TIVA and TCI

Take home messages
- TIVA is cool, and probably better for the environment, but has a higher risk of awareness than vapour anaesthesia
- There are lots of clever models to work out how much propofol to give the patient
- The numbers are still a guess, and you need to titrate to clinical effect
Podcast Episode
What are TIVA and TCI?
- TIVA stands for total intravenous anaesthesia, meaning you're not using any gases or vapours to anaesthetise the patient
- TCI stands for target controlled infusion, which refers to the clever calculations performed by the pumps to infuse the right amount of anaesthetic agent, rather than you guessing and bolusing as you go
There are few things quite as pleasing as a seriously slick TIVA anaesthetic, where the patient wakes up like the protagonist of a romantic comedy on a sunny day. There's no coughing, no emergence delirium, and they're not retching up their fasted, vapour-filled stomach in recovery.
There are many reasons to use TIVA over the old-fashioned (but still good!) vapour techniques, including:
- Patient at risk of malignant hyperthermia
- Previous severe post operative nausea and vomiting
- The nature of the surgery will make delivery reliable amounts of vapour hard, as in some ENT and thoracics cases
(See the CRQ questions below for the full list of indications for the exam)
What can I use for TIVA?
Technically, any combination of hypnotic and opioid will work, however the most commonly used combination is the two best friends - propofol and remifentanil.
Why use propofol?
- Rapid onset within 30s and offset within a few minutes
- It undergoes hepatic metabolism to inactive metabolites
- Peak action is at approxmately 1.5-2mins after injection, as the drug needs to travel to, and infiltrate into, the CNS
- The offset is due to its redistribution out of the plasma and therefore out of the CNS, rather than being due to elimination from the body
- Its distribution half-life is therefore 1–2 min
Why use remifentanil?
- Remifentanil is a synthetic opioid fentanyl derivative and a pure μ agonist
- It is rapidly metabolised by plasma and tissue, especially muscle, esterases
- It is particularly broken down in muscle tissue and its metabolites are essentially inactive
- One of the benefits of remifentanil is its very low context-sensitive half life
- This means that even after very long infusions, the elimination half life remains around only 5-8 minutes
- This is due to rapid metabolism and small volume of distribution as it is essentially confined to the plasma
- At the end of surgery, a continued infusion with a target of 1-2ng/ml can facilitate a very smooth extubation
An example target concentration at induction would be 4-8ng/ml and 3-6ng/ml during the operation
- The Minto model will give a initial bolus dose 3x higher if the effect site target is used compared to the plasma target
What's nice about these two is their synergistic effect, meaning their combined action requires less of both drugs for a satisfactory clinical effect.
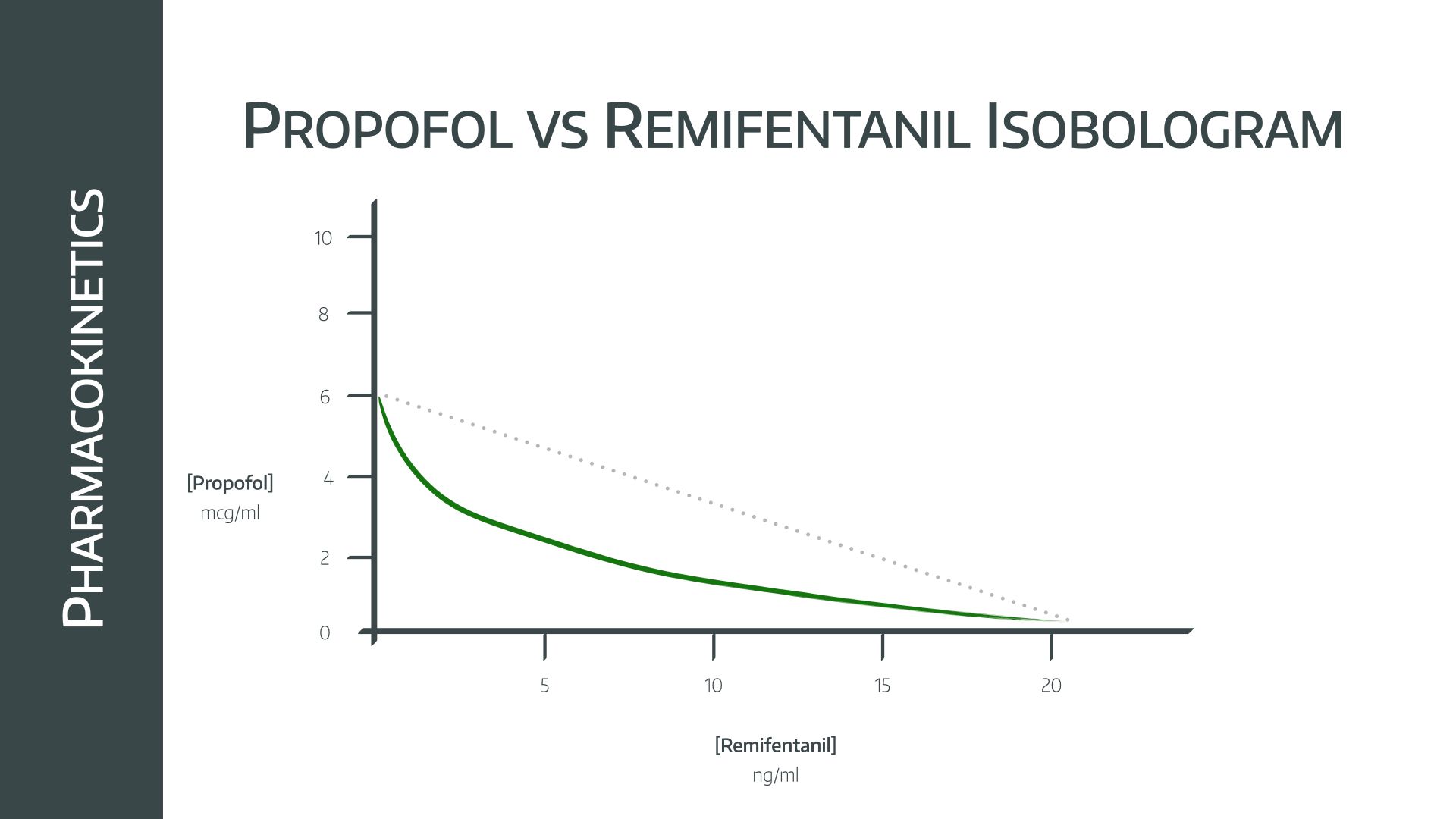
- The line on the isobologram below represents ‘equal clinical effect’, so you can see that if given together, much less of each is needed for the same clinical effect
- Together they are very effective at obtunding laryngeal reflexes for intubation, meaning muscle relaxation can often be avoided
Just remember that remifentanil doesn't provide any real hypnosis, so you should have at least 2-3μg ml−1 effect site propofol running to ensure the patient is nicely asleep.
