Spinal Anaesthesia

Take home messages
- Spinal anaesthesia is literally magic
- It can be used for anaesthesia below the umbilicus or analgesia below the neck
- Pay attention to blood pressure, and use extreme caution in aortic stenosis
Podcast episode
A needle and a nerve
Ever since Karl Koller figured out that dripping cocaine into a frog's eye rendered it largely unfussed by then being jabbed in said eye with a needle, humans (mostly anaesthetists) have busied themselves with the honourable task of seeing just how many different nerves can be successfully anaesthetised with local anaesthetic.
One of the most successful and routinely used locations to stick one's needle, laced with something ending in '-aine', is the subarachnoid space in the spinal canal, with the unimaginative title of 'spinal anaesthesia'
A Spot of History
If you haven't yet heard of August Bier then allow me to introduce a no-longer-living legend.

Bier qualified in 1886 and went to on become Chief Surgeon at one of the largest European teaching hospitals called the Charité - Universitätsmedizin in Berlin. While working as a surgeon he became interested in seeking an alternative to general anaesthesia, and began experimenting by injecting cocaine into people's spines.
In 1898, 15mg intrathecal cocaine allowed him to perform foot and ankle surgery on a thirty-four year old man with horrific TB that had tracked to the bones in his foot, thus crowning him as first past the post for a successful operation under spinal anaesthesia*.
While the patient was awake, alive and comfortable throughout the operation, he unfortunately developed a stonking headache, vomiting, back pain and ankle pain soon thereafter.
Bier then later practised on himself and his assistant, and - by using an enormous needle with substantial loss of CSF during the procedure - successfully induced the first documented post-dural puncture headache as well.
If you'd like to read a little more about Bier's adventures with needles and the spine, click here for our history page.
*There is debate as to whether James Leonard Corning was actually first in 1885. Based on his documentation he might have done an epidural or a spinal, it's unclear. Given he injected eight times as much cocaine as Bier, with slower onset and a lower level of blockade, and didn't see any csf at the time - it's all sounding rather epidural. Either way, it wasn't for an operation, so Bier probably wins anyway.
How to do a spinal
As with any procedure in anaesthetics, or medicine as a whole, you can divide the process of performing a procedure into the following steps:
Set up and safety checks
- Confirm patient identity, capacity and informed consent, and check recent clotting and platelet results, as well as the last time any prophylactic or treatment anticoagulation given*
