The Cardiac Action Potential
Take home messages:
- The heart is really cool
- The three main players in conduction of cardiac action potentials - and therefore the main targets of antiarrhythmic drugs - are sodium, potassium and calcium
- The pacemaker cells have an inherently unstable resting membrane potential, whilst contractile myocytes have a stable membrane potiental
The cardiac action potential is unique
The cardiac action potential has a prolonged plateau phase lasting around 300 ms, far longer than 1 ms in nerves.
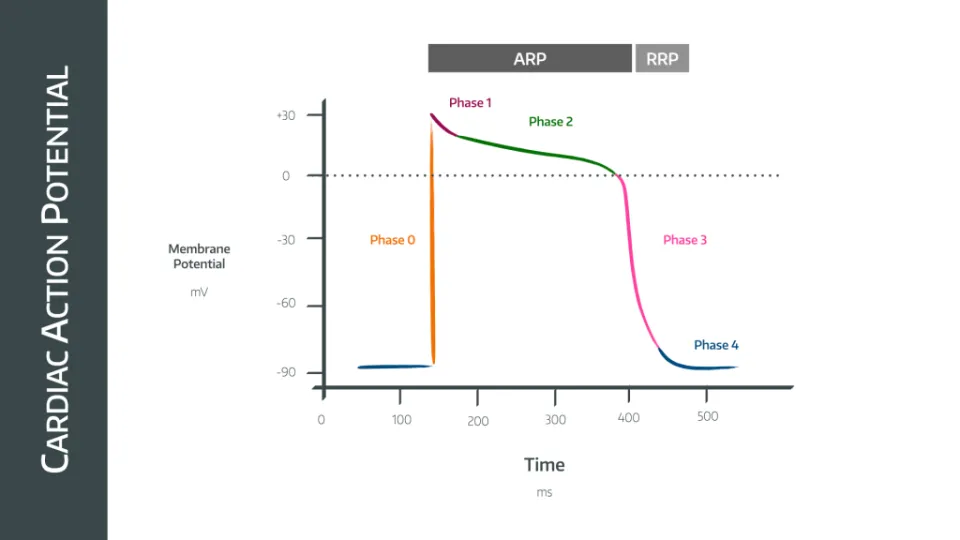
When describing cardiac action potentials, there are 5 phases, numbered 0 to 4.
The Pacemaker Potential
The main pacemaker for the heart is the sinoatrial node, as it has the highest rate of spontaneous depolarization, trying to depolarise at around 100 beats per minute. The reason the average resting heart rate is lower than this is because of vagal tone, which slows the heart rate down.
In a denervated (transplanted) heart, we see a faster resting heart rate because there is no vagal innervation to the heart.
It therefore suppresses the action of the other pacemakers.
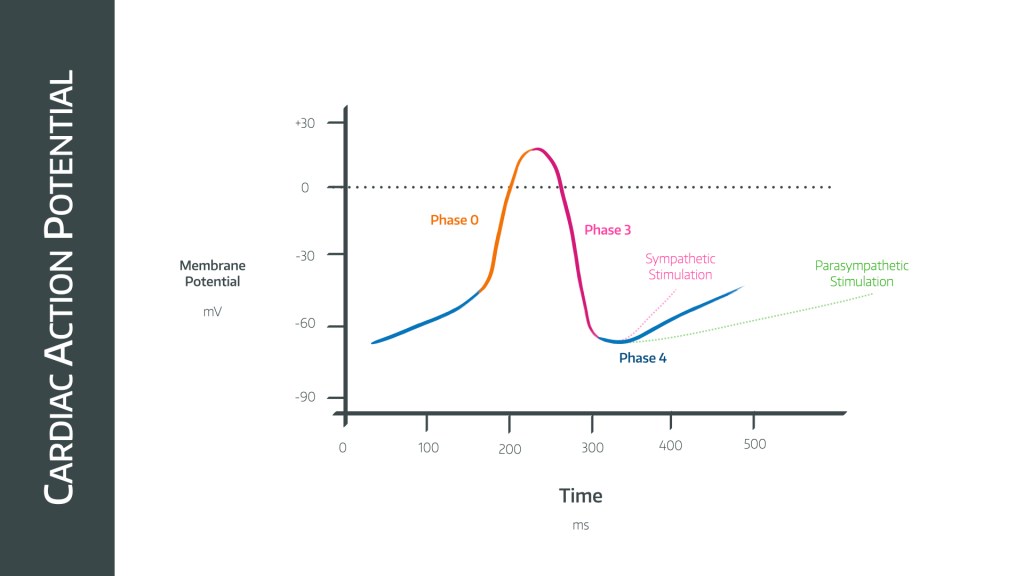
The pacemaker potential is the automated, rhythmic depolarisation of the sinoatrial node cells that provide the heart with its intrinsic rhythm.