You can't measure propofol in the patient
Well, you can, but it's not widely available or validated enough to be used in any meaningful way for routine anaesthesia.
It's certainly not as simple as measuring end tidal volatile agent to reassure yourself your patient is actually asleep.
Essentially every time you administer propofol to a patient, you're guesstimating how much they're going to need, and calibrating your doses to the patient's individual needs, based on clinical parameters like their weight, age and height.
Because this is both risky and tiresome, some very clever people put together some algorithms that work out, based on a few inputted parameters, how the drug is likely to behave in their body, and therefore how much is needed to achieve certain estimated 'levels' in the body.
To do this, they use compartment models.
(This is absolute prime FRCA Primary OSCE material, so it's worth taking the time to understand.)
The one compartment model
This is the simplest option, and it assumes the entire body is one gelatinous bucket of homogeneous goop into which the drug is injected and from which it is eventually eliminated.
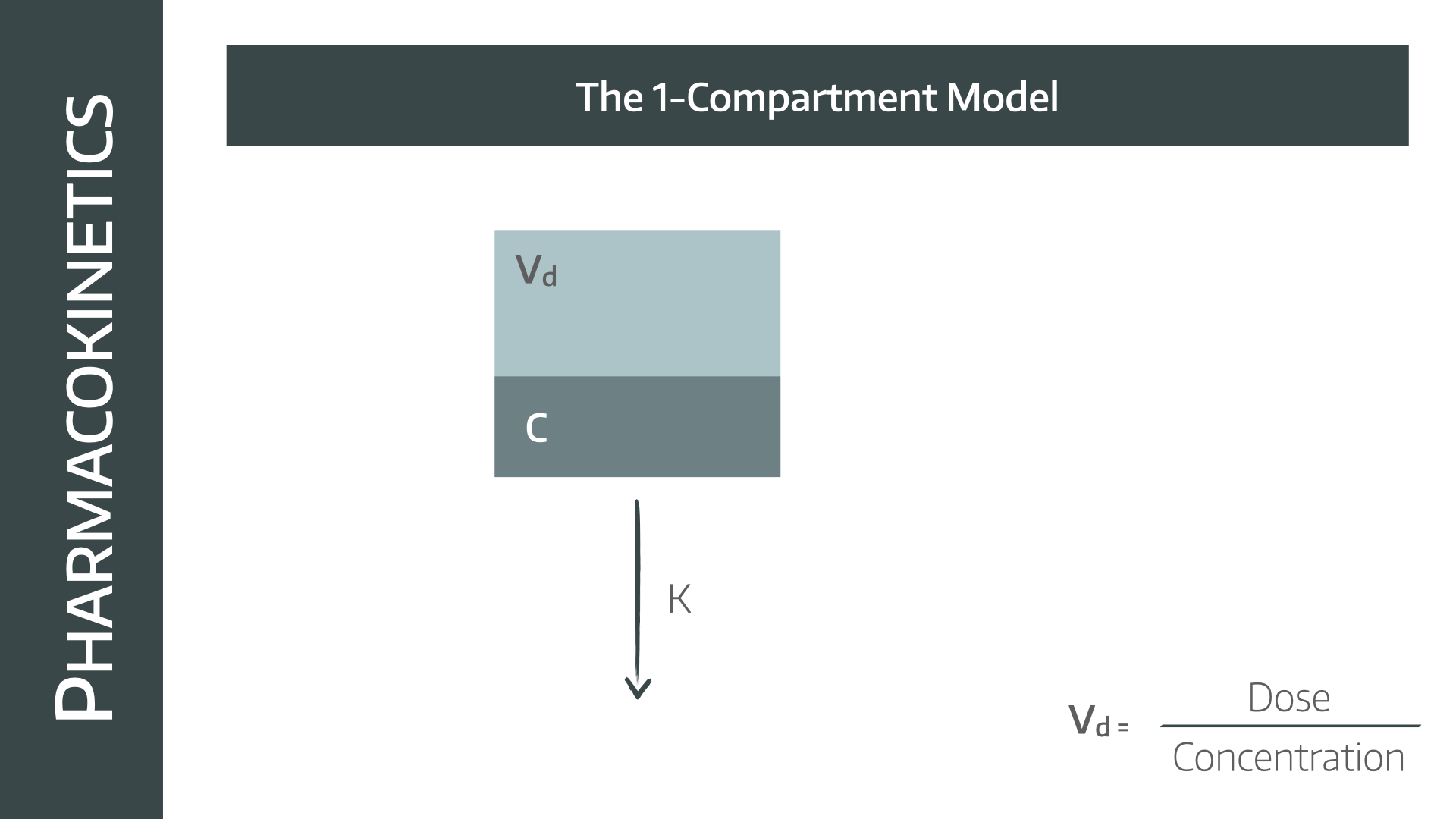
The assumption, to make the maths work out, is that the drug is injected and immediately distributes evenly throughout the whole compartment. If this (impossible) assumption is made then the following conclusions can be drawn:
- Elimination of the drug is exponential with a single elimination rate constant, because a set proportion of the remaining plasma concentration is removed per unit time
- The concentration at any given time t is given by the negative exponential equation:
C = Co x e^(-kt)
- Where Co = concentration at time zero and k = elimination rate constant
- The rate constant tells you what proportion of the volume of distribution is cleared completely of drug per unit time