- Ensure full AAGBI monitoring and vasopressor emergency drugs available
- Assistant present and full sterile precautions
*Needs to be 12 hours after prophylactic dose, and 24 hours after treatment dose.
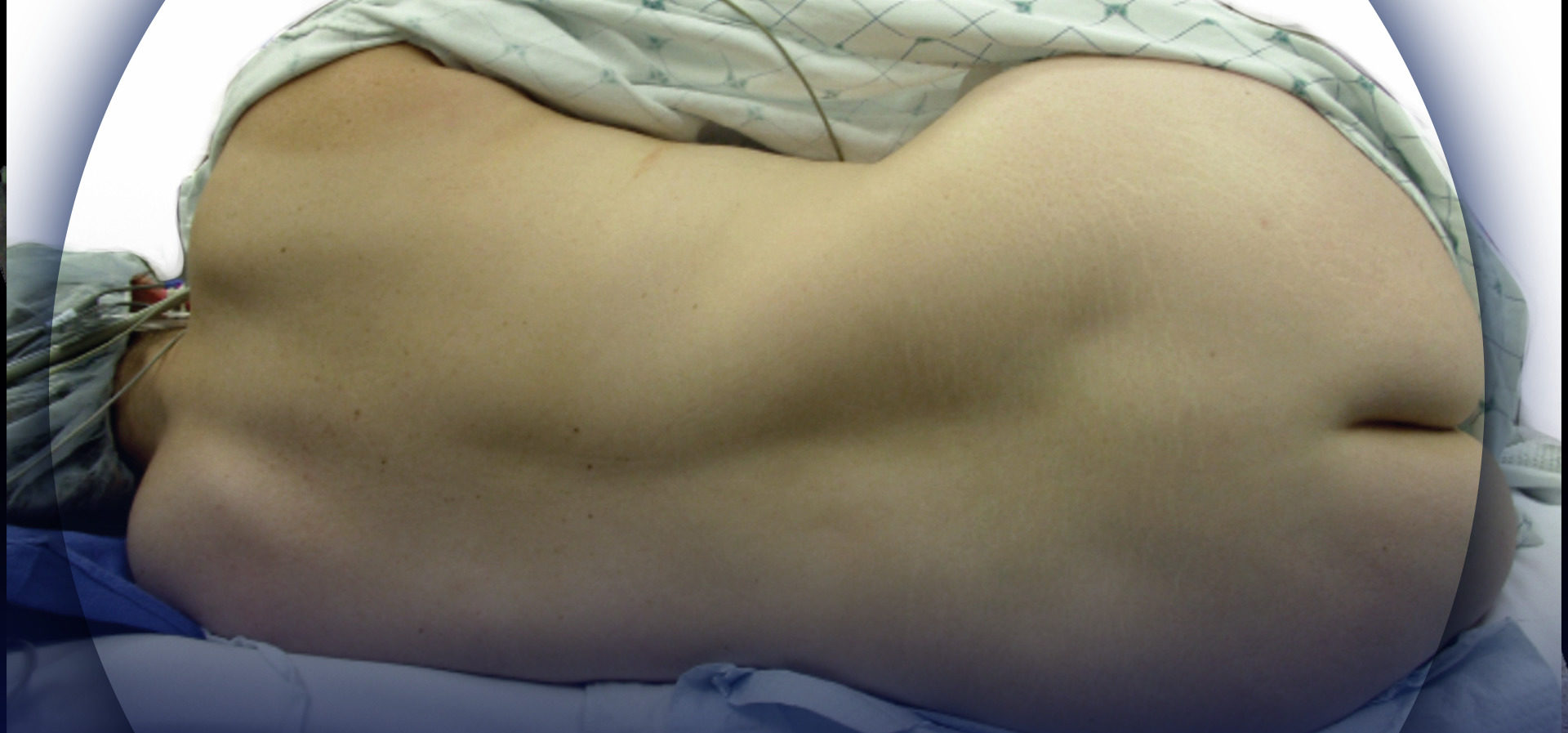
Positioning and preparation
- Positioning
- Seated or lateral position, ideally seated on the side of the bed with shoulders slumped down flexing the lumbar spine
- Ideally the patient should be wide awake, so they can tell you about any neurological symptoms during the procedure, but you can perform spinals under sedation or general anaesthesia
- Identify space
- Iliac crests mark Tuffier’s line which lies between L4 and L5
- L3/4 or L4/5 are acceptable spaces to use
- Midline or paramedian approach
- Scrub and prepare equipment
- 0.5% Chlorhexidine or similar to clean the skin*
- 25g pencil point (Sprotte) needle with introducer
- Local anaesthetic lidocaine 1% for skin
- Hyperbaric bupivacaine or prilocaine etc for injection
*Allow this to dry before pushing a needle through it - theoretically you can drag wet chlorhexidine into the spinal canal with your needle which is suboptimal.
The procedure itself
- Insert introducer into ligament
- Insert spinal needle and slowly advance feeling the texture of the tissue until there is a slight give
- Remove trocar and observe for clear colourless CSF
- Attach syringe with injectate and withdraw gently to confirm free flow of CSF
- Smoothly inject and confirm CSF aspiration still possible at the end
- Remove all needles and apply dressing
Post procedure monitoring
- Monitor blood pressure at regular intervals
- Ensure adequate fluid replacement and vasopressors as required
- Monitor neurological status to assess for signs of high spinal or toxicity
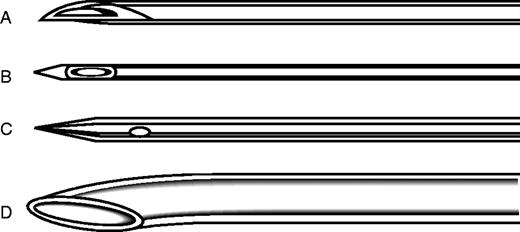
Types of needle
You can either have a cutting needle or a blunt 'pencil point' needle, and you need to know their names.
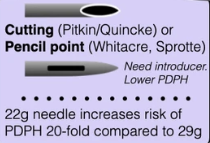
The theory goes that a blunt needle will 'part' the fibres of the dura, allowing them to spring back into position with less bleeding and lower risk of csf leak than a cutting needle.
Location, location, location
Clearly when thrusting a metal spike toward the single largest nerve tract in the body, one would be prudent to do so in as safe a location as possible.
This location is below L3, where there is no spinal cord to hit.
"But the spinal cord terminates at L1, so why L3?"
Because in 10% of adults it terminates at L3, so L1/2 isn't as safe as you'd think.
You can do spinals higher up, as demonstrated by this tweet below, however it's rather specialist, and carries substantially higher risk as one might imagine.
