Ventilator Modes

Ventilation is a breathtakingly large subject, so this post is merely an introduction to the specific modes we use, and what they mean.
But fear not - many more ventilator posts will follow.
Ventilators are simple
Well, in principle at least, as they serve one main function:
- Push gas into the lungs, and then let it out again
Now, the nuance lies in exactly how the ventilator does this, and to truly understand what we're talking about, we need to break down what a 'breath' actually entails.
The steps of a breath
Whether a patient is awake and breathing spontaneously, or intubated and entirely dependent on the ventilator, one would generally agree that the following broad steps need to happen for said patient not to asphyxiate.
- Inspiration is initiated
- A pressure gradient is generated
- Gas moves down this pressure gradient into the lungs
- Gas continues to move until the intrathoracic and atmospheric pressures equalise, and the gradient drops to zero
- Expiration is initiated
- A pressure gradient is generated
- Gas moves down this pressure gradient out of the lungs
- Gas continues to move until the pressures equalise once more
- The cycle repeats
These steps can be categorised into the four phases of the ventilatory cycle.
What are the four phases of a breath?
- Initiation
- Inspiratory phase
- Plateau phase (or inspiratory pause)
- Expiratory phase
Each of these has a parameter or variable that influences how it starts, how it stops and what happens in between.
As you can see, there are a few variables here that we can potentially fiddle with.
So what can we control?
If the patient is breathing by themselves in the emergency department with a facemask or nasal cannula, then there is very little that we can take control of here, and it's frankly extremely uncomfortable to be letting laypeople perform such an important task by themselves.
But apparently they seem to be quite good at it.
If, however, we have made the decision to take total control, by pharmacologically removing their ability to breathe and plugging them into our glorious machine then we have a whole host of parameters to play with and buttons to press.
There are then the nuanced scenarios where the patient is a bit in charge, with a ventilator helping out - we'll talk about them a bit later on.
For now, we'll get to grips with the basics by assuming our patient is doing nothing at all, and we have to do all the work with our ventilator.