- The rate constant determines the gradient of this graph
- The higher the rate constant, the faster the clearance, and the steeper the graph
In reality
We can’t directly measure the concentration at time zero because the drug doesn’t instantly distribute in the plasma, so we have to infer the starting concentration by extrapolating backwards using the natural log concentration graph shown below
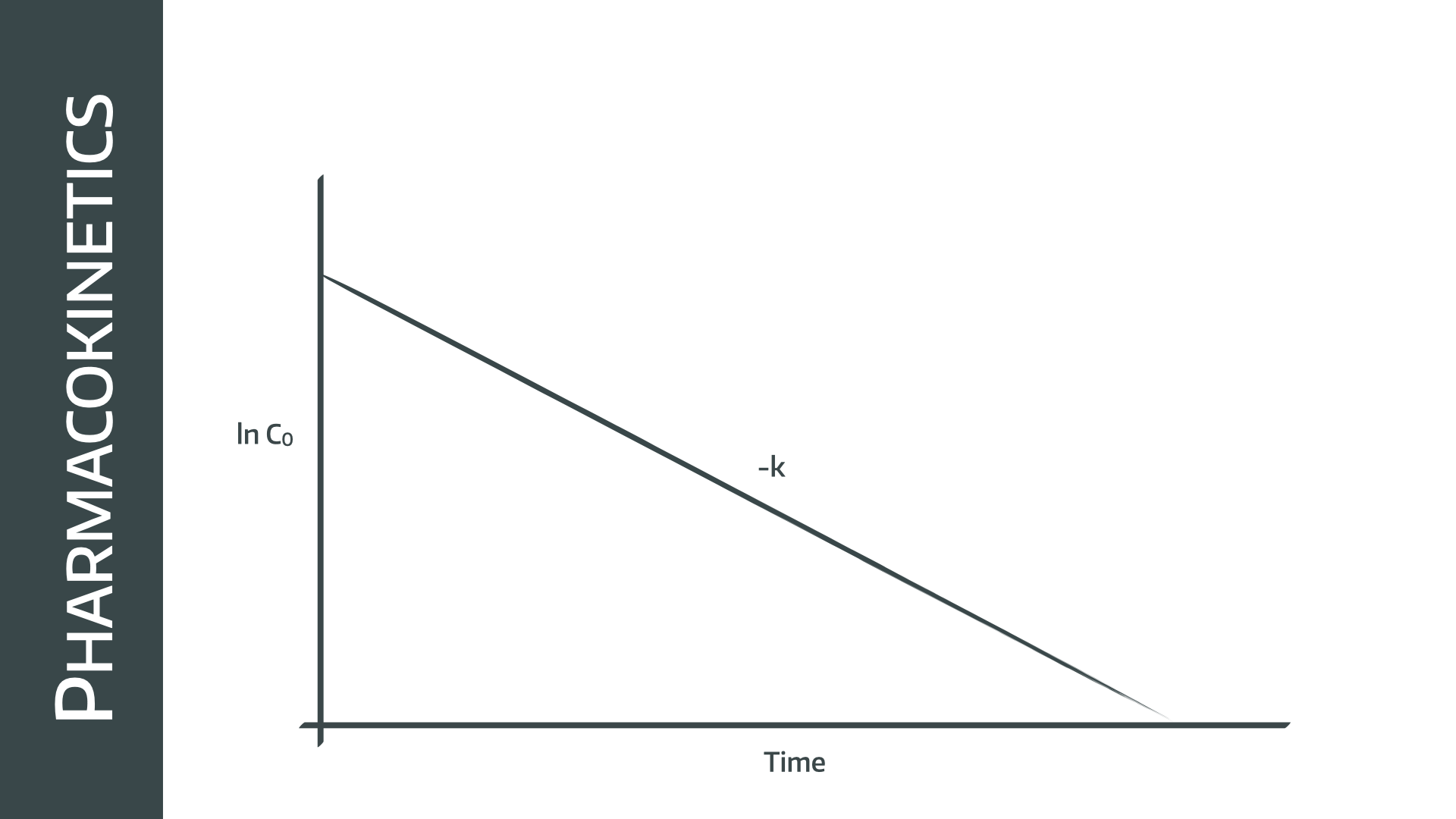
- In the one compartment model, clearance is equal to the elimination rate constant times the volume of distribution
Cl = k.Vd
- By definition, the rate constant k = 1/time constant (τ), so
Cl = Vd/τ
- This proves that clearance for a drug is constant, as the volume of distribution and τ are also both constant for a given drug
How does the model change when giving a continuous infusion?
If we give repeated bolus doses of a drug, then the plasma concentration will rise and fall in a bumpy or ‘sawtooth’ fashion, depending on how quickly the drug is redistributed and cleared by the body.
If we give a continuous infusion however, then the plasma concentration will build gradually to a steady state concentration (Css)
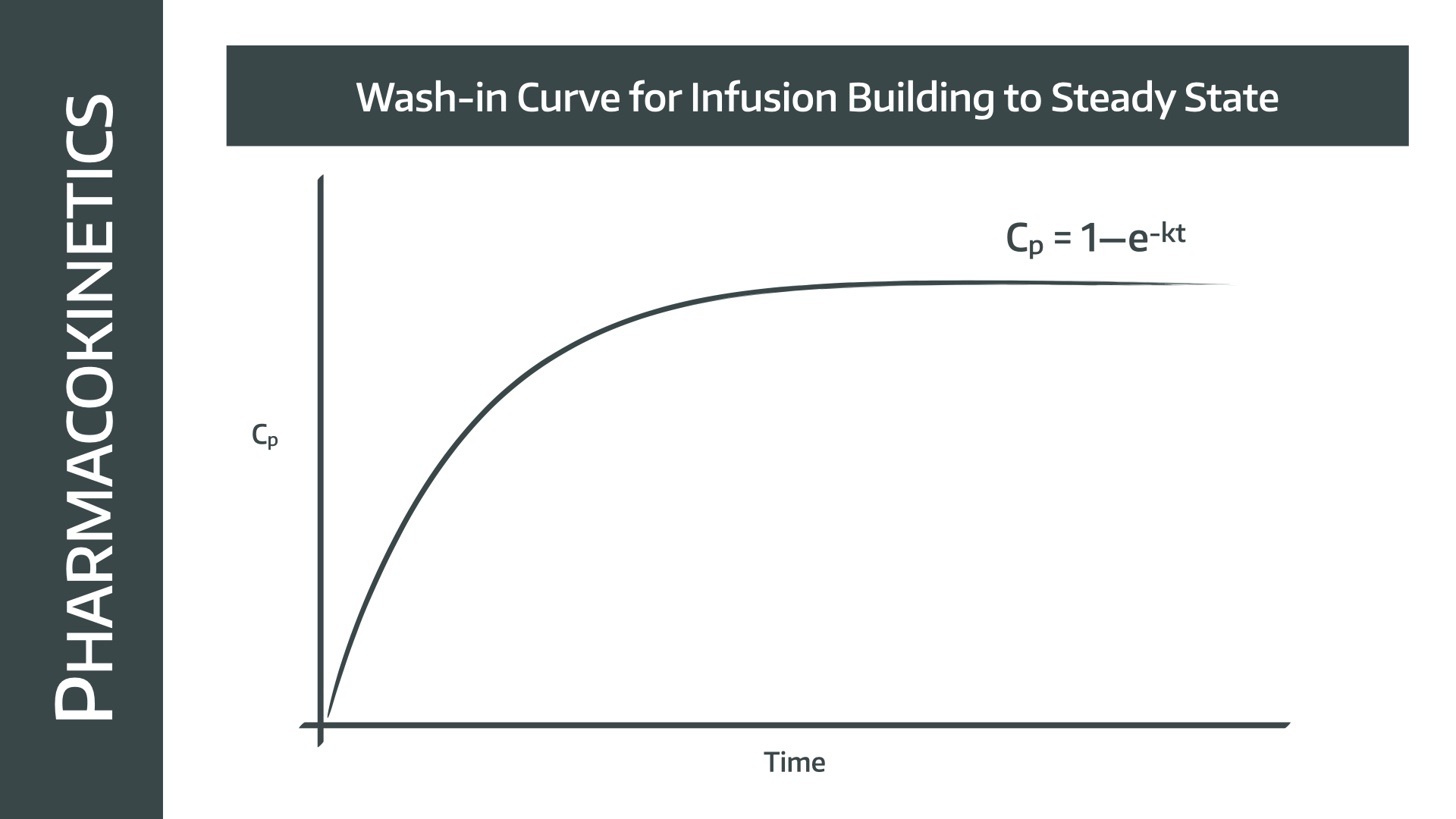
This Css depends on how fast the drug is cleared, and how fast the drug is being given (mg/min), which in itself is determined by the drug concentration (mg/ml), and the infusion rate (ml/min)
- This will give a negative exponential wash in curve
- If no loading dose is given it will take 5 half lives or three time constants to reach steady state
- Remember that a drug with a large volume of distribution will take longer to reach steady state
The two compartment model
This gets slightly more complex, and slightly more realistic, because it acknowledges the fact the body's tissues don't all behave as one uniform fluid, and that different areas receive blood, and therefore drug, at different rates.