Defining the role of thoracic spinal anaesthesia. New narrative review by Dr le Roux and colleagues.#anaesthesia #anaesthesia #pain #perioperativehttps://t.co/ZqNQuABavf pic.twitter.com/yd6nN40snC
— British Journal of Anaesthesia (@BJAJournals) April 12, 2022
What to give and how much?
Spinal anaesthetics require only very small doses of local anaesthetic to be powerfully effective.
Local anaesthetics commonly used for spinal anaesthesia
- Bupivacaine
- Hyperbaric bupivacaine - probably the most commonly used, solid all-rounder
- Levobupivacaine
- Ropivacaine
- Prilocaine - short acting, great for day cases
- Chloroprocaine
Lidocaine can be used but is falling out of fashion as it is associated with higher incidence of transient neurological symptoms after injection.
What does 'hyperbaric' mean?
If you add 8% glucose to your anaesthetic mixture then it becomes substantially denser than CSF, meaning it will 'sink' once injected to the lowest point it can. You can then adjust the height of your block by tilting the patient like a spirit level.
(See the glass spine video below)
What else can I inject?
Adjuncts. These are extra drugs that can either improve the efficacy, duration or side effect profile of the spinal anaesthetic.
Commonly used spinal adjuncts
- Opioids (diamorphine, fentanyl, preservative-free morphine)
- Adrenaline
- Clonidine
- Dexamethasone
Bicarbonate and adrenaline have been used with lidocaine to speed up the onset of blockade, but lidocaine is less frequently used nowadays.
When not to stab
As with any procedure, there are always risks and complications, and therefore contraindications as well, and these can be divided into absolute and relative.
Absolute contraindications
- Patient refusal
- Local anaesthetic allergy
- Infection over needle insertion point
- Severe systemic sepsis
- Severe hypovolaemia or hypotension
- Uncorrected coagulopathy
- Undiagnosed neurological symptoms
- Evidence of increased neurological pressure
Relative contraindications
- Moderate infective symptoms or inflammatory markers
- Surgery lasting over two hours*
- Reversible clotting abnormalities
*This doesn't make your spinal higher risk, it's just unlikely your spinal is going to last long enough to be your sole anaesthetic technique. You can still use a spinal for analgesia alongside a general anaesthetic for a four hour laparotomy for example.
There are only really four things that can go wrong with a spinal:
- Bad reaction to the drug, either allergic or cardiovascular instability
- Bleeding and risk of spinal canal haematoma
- Introduction of infection into the central nervous system
- Leakage of CSF and potential imbalance of pressures leading to coning if significantly raised intracranial pressure
Hopefully these three points help to explain the rationale behind each of the above contraindications.
Where does the needle go?
A classic FRCA Primary OSCE question - naming the layers the needle passes through on its journey to the CSF.
- Skin
- Subcutaneous fat
- Supraspinous ligament
- Interspinous ligament
- Ligamentum flavum
- Epidural space
- Dura
- Arachnoid
- CSF
How high is too high?
It probably goes without saying that you need your spinal anaesthetic to be blocking nerves to a higher level than the surgeon is going to be slicing. Therefore we generally tend to reserve spinal anaesthesia for lower abdomen and below (unless you're using it for extra pain relief alongside a general anaesthetic).
This is easily done with a lumbar injection for lower limb surgery, as you only really need to be hitting T11-12 and below to cover the important dermatomes, myotomes and osteotomes.
For caesarean section however, you need to block up to T4, covering all the nerves supplying the uterus and relevant bits of the abdomen, to ensure that the baby is the only one screaming in theatre.
A quick reminder of dermatomal landmarks
- C8 - Little finger
- T4 - Nipple
- T7 - Xiphoid process
- T10 - Umbilicus
- L1 - Inguinal crease
- S4 - Perineum
Four things determine the height of your block:
- The amount of local anaesthetic you inject
- How fast you inject it
- How big the patient is
- How you position the patient after injecting
This video is an absolute must-watch. It beautifully demonstrates how the drug moves through the csf, and the effects of a hyperbaric solution.
What to look out for
As one might expect, when injecting drug into a column of fluid, the extent to which it spreads - and therefore the height of the block obtained - can vary substantially.
As you anaesthetise higher up the spinal cord, the patient will lose sensation, muscle power and autonomic supply at higher levels, and they'll start to feel short of breath as the intercostals are affected in the mid-thoracic levels.