It only has phases 0, 3 and 4
Phase 0
- Depolarisation
- Triggered at -40mV
- Slow L-type calcium channels allow slow calcium ingress into the cell
Phase 3
- Repolarisation
- Calcium channels close
- Potassium channels open
Phase 4
- Transient ‘overshoot’ hyperpolarisation reaching maximum diastolic potential of -65mV
- Potassium channels close
There is then a process of gradual depolarisation until the threshold potential is met, due to:
- Sodium ion leak
- T Type calcium channels allowing calcium in
- Sodium-calcium pump
Sympathetic and parasympathetic stimultion cause the gradient of phase 4 to be steeper and shallower respectively
The Cardiac Action Potential
This is the main action potential that propagates through the bulk of the myocardium.
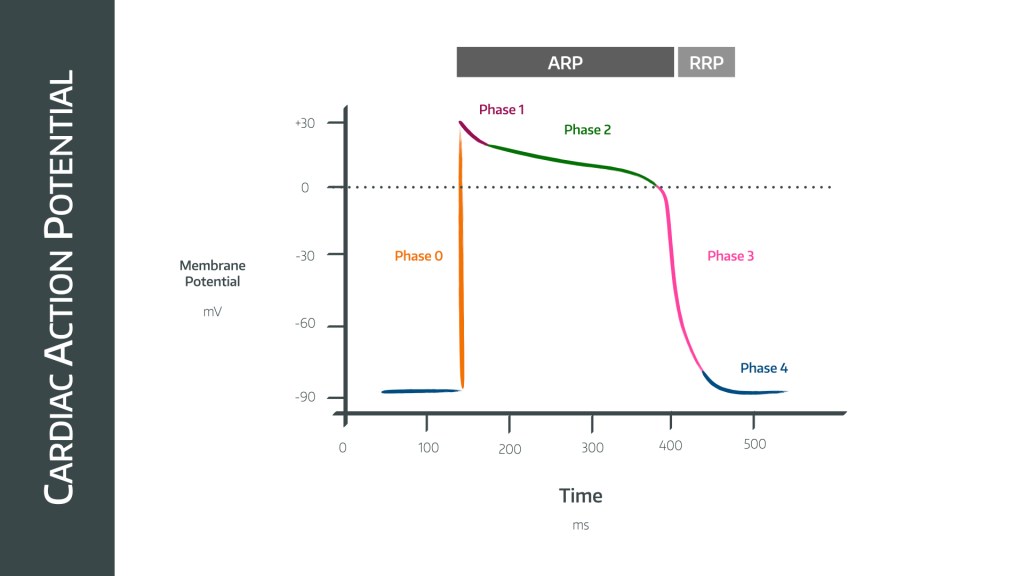
The trace of the action potential seen in cardiac myocytes is different to pacemaker cells, as rather than being rhythm generators, they use the action potential to generate a sustained contraction during systole.
As mentioned above, there are five phases to the cardiac action potential, labelled 0 to 4
Phase 0
- Rapid depolarisation
- Fast sodium channels
Phase 1
- Repolarisation (short)
- Sodium channels close
- Potassium channels open
- Does not repolarise beyond zero mV
- Part of the absolute refractory period
Phase 2
- Plateau phase
- L type calcium channels allow calcium in to slow the process of repolarisation
- Part of absolute refractory period
Phase 3
- Repolarisation
- L type calcium channels close
- Potassium channels remain open, and potassium diffuses out
- Part of relative refractory period
Phase 4
- Na/K ATPase returns the membrane potential to baseline
- Part of relative refractory period
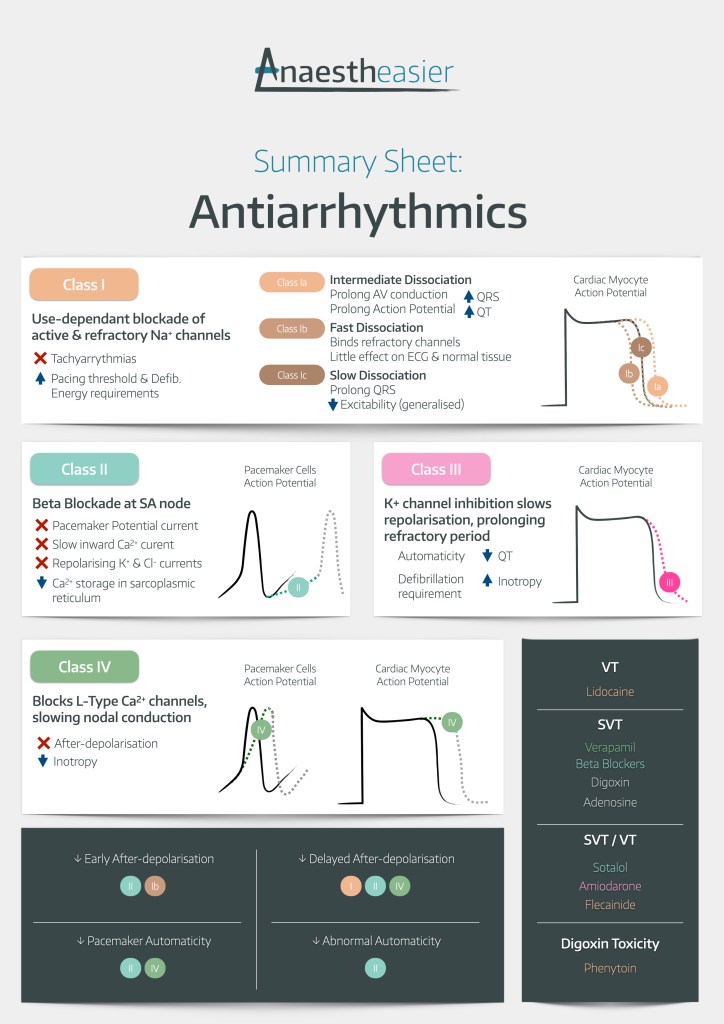
Which aspects of the cardiac action potential do each class of antiarrhythmic agent act on?