The V1 compartment is the blood, and is where the drug is administered to and eliminated from.
V2 is the 'peripheral' compartment, which is then supplied by the blood. The rate at which drug enters and leaves this compartment depends on the concentration gradients between V1 and V2, and other factors such as:
- Blood supply to the compartment
- Presence of facilitated diffusion channels or active transport mechanisms
- Fat solubility of the drug
All of these variables are summarised and simplified into a rate constant that determines how quickly the drug moves in each direction.
For example, the rate constant for the drug moving from V1 to V2 would be K12, and the reverse would be K21.
K0 is the elimination rate constant that we met earlier.
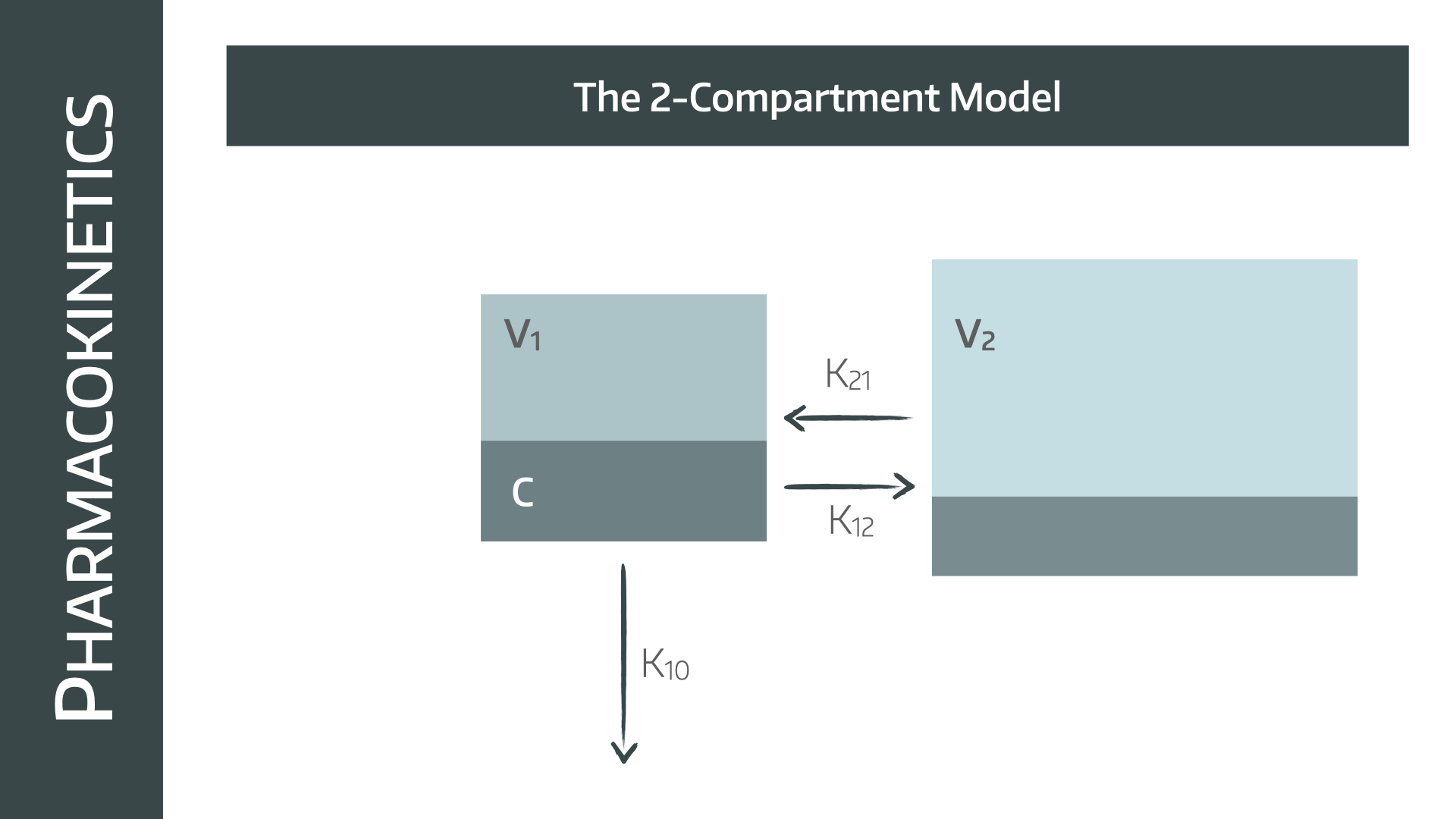
- Therefore, any time when the concentration is higher in the plasma than the tissues, such as when starting the infusion, drug will redistribute into the tissues (K12)
- When the infusion stops, the drug is then cleared from the plasma and excreted, the concentration gradient will reverse, causing drug to move back from the tissues into the plasma (K21)
This will slow the rate at which the concentration in the plasma decreases, by essentially ‘autoinfusing’ drug into the blood from the body tissues.