Remember the diaphragm is innervated from C3, 4 and 5 levels, so you need a very high spinal for complete respiratory paralysis, however the patient can feel seriously short of breath from intercostal blockade, especially if they're harbouring a baby in their abdomen.
Moving up through T1-4, we see the cardioaccelerator fibres of the sympathetic system being affected, producing a profound bradycardia (a mild bradycardia is a good sign that your spinal is high enough (T4) for a caesarean section).
Above T1 and C8 and the patient will start feeling weakness in their hands, and may have reduced grip strength - so asking them to squeeze your hands firmly is a good way to reassure yourself it hasn't spread too high.
Higher than this and we're headed into the realms of severe hypotension, respiratory failure and reduced consciousness requiring intubation - not necessarily disastrous, but clearly not ideal if they just needed a knee replacement.
When it goes wrong
Every procedure we do has risks and complications, and spinal anaesthesia is no different.
What are the risks and complications of spinal anaesthesia?
Mild
- Nausea and vomiting
- Hypotension (1: 50 ish)
- Itching
- Urinary retention
- Shivering
Moderate
- Failure of procedure
- Headache (1:150 ish)
Severe
- High spinal or total spinal anaesthesia
- Epidural abscess (1:50 000 ish)
- Nerve damage (1:100 000 ish)
- Epidural haematoma (1:170 000 ish)
- Paralysis (1:250 000 ish)
- Death (vanishingly rare)
Why a headache?
If you put a hole in the dura and allow CSF to leak out, the brain has less fluid in which to float, and the intracranial pressure drops, producing a characteristic and rather unpleastant post dural puncture headache.
This is classically a throbbing occipito-frontal headache that is highly positional - improving greatly on lying down, and worsening on standing upright.
Patients may report photophobia, stiff neck, nausea and vomiting and can be totally floored by it.
Assuming the leak has been stopped, the fluid will gradually be replaced over the next few days and 90% of PDP headaches will resolve within a week by themselves.
If there is suspicion that the leak is ongoing, then clearly the obvious solution is to take 20ml of the patient's own blood and thrust it into their epidural space to duct-tape the hole.
Shared with permission from nysora.com
Signs and symptoms of a high spinal
- Bradycardia
- Hypotension
- Shortness of breath and desaturation
- Weakness in hands
- Tingling and numbness in face
- Reduced consciousness
- Apnoea
- Coma
Management of a high spinal
Amazingly, we're going to do something that we never do in anaesthesia, we're going to assess and treat in an ABCDE fashion...
- 100% oxygen and call for skilled senior assistance
- Reassure the patient that they're going to be okay (and escort birth partner out if present)
- Explain to the theatre team that you need to intubate the patient
- Get intubation drugs and equipment ready - (if the patient is losing consciousness you don't need to give as much hypnotic agent)
- Give a big fluid bolus (assuming no contraindications) and maintain blood pressure with vasopressors to offset the rather inconvenient sympathetic blockade
- Intubate and maintain general anaesthesia with either volatile or an intravenous anaesthetic agent
- Maintain anaesthesia and continue with surgery if safe to do so
- Discuss with ICU if spinal hasn't clearly worn off by the time comes to extubate, as they may need an extended period of ventilation
Intrathecal catheters
Long story short - you can put catheters in the subarachnoid space and give very small infusions to achieve very accurate spinal anaesthesia in high risk patients, as documented here:
🔐Ultra-low-dose spinal anaesthesia for elective hip arthroplasty in a patient with severe pulmonary hypertension.
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 𝘙𝘦𝘱𝘰𝘳𝘵𝘴 (@Anaes_Reports) December 1, 2020
This great new report from @BarnwellNiamh is now available to read and download #FreeForAWeek!
🔗https://t.co/ieY4J4de2c pic.twitter.com/K42FeiDnwD
However unless you're working in a department that performs this sort of technique on the daily, we'd suggest you stick to a single injection for now.
Unless you have a very high risk obstetric patient and you've just dural tapped them while trying to do an epidural, in which case read this.
Here's our intro video to spinals and epidurals
@anaestheasier if you're looking after a patient with an epidural, here is an intro as to how they work and what to look out for.
