Amniotic Fluid Embolism

Take home messages
- Amniotic fluid embolism remains a significant cause of maternal mortality
- Consider it when faced with sudden unexplained peripartum hypotension
- Classically one sees a hypoxic mixed respiratory and metabolic acidosis
Obstetrics just isn't stressful enough
It's 3am and the decision to operate is being made by a baby that is currently inside another human. You get the bleep telling you that said baby needs to be outside of the other human within the next 15-20 minutes please.
You then have to draw up a concoction of blisteringly powerful drugs and blindly thread a needle into a 35mm gap in an understandably-less-than-pleased pregnant woman's back, while three different specialties and the partner of said woman all watch.
But hey, at least once the spinal's in you can chill out right?
Wrong.
In 1926 at the University of São Paulo, J. R. Meyer first documented the diagnosis of amniotic fluid embolism, after a young parturient died from what looked like a pulmonary embolus, until they studied the pulmonary vasculature at autopsy and found amniotic fluid, foetal cells and hair.
It can happen at any time before, during or after delivery, and you need to know about it.
Enter amniotic fluid embolism
We'll start with two quotes:
- The first is from Doke Uyeno (1919) who described the constitution of amniotic fluid as follows:
"The amniotic fluid is slimy, yellowish white or pale yellow, and cloudy like soap water (rarely clear); it almost always contains much mucous flocks and has a peculiar odor."
- The second is from Dr Alex Yartsev of Deranged Physiology
"So, a volume of this material entering the circulation can mean only the most disastrous of consequences, being equivalent to the intravenous injection of sewer water."
There are - as you might imagine - a wide variety of ways in which amniotic fluid embolism can present, but two things are always present:
- Hypotension
- Foetal distress
The case reports are all fairly similar in nature - unsurprisingly it's usually a fairly fit and well young pregnant woman in the immediately peri-partum period who suddenly becomes catastrophically unwell.
The classic description is a very sudden deterioration in blood pressure and foetal distress, with breathlessness, lightheadedness and cyanosis followed quickly by unconsciousness and cardiac arrest.
The problem is that when it does happen, there's often other stuff happening at the same time, like an epidural or a caesarean etc, so it's very easy to mistake AFE for local anaesthetic toxicity, pulmonary embolism or major haemorrhage.
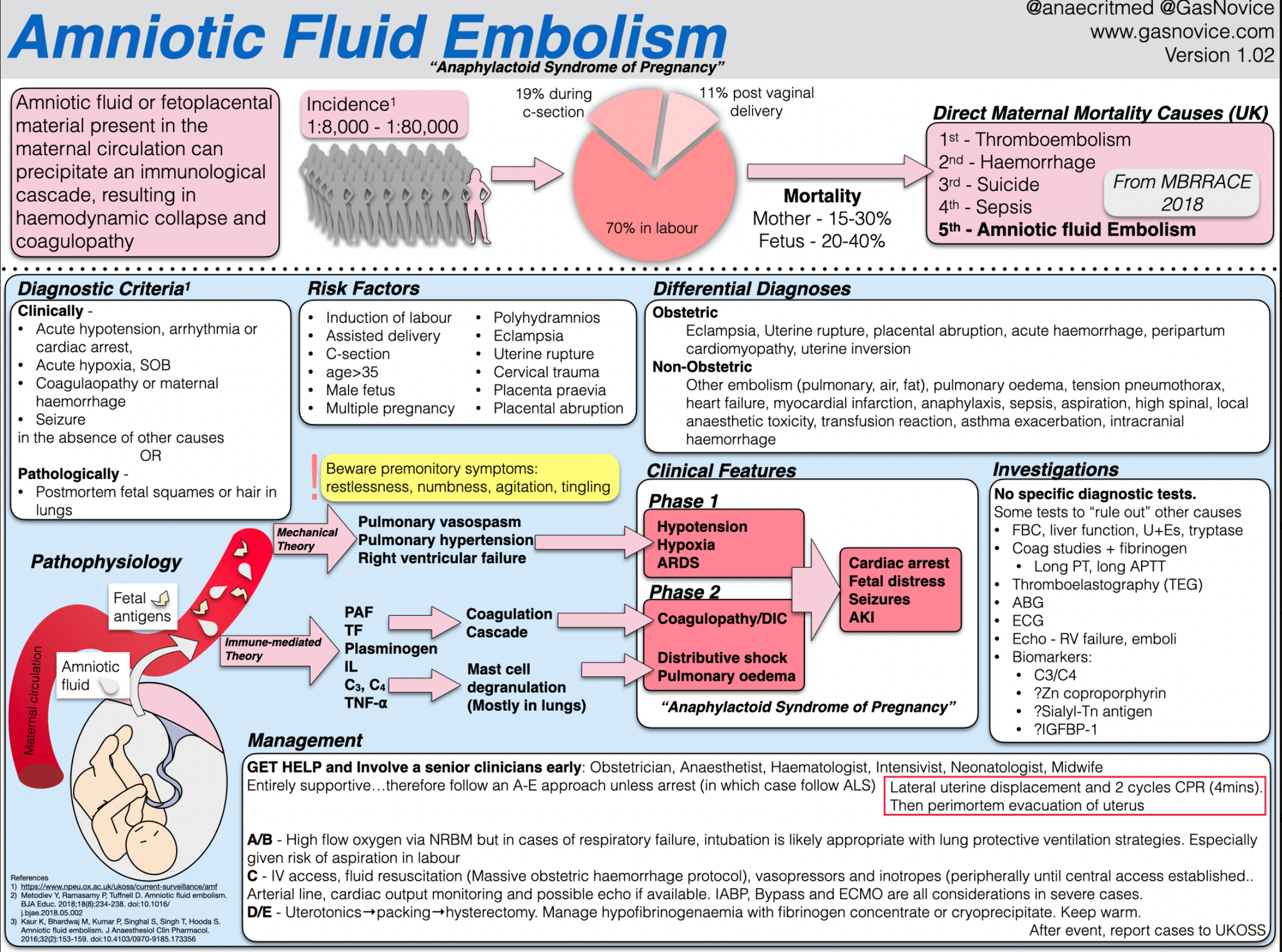
What are the four cardinal features of AFE?