- This is particularly important for very fat-soluble drugs that accumulate in adipose tissues, and explains why drugs such as fentanyl and propofol take much longer to wear off after a long duration of infusion, as there is far more accumulation of drug that needs to be cleared
This produces a bi-exponential decline on the natural logarithm/ time graph, with an initial rapid drop in plasma concentration as drug redistributes into the tissues, followed by a slower elimination phase, where drug is simultaneously returned to the plasma from the tissues and cleared from the blood
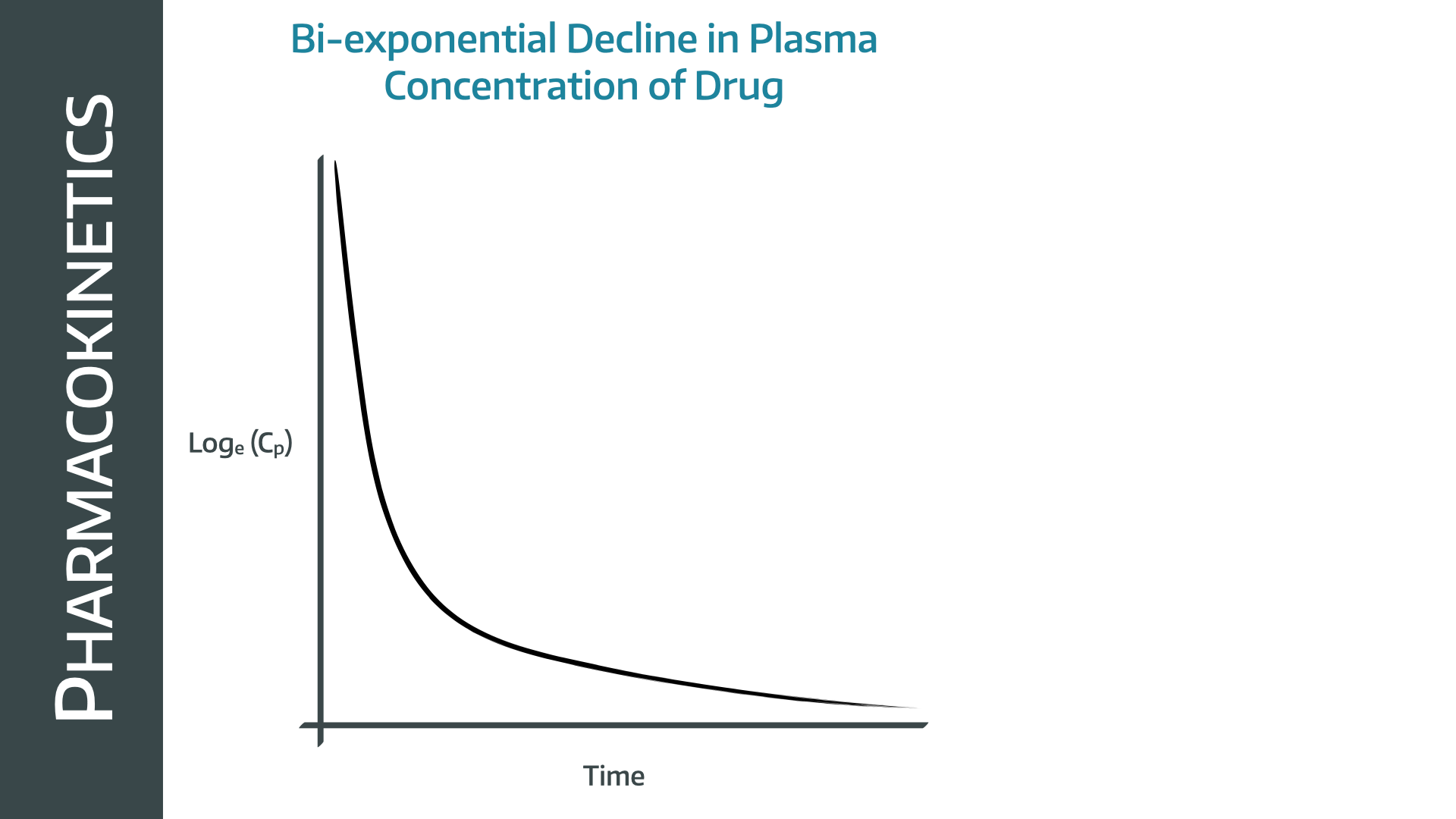
The equation that you need to know for a two compartment model is as follows:
C = A · e^(−αt) + B · e^(−βt)
A common source of confusion is to think that α and β represent the rate constants for each compartment - they don’t, they’re just the calculated time constants that make the equation work out in each given situation
Tell me about the three compartment model
Phew, we're nearly there - I promise.
The three compartment model takes this one step further, and it is the model used in the infusion pumps for running TCI infusions.
It does exactly the same as the two compartment model, but it appreciates that there are some areas of the body with better blood supply (e.g. abdominal organs) and some areas with much lower blood supply (e.g. peripheral fat).
So it makes sense, therefore, to have two separate rate constants, one for the better supplied organs (C2) and one for the the compartment with less supply (C3).
Just as before, drug can only be administered to, and removed from, the central compartment (C1).