♬ original sound - Anaestheasier
Useful Tweets and Resources
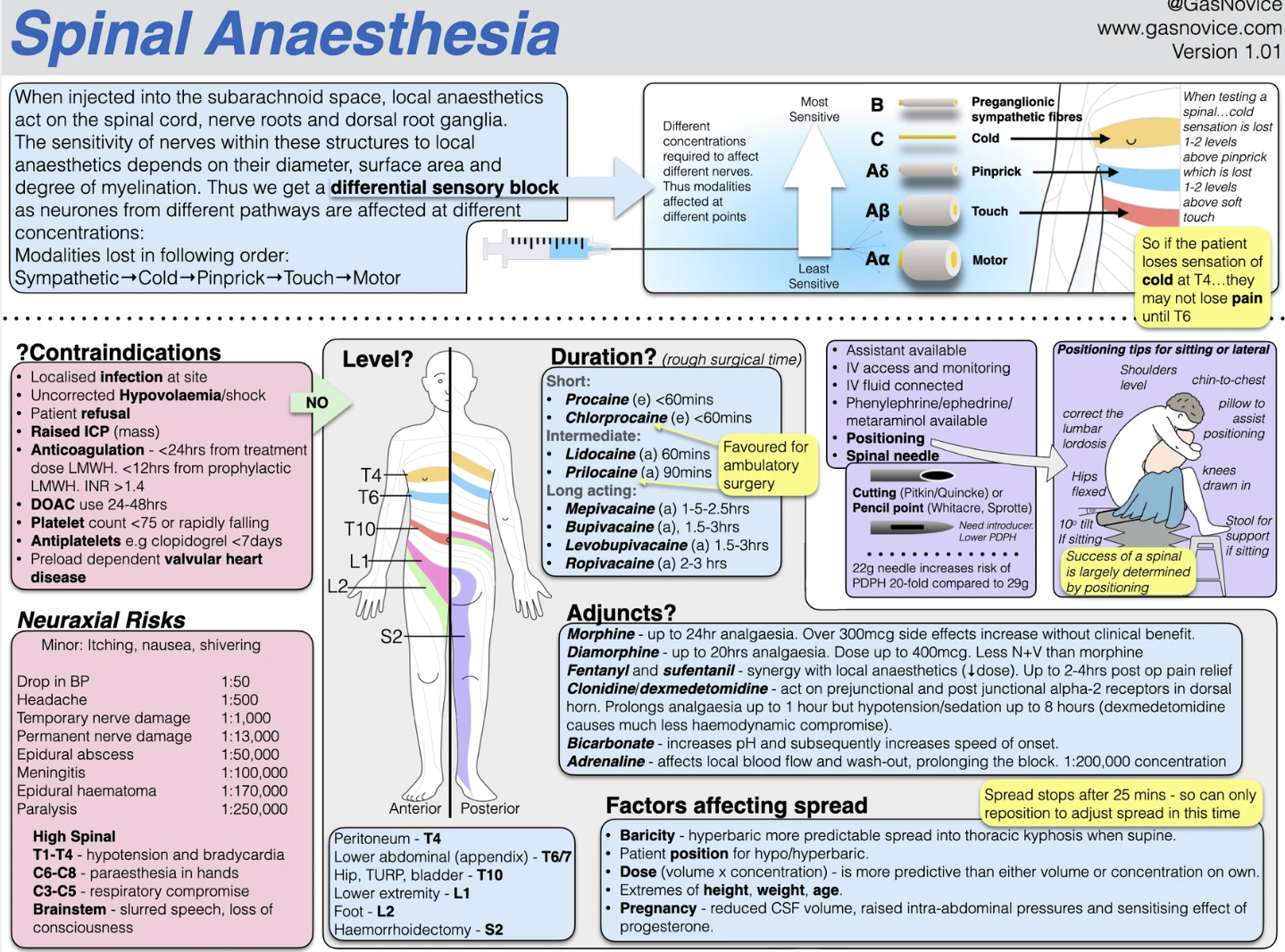
Tap the infographic to go to the brilliant gasnovice.com
#OTD in 1898, August Bier performed the first spinal anaesthesia 💉 It was the first of 6 trial operations using cocaine. After half of the patients experienced headaches & vomiting post op, Bier tried it on himself & his assistant “to reach a well-informed opinion.” #histmed pic.twitter.com/hzetqz9tzx
— Anaesthesia Heritage (@Anaes_Heritage) August 16, 2020
Asystole following spinal anesthesia!
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 𝘙𝘦𝘱𝘰𝘳𝘵𝘴 (@Anaes_Reports) January 9, 2023
Read about the proposed aetiology of cardiac arrest under spinal anaesthesia and refresh your understanding of cardiac reflex mechanisms including Bezold–Jarisch, reverse Bainbridge & the pacemaker stretch reflex.
🔗 https://t.co/6JcncVWG2W pic.twitter.com/biBcRYgfY2
References and Further Reading

Everything you could possibly ever want to know about spinal anaesthesia
Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.