Let's start with pressure and volume.
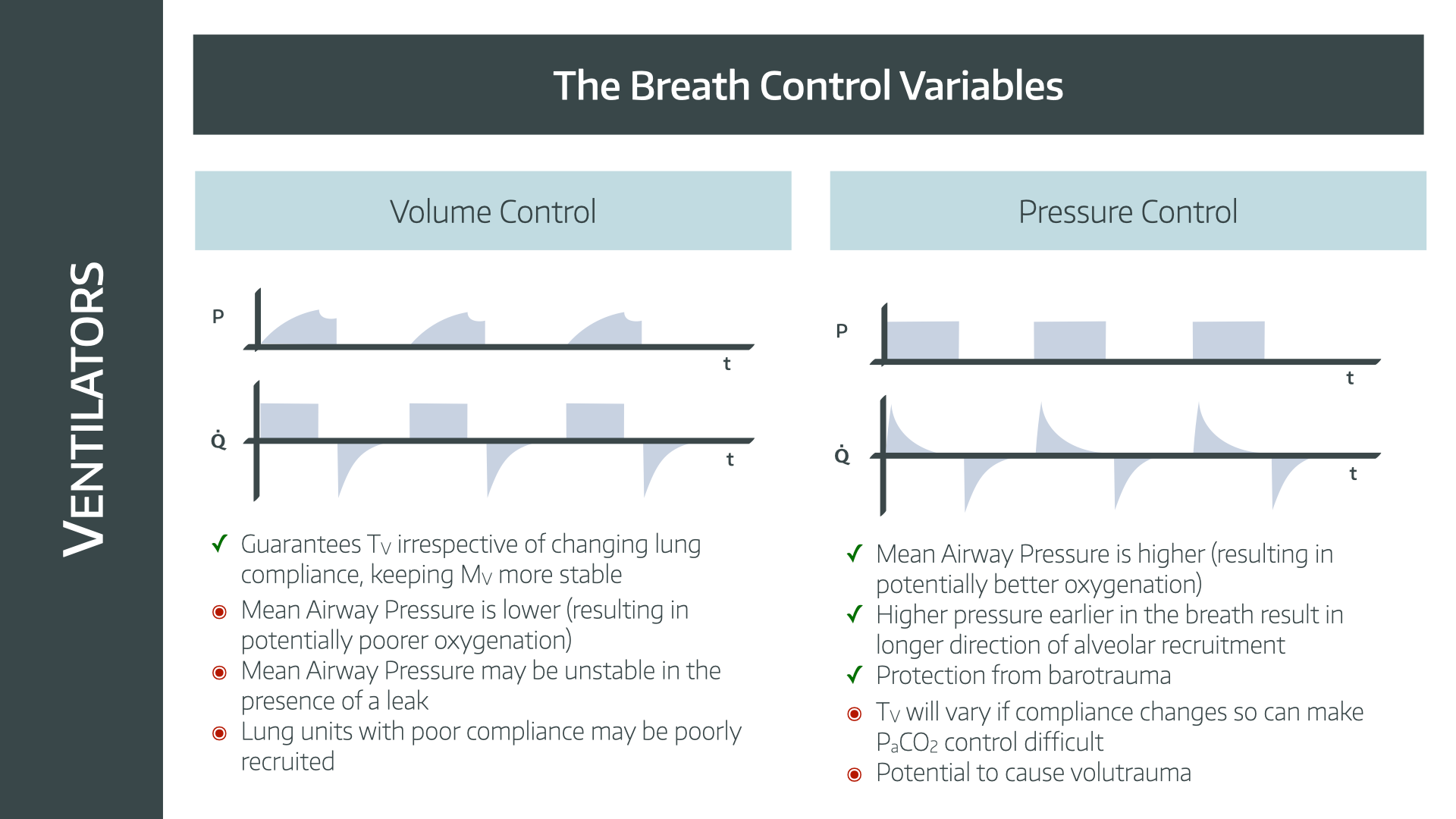
Pressure and Volume control
Earlier we mentioned generating a pressure gradient to encourage molecules of fresh gas into our patient's lungs.
- When breathing spontaneously, this gradient is generated by creating negative pressure in the thorax
- When ventilated, we usually used positive pressure
- Negative pressure ventilators do exist, but you probably won't be using them any time soon
So the ventilator will apply positive pressure at its end of the breathing tubing, greater than the intrathoracic pressure of the patient, and voila - a gradient appears and molecules move.
But how does it know how much pressure to apply and how long to apply it for?
Well we're going to tell it, with either volume control or pressure control.
Volume control
- You tell the ventilator to apply sufficient pressure such that a set volume of gas is delivered to the patient
- Once this volume has been delivered, the pressure is released
- It will release this pressure not all the way to zero, but to a lower pressure level designed to hold the alveoli open
- This is the positive end expiratory pressure or PEEP
- It will then wait for a bit (you tell it how long)
- Then it will start again
This mode will attempt to deliver the set tidal volume, and will push harder in order to achieve it, which can risk pressure damage in stiff lungs (barotrauma).
You control:
- Tidal volume
- PEEP
- Respiratory rate
You don't control:
- Inspiratory pressures (but you can set safety limits)
Pressure control
- You tell the ventilator to apply a certain amount of pressure, for a certain amount of time
- This is the inspiratory pressure
- It will then release this pressure down to the PEEP, exactly as above
- It will then wait for a bit (you tell it how long)
- Then it will start again
It will never apply more pressure than you tell it, meaning there is less chance of damaging the lung with excessive pressure (barotrauma).
However you have no guarantee of an adequate tidal volume, so you have to monitor what volumes you are achieving, and adjust your settings accordingly.
You control:
- Inspiratory pressure
- PEEP
- Respiratory rate
You don't control:
- Tidal volume
Literally every ventilator mode on the planet falls into these two categories, or combines aspects of both, so it makes sense as a good place to start.