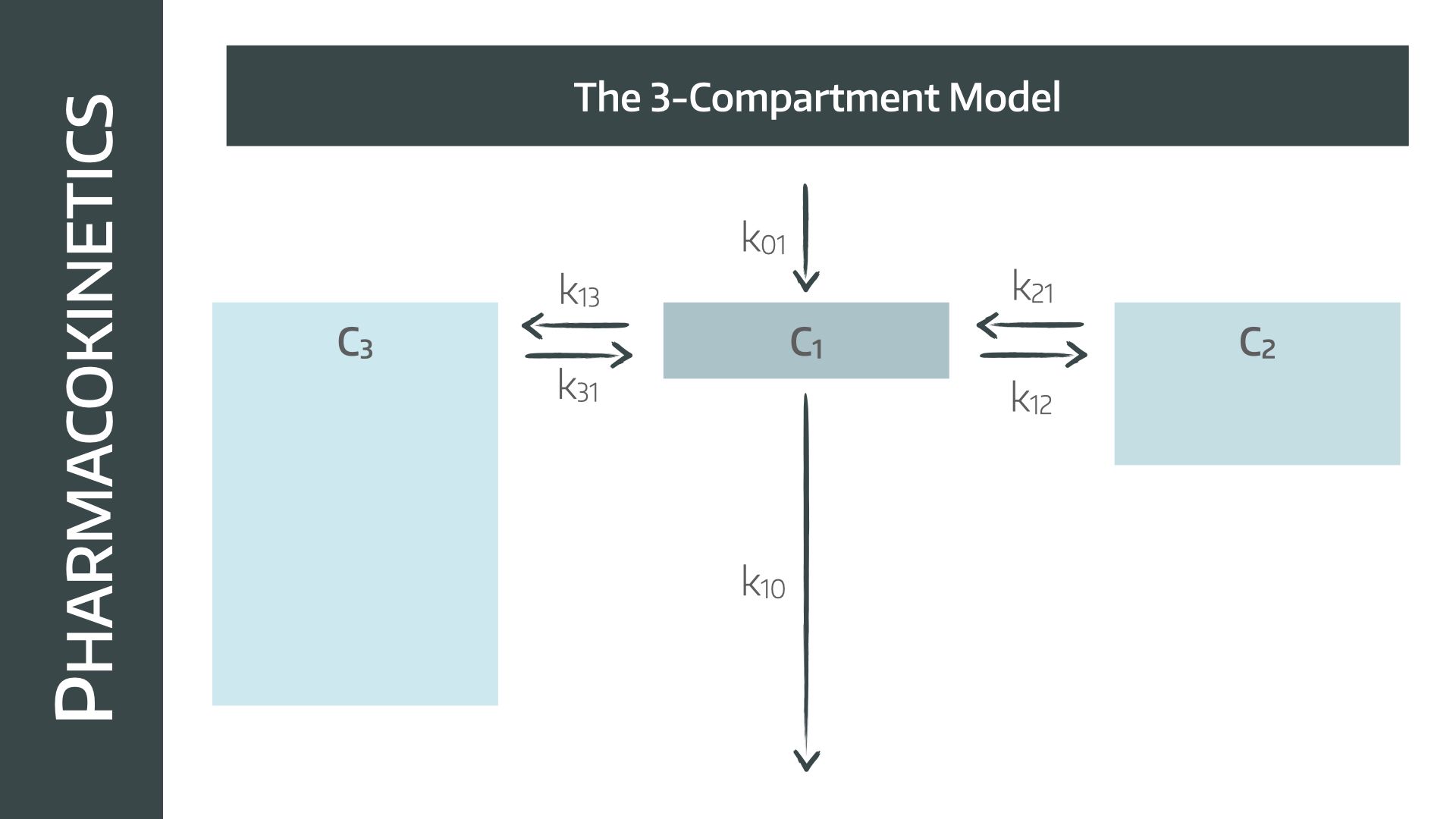
- There are therefore two distribution components and one elimination component
Altogether this results in a tri-exponential decline, which more closely maps the observed concentrations seen in in-vivo measurement
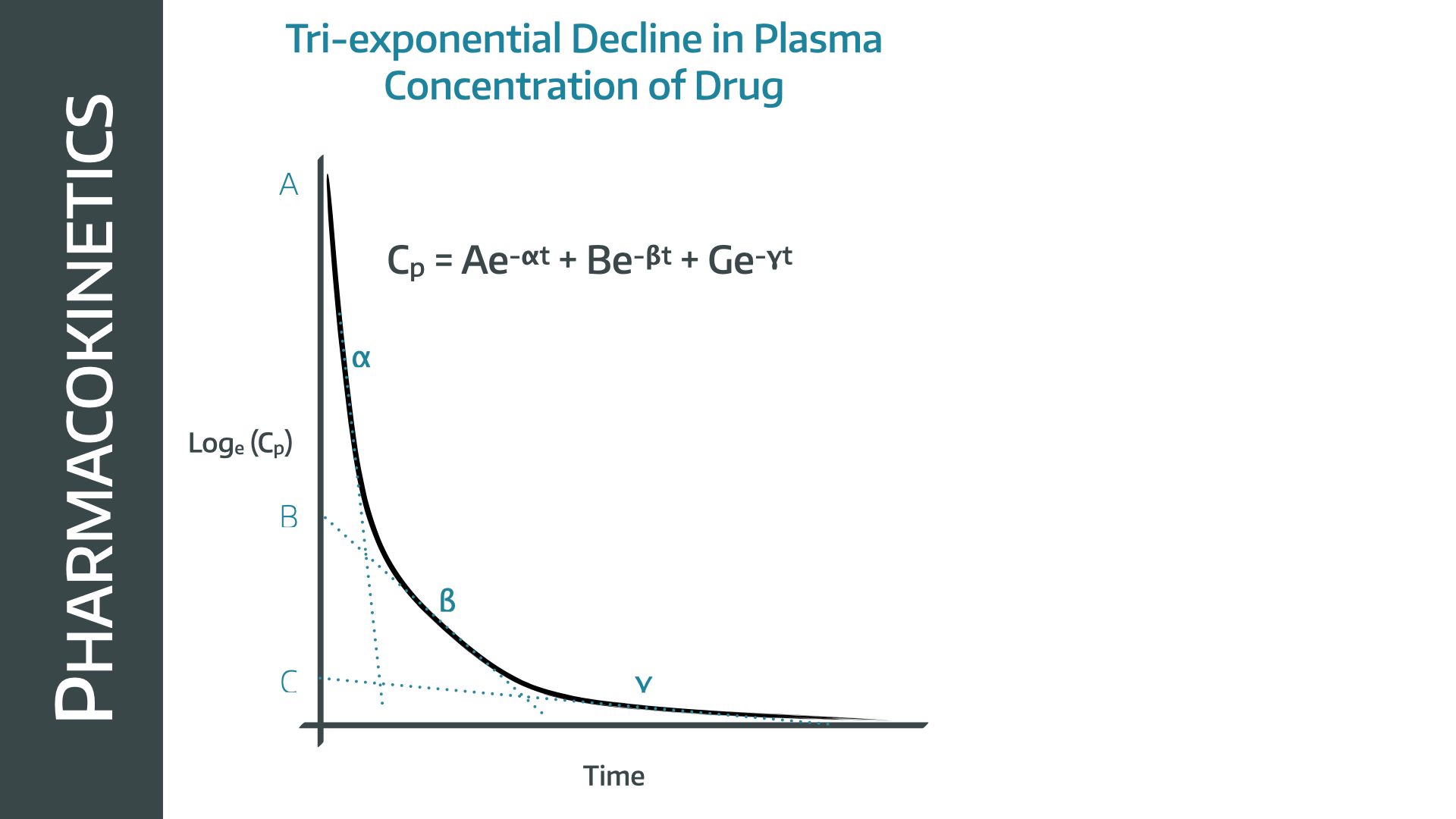
C = A · e−αt + B · e−βt + G · e−γt
- Note that it is the final rate constant that determines the terminal elimination time constant
What is the effect compartment?