- Respiratory distress
- Cyanosis
- Cardiovascular collapse
- Coma
There are also no specific diagnostic tests*, and given the management is largely just 'supportive critical care', you might as well assume the worst and crack on.
*If you're not busy doing something else (like resuscitating a parturient mother) then you could test her blood for zinc coproporphyrin, which is known to be a component of meconium, or Sialyl-Tn antigen (found in amniotic fluid) but you probably have other stuff to deal with right now.
So what happens?
Much like fat embolism syndrome, we don't really know.
There are two suggested pathophysiological mechanisms:
- Mechanical
- Immunological
As is often the case when we have two competing theories - neither does a complete job of explaining the situation on their own, but together they probably cover it.
Mechanical theory
- Amniotic fluid and all of its lovely contents (foetal squamous cells, vernix, lanugo and the like) enter the maternal circulation as an embolus*
- This gets lodged in the lungs like a ruptured DVT-turned-PE
- This results in sudden onset pulmonary hypertension and right ventricular failure leading to hypotension and collapse
*A sudden deep inwards breath in a dehydrated parturient could generate sufficient negative intrathoracic pressure to briefly make the venous pressure negative enough to 'suck' amniotic fluid along for the ride.
Combine this with massively positive intrauterine pressure during violent contractions and it's entirely reasonable to expect that amniotic fluid be shoved into the vasculature.
Immunological theory
- Uterine or placental trauma brings amntiotic fluid into contact with maternal blood
- Foetal antigens enter maternal blood (platelet-activating factor, interleukins, tumour necrosis factor-alpha)
- This triggers mast cell degranulation either directly or via complement activation*
- This leads to pulmonary vasoconstriction and hypertension due to release of arachidonic acid, prostaglandins and leukotrienes
- These antigens also trigger the clotting cascade and can lead to DIC
*You don't see a tryptase rise as in anaphylaxis, but this might be because the majority of the degranulation is in the lungs and therefore not picked up by blood tests done on the systemic circulation.
There are also two proposed phases of the condition:
- Phase 1 - amniotic fluid and its various contents enter the pulmonary circulation and trigger an increase in pulmonary arterial pressure and right ventricular failure, worsening by microthrombi formation
- Phase 2 - if the patient survives phase 1 then they can go on to develop left ventricular failure, endothelial dysfunction and disseminated intravascular coagulation
What are the contents of amniotic fluid?
- Fetal squamous cells
- Vernix
- Lanugo hair
- Trophoblasts
- Mucin from the foetal GI tract
- Meconium and bile
It therefore makes sense that there might be an element of an anaphalactoid reaction if this cocktail enters the maternal bloodstream.
How bad is it?
Bad.
But we're not really sure exactly how bad.
It has the tricky characteristics of being both deadly and rare, making it rather tricky to study in research trials with any real power.
When does it happen?
- 70% in labour
- 19% during C-section
- 11% immediately post-partum
What are the generally accepted risk factors for amniotic fluid embolism?
- Age greater than 25 years
- History of atopy
- Multiparous
- Chorioamnionitis
- Rapid labour
- Obstructed labor
- Use of oxytocics
- Meconium
- Polyhydraminios
- Maternal history of allergy or atopy
- Placental abruption
- Uterine rupture
- Intra-uterine foetal demise
What are the signs and symptoms of AFE?
- Hypotension - 100%
- Foetal distress - 100%
- ARDS/pulmonary oedema - >90%
- Cardiac arrest - >80%
- Coagulopathy - >80%
- Cyanosis - >80%
- Seizures
- Dyspnoea
What factors contribute to the hypoxia seen in amniotic fluid embolism?
- VQ mismatch
- Pulmonary oedema (both cardiogenic and due to capillary leak)
- Bronchospasm
Management
So what do I do?
- Call for help - more anaesthetists, obstetricians, ICU, paediatricians and a haematologist
Resuscitation and supportive care as for any sudden deterioration:
Airway
- Intubate if cardiac arrest
- RSI if airway or respiratory compromise
Breathing
- 100% oxygen
- PEEP for left heart failure
- Inhaled nitric oxide and prostacyclin have been used to counter pulmonary vasoconstriction
Circulation
- Big IV or IO access
- Fluids
- Vasopressors and inotropes (peripheral followed by central once available)
- Arterial line
- Echocardiography is a good idea
- Manual lateral displacement of the uterus
- Resuscitative hysterotomy and delivery of the foetus at four minutes if cardiac arrest
- ECMO, bypass and IABP have all been described as options where available
- Manage haemorrhage and coagulopathy
Haematological
- Early activation of major haemorrhage protocol
- Antifibrinolytics (tranexamic acid)
- TEG/ROTEM guided management of hypofibrinogenaemia
General
- ICU admission
Useful Tweets and Resources
Check out this amazing infographic by Chris Hellyar over at gasnovice.com
🚨#POCUS #echofirst image of the day:
— NephroPOCUS (@NephroP) January 18, 2023
Right ventricular dysfunction and McConnell's sign in a patient with amniotic fluid embolism.
🔗https://t.co/goeNYc8foL#MedEd #IMPOCUS #FOAMcc pic.twitter.com/i9Nm8QDmEq
References and Further Reading

Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.