If you know nothing more than this, then you still know a lot more than most.
However if you want to join us in the details, read on.
Triggers, cycles and limits
So we've told the ventilator how to deliver a breath, and how frequently, but there are many other questions that our machine has of us:
- When should I start delivering a breath?
- When should I stop delivering a breath?
- How long should I allow the patient to exhale for?
- What if the patient wants to breath by themselves?
And that's where triggering, cycling and limiting come into play.
Triggering
What triggers the ventilator to deliver a breath?
Think about what the ventilator is capable of detecting, and measuring:
- Time
- Pressure
- Flow
- Volume
Time is the trigger in mandatory modes, as the ventilator decides when the next breath is going to start.
For the other three, the patient is initiating the breath, and the ventilator is responding to either an increase in flow, a drop in pressure or a set volume to have been sucked in by the patient.
Cycling
How does the ventilator decide to switch from inspiration to exhalation?
There are again the same four options:
- Volume cycling - switch to exhalation after set volume delivered
- Time cycling - switch after a set length of time
- Pressure cycling - switch once a set pressure is reached
- Flow cycling - switch once a set flow rate is reached
Which one your ventilator is going to use is going to depend on the mode you've settled on.
Limit
What is the main parameter that you control?
- Pressure
- Volume
- Flow (older, less commonly used mode)
This is essentially what we talked about at the start - which bit do you control, and which bit do you allow to fluctuate?
Cycling is what tells the ventilator to stop inspiration.
So to describe VCV and PCV in their full terminology, one might say...
Volume controlled ventilation
- Trigger = Time
- Cycling = Time
- Limit = flow or volume
Volume controlled ventilation is a volume-targeted, time-triggered, time-cycled mode, where the pressures generated will depend on lung compliance.
Pressure controlled ventilation
- Trigger = Time
- Cycling = Time
- Limit = Pressure
Pressure controlled ventilation is a pressure-targeted, time-triggered, time-cycled mode, where the tidal volume will depend on lung compliance
What if the patient is spontaneously breathing?
Excellent question, and the answer is simple - all of the previous points still apply, there's just a smidge of nuanced negotiation between man and machine.
Who's in charge of what?
Well it's fairly obvious that in a fully spontaneously breathing patient, the patient is in charge of all four phases of the breath, and therefore the trigger, the cycle and the limit.
Likewise if they're on fully mandatory ventilation, then the ventilator is deciding instead.
But we run into an issue if the ventilator is trying to do one thing and the patient another - this is called dyssynchrony and makes for terrible gas exchange and can lead to all sorts of other pulmonary problems.
Therefore there are in-between modes where the human and the ventilator must dance a respiratory waltz and figure out how to work together, called assisted and supported modes.
In short:
- In assisted modes, the patient will trigger a breath, but the ventilator does the rest
- In supported modes, the patient will trigger a breath and decide when to stop (cycle), but the ventilator will be able to stop a breath early (limit) if needed (e.g. too slow or too large an inspiration)
So in summary:
| Type | Trigger | Cycle | Limit |
|---|---|---|---|
| Mandatory | Ventilator | Ventilator | Ventilator |
| Assisted | Patient | Ventilator | Ventilator |
| Supported | Patient | Patient | Ventilator |
| Spontaneous | Patient | Patient | Ventilator |
This means they will allow the patient to trigger the breath, and provide whatever support they've been programmed to give (usually a set pressure).
Then they will wait patiently for the flow to drop to some pre-determined parameter, such as 25% of the highest flow rate during the breath, at which point they will say enough's enough and cycle into the expiratory phase.
Pressure support ventilation
- Trigger = Patient
- Cycling = Flow
- Limit = Pressure
Pressure support ventilation is a pressure-targeted, patient-triggered, flow-cycled mode, where the tidal volume will depend on lung compliance
"I get it, pressure support is kind of an intubated version of BiPAP, where the patient is breathing but getting some extra help."
Precisely.