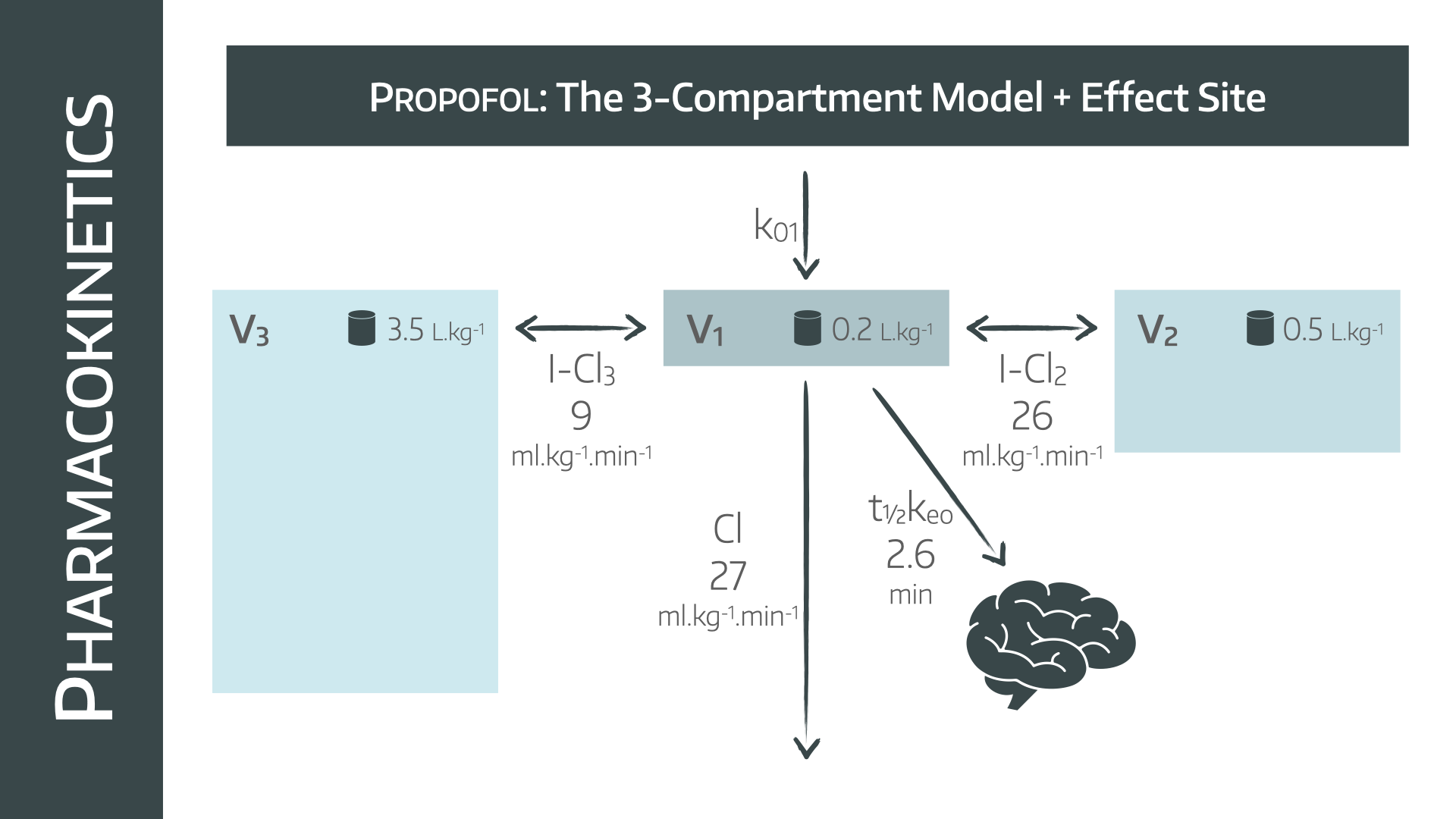
- This is an additional compartment added to the three compartment model, where the drug is believed to take effect, and in anaesthetics usually refers to the brain
- Its volume is considered to be negligable, however it acts on a delay, to allow the drug to reach the effect site, and it therefore has its own elimination rate constant, usually Keo
Ke0 refers to elimination from the effect site, and is therefore relevant because it relates to when the patient is likely to wake up.
Just remember that the drug will still be in the patient's plasma until it is excreted from the body (K10).
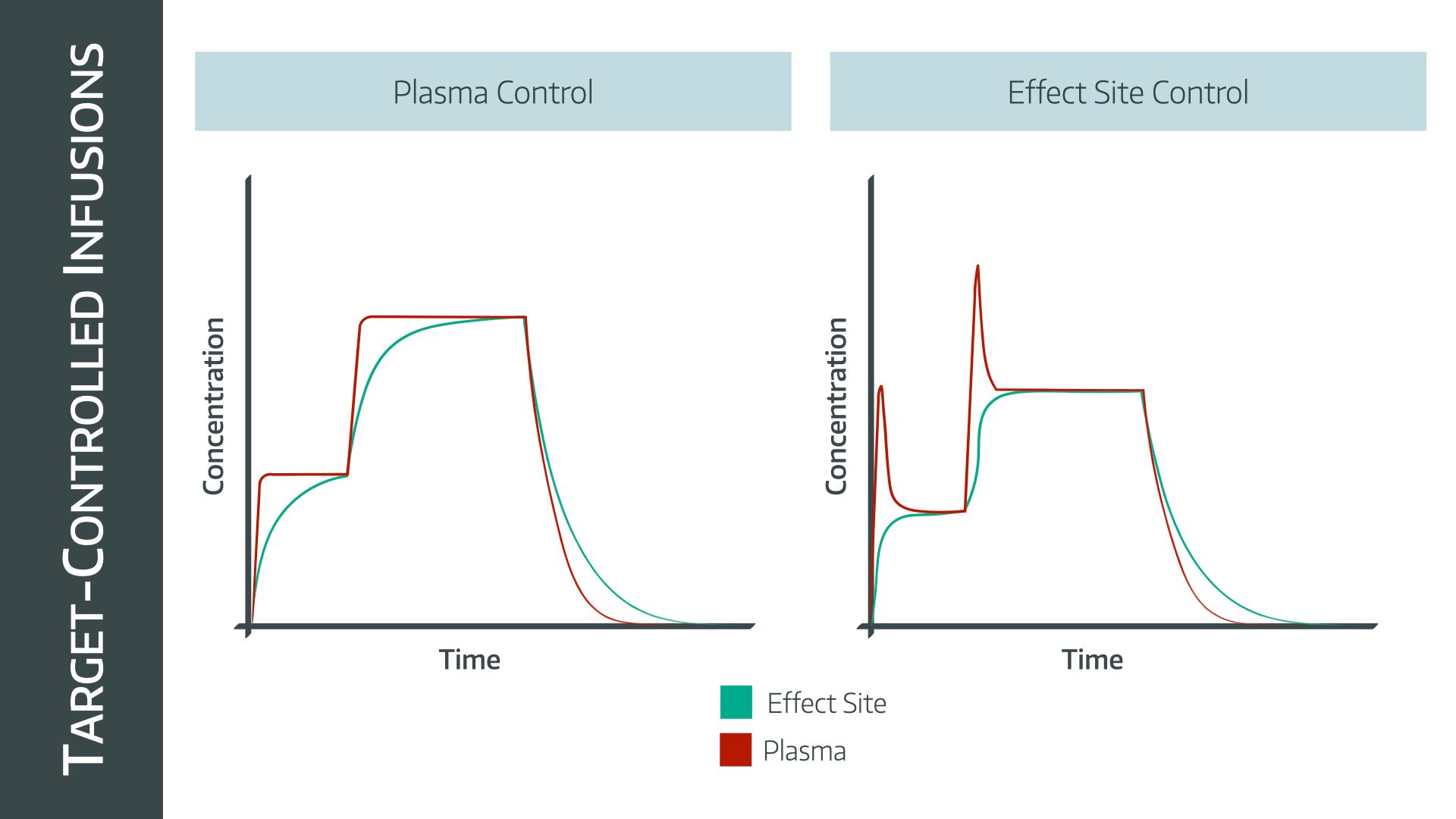
What is 'effect' site targeting?
