help
Question 6
After insertion of the endotracheal tube, what methods can be used to ensure correct tube placement?
- Hopefully you saw the cords, tracheal rings and carina with your scope during the procedure, which acts as your first source of reassurance that you’re in the right place
- Clearly your end tidal CO2 capnography trace is going to be your gold standard here, but you should also
- Auscultate for breath sounds and ensure there is equal bilateral air entry
- Check for misting of the tube and angle piece
- You can then use a direct or video laryngoscope after intubation to assess the difficulty of the airway, and check your tube position as well
Question 7
List five complications of an awake fibre-optic intubation
So here we have four categories of things that can go wrong:
- Over sedation, leading to vomiting, aspiration, and loss of the airway
- Topicalisation, which can lead to local anaesthetic toxicity, anaphylaxis if allergic, or pain and distress if insufficient
- Hypoventilation, as a result of opioid use or airway obstruction, leading to hypercapnoea and hypoxia
- Performance: Failure to perform the procedure, bleeding and trauma to the airways, perforation of the cuff, oesophageal intubation and mucus plugging
Summary and Feedback
Here the aim of the question is to be able to confidently describe the anatomy relating to an awake fibre-optic intubation, as well as the complications that can be associated with it’s placement, and the pass requiremetn is to correctly identify the complications of an awake fibre-optic intubation.
Awake fibre-optic intubation needs to be one of those tools you keep in your back pocket for a predictably difficult airway. The recent guidelines from the difficult airway society or DAS in 202 have made an effort to standardise the procedure, and as with any invasive procedure, you’ll want to have a solid understanding of the anatomy you’re going to encounter, not only because the RCOA love to grill you on it, but also because the safety of the patient is rather important too, we probably shouldn’t forget that.
How would you prepare for safe extubation?
- Airway equipment ready for reintubation
- Extubate in theatre with trained assistant
- Appropriate anaesthetic drugs drawn up
- Surgical team remain in theatre until successful extubation
- Close observation in theatre prior to transfer to recovery
A final thought
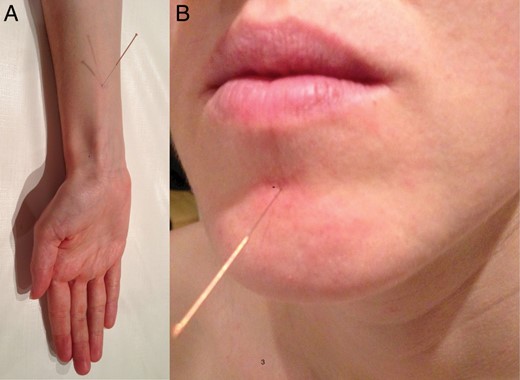
Why do these patients have acupuncture needles in these specific places?
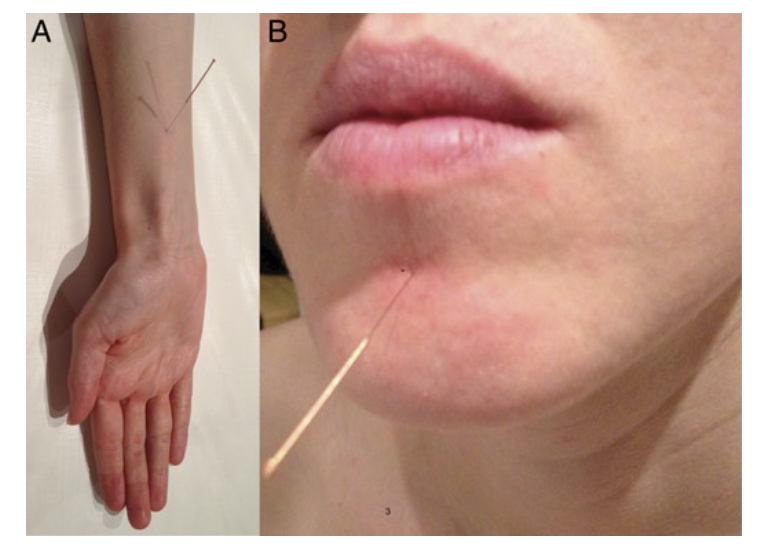
These are the specific Acupuncture points PC 6 and CV 24, which have anecdotally been described to reduce the gag reflex in patients having dental procedures.
While the evidence isn't overly convincing, it might be a useful (or at least interesting) adjunct for your particularly sensitive patients, or those with the dreaded local anaesthetic allergy that we talk about in exams so often...
Useful Tweets and Resources
If you don't already follow the #JanuAIRWAY masterpiece below - we'd highly recommend it.
Welcome back to #JanuAIRWAY! Today we’re looking at awake tracheal intubation. Here’s some #OnePagers on ergonomics and equipment to get things started… 1/4 pic.twitter.com/osED745sVQ
— Difficult Airway Society (DAS) Trainees (@dastrainees) January 14, 2023
Airway burns
If you don't know what a burnt airway looks like...
Chemical ingestion ( Air way burn )
— Mohammed Alsubaie (@sub3oon) August 5, 2022
Awake intubation.@EM_RESUS pic.twitter.com/KvVBtPyvUA
The Macewen article (1880) mentioned on 6/13/22 is a case series describing awake intubation of patients with partial glottic obstruction. Image: first page of the article. The 4th patient died during the procedure. Macewen's idea was not repeated by other physicians at the time. pic.twitter.com/WrJrRmprUD
— Merlin Larson, MD (@MerlinLarsonMD1) June 20, 2022
DAS Intubation guidelines
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