"But what if I give a load of morphine and they stop breathing for a bit?"
Ah then you probably want to use a different mode like SIMV.
"Huh?"
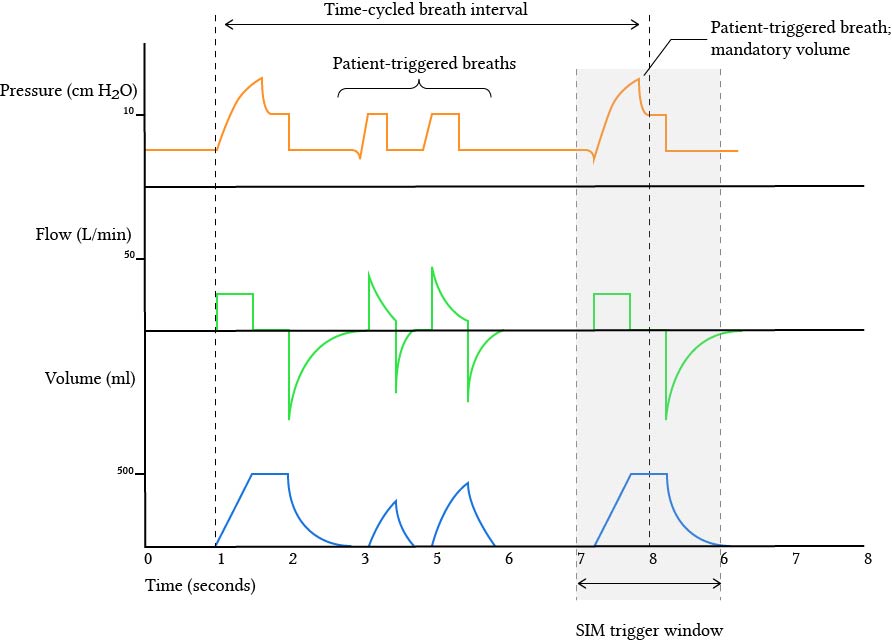
Okay so what the hell is SIMV?
Now we're talking.
Synchronised intermittent mandatory ventilation is a hybrid mode that aims to combine the best bits of both support and mandatory ventilation.
The aim is to allow the patient to take some assisted breaths if they want to (which pure VCV and PCV don't), but also to ensure the patient will get some mandatory breaths if they decide that breathing is for the weak and they're having none of it (which PSV doesn't).
The key points are as follows:
- You tell the ventilator to give a set minimum number of breaths per minute
- These can be volume or pressure controlled but they're mandatory either way
- If the patient wants to take additional breaths in between, the ventilator will help by giving some pressure support
- The ventilator will then also synchronise with the patient's breaths, to avoid delivering the next scheduled mandatory breath half way through a spontaneous one
Simples.
SIMV
- Trigger = Time or patient
- Cycling = Time
- Limit = Volume or pressure
What settings do you control with SIMV?
- Minimum respiratory rate (but you can't stop the patient breathing more frequently if they want to)
- Tidal volume or inspiratory pressure depending on whether VCV or PCV
- PEEP
- FiO2
- Pressure support*
*This is how much pressure the ventilator gives to the patient for the spontaneous extra breaths they decide to take.
So what is SCMV?
Welcome, welcome, take a seat.
Synchronised controlled mandatory ventilation.
Hamilton call this SCMV, Drager call it VC-AC, GE call it A/C VC
It doesn't matter what it's called, what matters is that it's basically the same as SIMV, but instead of supporting those extra breaths that the patient decides to take (by applying a bit of pressure), these breaths are now controlled.
- The ventilator has a set minimum rate of mandatory breaths, same as with SIMV
- The patient can also take extra breaths, just like SIMV
- If the patient does take an extra breath, the ventilator will give a mandatory breath, whether the patient likes it or not
- It will then synchronise the next scheduled breath to avoid double stacking breaths, just like SIMV
- So all of the breaths are the same, mandatory, ventilator controlled breaths, but the patient gets to adjust the rate
The only difference is what the ventilator does with the extra breaths - support or control.