Any drug infused into the blood is going to take longer to accumulate in the target site (the brain) than the plasma. This is why the models discussed above have an 'effect site' compartment built into the algorithm.
If you want to rapidly establish a certain concentration in the brain, then a larger concentration gradient is needed across the blood brain barrier, and so a higher plasma concentration is required.
- Using the effect site target aims to establish equilibrium between blood and brain concentrations as quickly as possible, and therefore it will ‘overshoot’ the plasma concentration slightly, in order to elicit more rapid changes in effect (brain) site concentration
Key points:
- The Marsh model traditionally targets plasma concentration
- The Schneider model traditionally targets effect site concentration
- In modern machines they can be adjusted to target either
- Patients usually fall asleep at an effect site concentration of 2.5-3μg/ml on propofol alone, or 2-2.5μg/ml if remifentanil is used as well
When the target is changed during the procedure, the pump will either deliver a bolus to rapidly establish the new higher set point, or it will stop the infusion temporarily if the target is lowered, before restarting at a lower rate.
It then becomes clear, therefore, that if you target a certain effect site concentration, the machine is going to deliver a much larger bolus dose, than if you target the same plasma concentration.
- Just note that Marsh and Schnider have very different models of how big V1 is in the patient, and so bolus doses can be wildly different
- Marsh will generally speaking always give a larger bolus at the start, but in reality, it's still less than when we go rogue and dare to use a syringe of propofol with our own hands, and generally produces less overshoot
Some sensible effect site concentrations
Clearly there will be enormous variation here depending on the patient, the surgery and the practitioner. These are just rough figures to give you an idea of what sort of numbers to expect.
For IPPV
- Propofol 3-4μg/ml and Remifentanil 6-8ng/ml
For spontaneous ventilation
- Propofol 4-6μg/ml and Remifentanil 1-3ng/ml
These are your steady-state infusion rate targets, and you should expect to reduce the dose to around half for patients over the age of about 50.
As always - titrate to your individual patient's requirements.
When do I hit go?
Everyone asks it at some point in their anaesthetics training - do I start the remi and the propofol at the same time?
- If you're using effect site targeting for both, then yes definitely
- If you're using effect site for propfol and plasma site for remi, it's a bit more tricky - you can start the remi first and allow it to equilibrate between plasma and effect site, then start the propofol, just remember to tell the patient to breathe
- If you're using plasma site targeting for both drugs, start the remi first
- If you're experienced with TIVA and have your own way of doing things, do that
How do I know they're asleep?
Look at them.
As with all of anaesthetics, the key is to monitor the patient's clinical signs and adjust your drug dosing accordingly. Everyone is different and no model or calculation works perfectly every time.
Key tips:
- Look at the effect site concentration displayed on the pump when the patient closes their eyes - if the concentration during the operation is higher than this number, then they're probably asleep
- Muscle relaxant can safely be given after there is no response to a jaw thrust
- Use BIS or EEG monitoring to reassure yourself that the patient is alright, depending on how well you trust the numbers
We should probably mention NAP5
The Fifth National Audit Project is titled:
Accidental Awareness During General Anaesthesia in the UK and Ireland
- The estimated incidence of patient reports of AAGA was ~1:20,000 anaesthetics
- The incidence of reports of AAGA when neuromuscular blockade was used was ~1:8,000
- When no paralysis was involved this was ~1:136,000
- The incidence of reports from cardiothoracic anaesthesia (~1:8,600) closely resembled that for neuromuscular blockade.
- Caesarean section was much higher, ~1:670
Clearly this refers to awareness under general anaesthesia. For spinal anaesthesia one would hope this number would be closer to 1:1...
- Almost two-thirds of AAGA experiences arose at induction and emergence
- One third of AAGA events arose during the maintenance phase of anaesthesia
Risk factors for accidental awareness under general anaesthesia
- Previous awareness under GA
- Use of neuromuscular blockade
- Use of thiopental
- Use of rapid-sequence induction
- Use of Total intravenous anaesthesia techniques
- Female patients
- Early middle age adults
- Out of hours operating
- Junior anaesthetists
This is core Final CRQ material
Take home message:
If you understand how the TCI models work, and make sure to target your infusions to clinical parameters and BIS, then you can avoid awareness fairly reliably.
Useful Tweets and Resources
If anyone wants any PERUSE posters for their Trust, get in touch.
— Rob Fleming (@RobJimFleming) March 29, 2023
Now in A4, perfect for anaesthetic room walls, or dangling off drip stands.
If you use TIVA, you might be making errors, and a standardised check might mean you make less of them. pic.twitter.com/NLMILlQ4zd
We made a little video
@anaestheasier Propofol sedation using TCI #MedEd #FOAMed #TipsForNewDocs #FiY1 #medschool #anaestheasier #anaesthetics #novice #anaesthesia #revision #pharmacology #FRCA #anesthesiologist #anaesthesialife #anesthesialife #odp #studentodp #emergency #crna #student #surgery #or #nurse #theatre
♬ Monkeys Spinning Monkeys - Kevin MacLeod & Kevin The Monkey


References and Further Reading

Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Please remember as always that all information posted on Anaestheasier.com is for educational purposes only and does not constitute clinical or medical advice.