When we talk about class of antiarrhythmic agent, we usually refer to the Vaughn-Williams Classification, which we discuss here

Class 1 drugs
- These are membrane stabilisers
- They inhibit rapid influx of sodium ions during phase 0
- They also reduce the rate of depolarisation in phase 4, in pacemaker cells
- 1A prolong the refractory period, and act in the atria, ventricles and accessory pathways
- 1B shorten the refractory period, only acting in the ventricles
- 1C have no effect on the refractory period, acting in atria, ventricles and accessory pathways
Class 2 drugs
- These are beta blockers
- They inhibit sympathetic tone to the heart, and have three effects:
- Reduction of slope of phase 4 in pacemaker cells
- Reduction of maximum rate of depolarisation (Phase 0)
- Prolongation of the action potential duration
Class 3 drugs
- These are potassium channel antagonists
- They prolong the duration of the action potential and refractory period by slowing potassium efflux
Class 4 drugs
- These are calcium channel inhibitors
- They modify the plateau phase in non-pacemaker cells by acting on the L type calcium channels
- They also inhibit depolarisation in phase 0 of the pacemaker cells
Why do tachyarrhythmias occur?
- Increased automaticity of atrial or ventricular myocytes resulting in premature depolarisation before the sinoatrial node
- Can be triggered by anything that encourages the membrane potential to reach the threshold for depolarisation too quickly, such as ionic imbalance - particularly hypokalaemia - and ischaemia
- Re-entry tachyarrhythmias can occur if there is an ectopic focus and a conducting pathway that allows a circuit of repolarisation and depolarisation to occur
Why might a patient become bradycardic?
This could be a physiological response or a pathalogical conduction issue
Physiological response:
- Pneumoperitoneum
- Cervical dilatation
- Pressure on the eye
- Anaesthetic
- Laryngoscopy, particularly using a Miller blade in children
- The Miller blade lifts the underside of the epiglottis, which is innervated by the vagus, rather than the valleculae which are innervated by the glossopharyngeal nerve
Medications:
- Opioids
- Neostigmine
Conduction pathology:
- Failure of AV node to conduct atrial impulse to conducting system
- Type II or complete heart block
- MI
- Ischaemia
Antiarrhythmics summary sheet
Useful Tweets
For periodic processes, such as the #cardiac action potential, the concept of phase is useful. While the potential smoothly rises and falls between two states, the phase is monotonously increasing. An internal clock of each cell's routine. #mathematics @KU_Leuven @LUMC_Leiden pic.twitter.com/gneHVHJJaL
— Desmond Kabus (@mondkubus) April 8, 2022
A 23 y/o male comes into the ED on New Year's Day with chest pain, palpitations, and difficulty breathing. His ECG is below.
— Druv Bhagavan (@DruvBhagavan) January 1, 2023
After being shocked once, he recovers completely and is soon discharged.
What do you think happened? 🧐 (1/n) 🧵⬇️#MedTwitter #CardioTwitter #FOAMed pic.twitter.com/QBE5KO54KQ
Try our free Viva Practice Questions

Everything you need to pass the FRCA Primary

60% discount available to Anaestheasier members
References and Further Reading:
- Jeremy Pinnell, MB ChB FRCA, Simon Turner, BSc MB ChB FRCA, Simon Howell, MRCP FRCA MSc MD, Cardiac muscle physiology, Continuing Education in Anaesthesia Critical Care & Pain, Volume 7, Issue 3, June 2007, Pages 85–88, https://doi.org/10.1093/bjaceaccp/mkm013