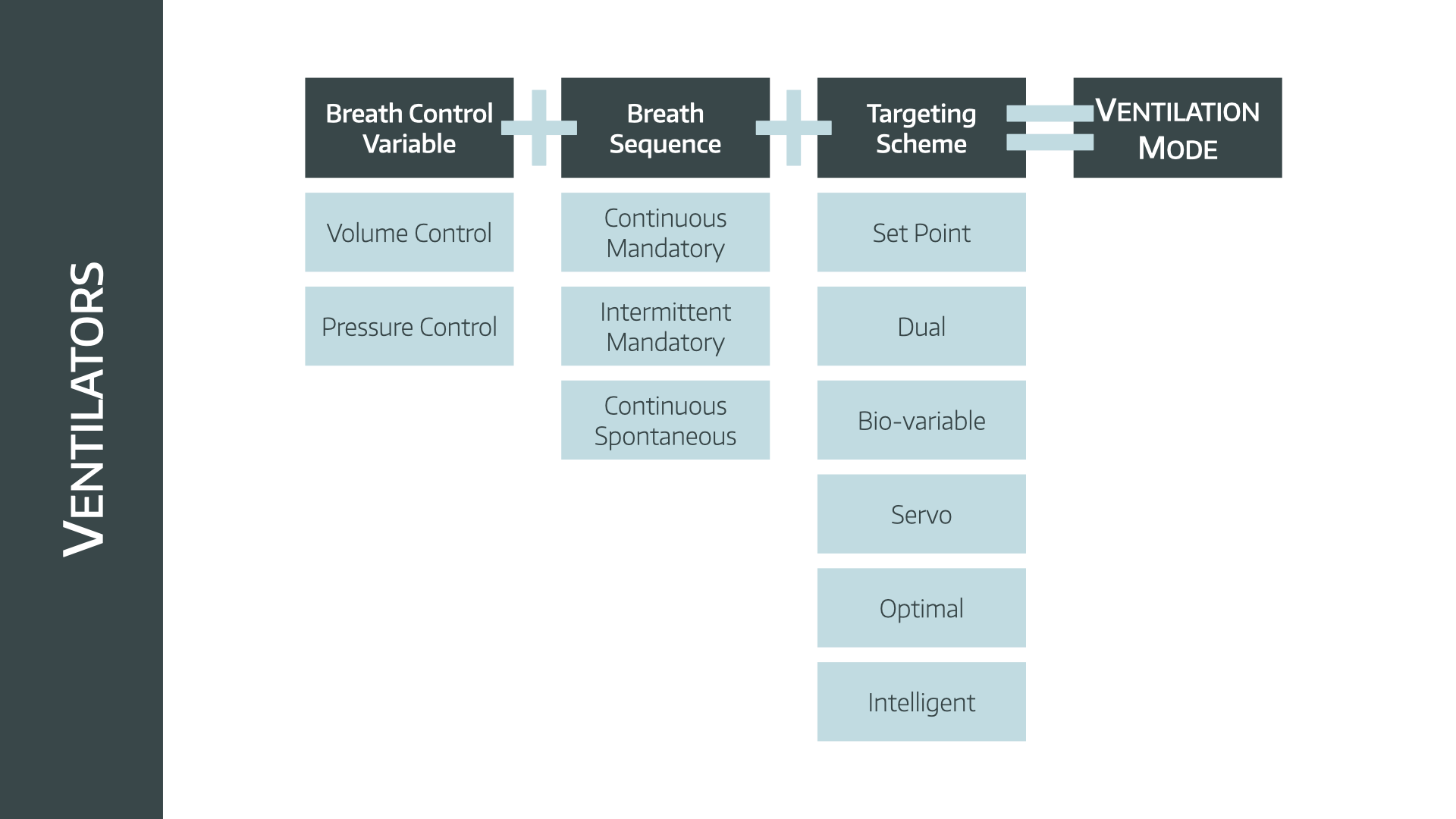
Then you can get even smarter
Up until this point, we've just told the ventilator some rudimentary targets to aim for and allowed it to measure only a few parameters:
- Volume
- Flow
- Time
- Pressure
This is what we call a set point target, and it's the simplest way to ventilate someone.
The ventilator will keep doing what you've set it to do, hopefully achieving those targets, regardless of the patient's other parameters.
But here's a fun idea, what if we let it measure a bunch of other stuff too, and then it can adjust itself to optimise the patient even further?
Enter targeting and adaptive ventilation
This is the last thing I promise.
Set point
What we just mentioned - you give a set number to achieve, and the ventilator does its merry best to make it happen.
- Pressure for PCV
- Tidal volume for VCV
Dual targeting
The ventilator switches to a different target halfway through a breath.
- It might start off with a set pressure target
- It might then hit that pressure half way through the breath
- Then switch to a volume target for the rest of the breath instead
Not used a whole lot anymore.
Servo control
This is where it gets quite cool.
You add in some other signal that the ventilator can measure, and then adapt how it helps to the patient's need.
For example, if you measure with a diaphragmatic EMG, you can tell the ventilator when the patient is initiating a breath (without having to wait until it detects a change in flow) and you can say how hard the patient is trying, and therefore how much help to give.
Very cool, rarely examined.
Adaptive targeting
This is much more commonly used, especially on ICU with newer ventilators.
An example would be the pressure-controlled, volume-guaranteed (PC-VG) mode (which is the best to use in theatre by the way).
- The ventilator gives a test breath to assess lung compliance
- It then works out the lowest pressure required to hit the target tidal volume
- It then uses pressure control to achieve that volume
- If compliance changes, it reassesses, and adapts the pressure as needed
It is:
- Time-triggered
- Time-cycled
- Pressure-limited
- Volume-targeted
Optimal targeting
This is just the next level up from adaptive.
As well as being adaptive as described above, optimal allows you to put in more information such as the patient's height and weight.
The ventilator then calculates the ideal targeting scheme for that individual patient, based on compliance, volume, pressure... etc
You get the idea.
Bio-variable
This is a weird one you don't really need to know much about, other than that the ventilator deliberately throws in a bit of randomness and variation, because 'that's what spontaneously breathing people do.'
Not every breath is quite the same, and it seems to help with VQ matching and gas exchange.
Intelligent targeting
The big boss of ICU ventilation, and basically just a better version of optimal with even more data.
- User sets ideal body weight, height, and whatever other data it asks for
- The ventilator then targets an optimal minute ventilation and adapts rate, pressure and tidal volume to lung mechanics
- Adjusts breath-by-breath.
- Can also have EtCO2 and oxygen saturation feedback loops
- Automatically adjusts FiO₂, PEEP, and other ventilation settings to meet oxygenation and ventilation targets
- Very effective for automatic weaning*
*When it works.
Finished
If you take all of the above ideas and cram them into one equation, it looks like this.
There, we're done.
Promise.
I'm a novice, just give me some sensible numbers to start with.
In the unlikely event that you've intubated a patient as a novice with zero senior guidance and are now stuck with the task of initiating the ventilator with no help at all, then start here:
- Pressure Control Ventilation
- Inspiratory pressure- 15cmH2O
- PEEP - 5cmH2O
- Adjust the inspiratory pressure to get a tidal volume of 6-10 ml/kg
- Adjust the respiratory rate to get an end tidal CO2 of 4.5-5.5 kPa
Then we'd heavily suggest getting some sort of senior input rather promptly.
A challenge for you
Go to this webpage and see if any of the ventilator modes make any more sense than before you read this post.



Useful Resources
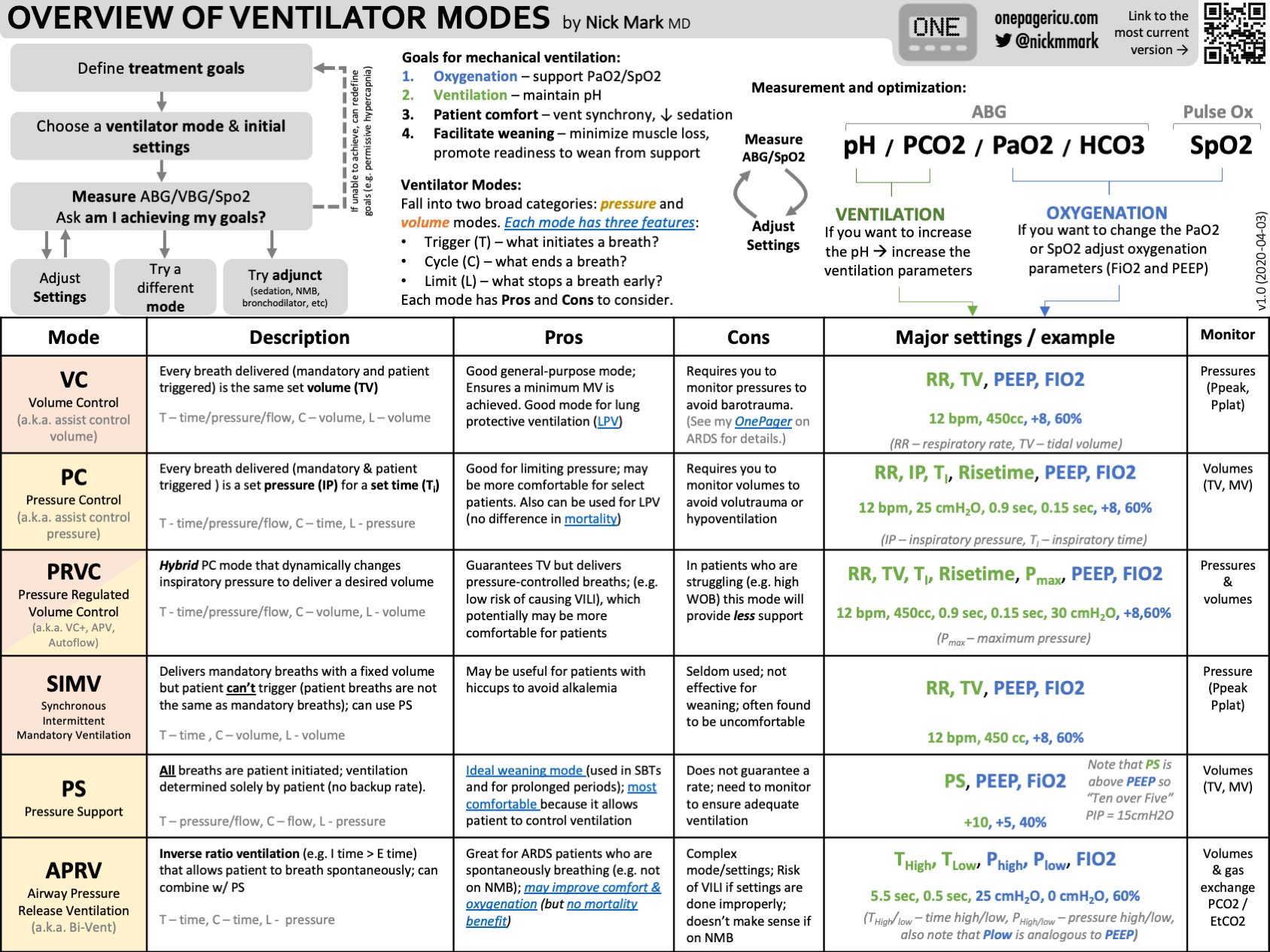
Here's a spectacular one page summary from onepagericu.com
@anaestheasier Replying to @lloveoakley123 ventilation modes and avaps
♬ original sound - Anaestheasier
References and Further Reading
Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.