Paravertebral block

In our relentless quest to find new and interesting places to shove local anaesthetic into our patients, we (or more accurately Hugo Sellheim) discovered the paravertebral block in 1905 for gynaecological procedures.

The technique was then largely shelved, presumably due to record numbers of unexpected pneumothoraces, until Eason and Wyatt picked it up again in 1979 for management of a variety of complex and chronic pain conditions.
Since the advent and widespread adoption of ultrasound the block has become safer and more popular, although it is finding stiff competition in its erector spinae cousin.
What are the alternatives to paravertebral block?
- Epidural
- Erector spinae plane block
- Retrolaminar block
- Midpoint transverse process to pleura block
- Intercostal paraspinal block
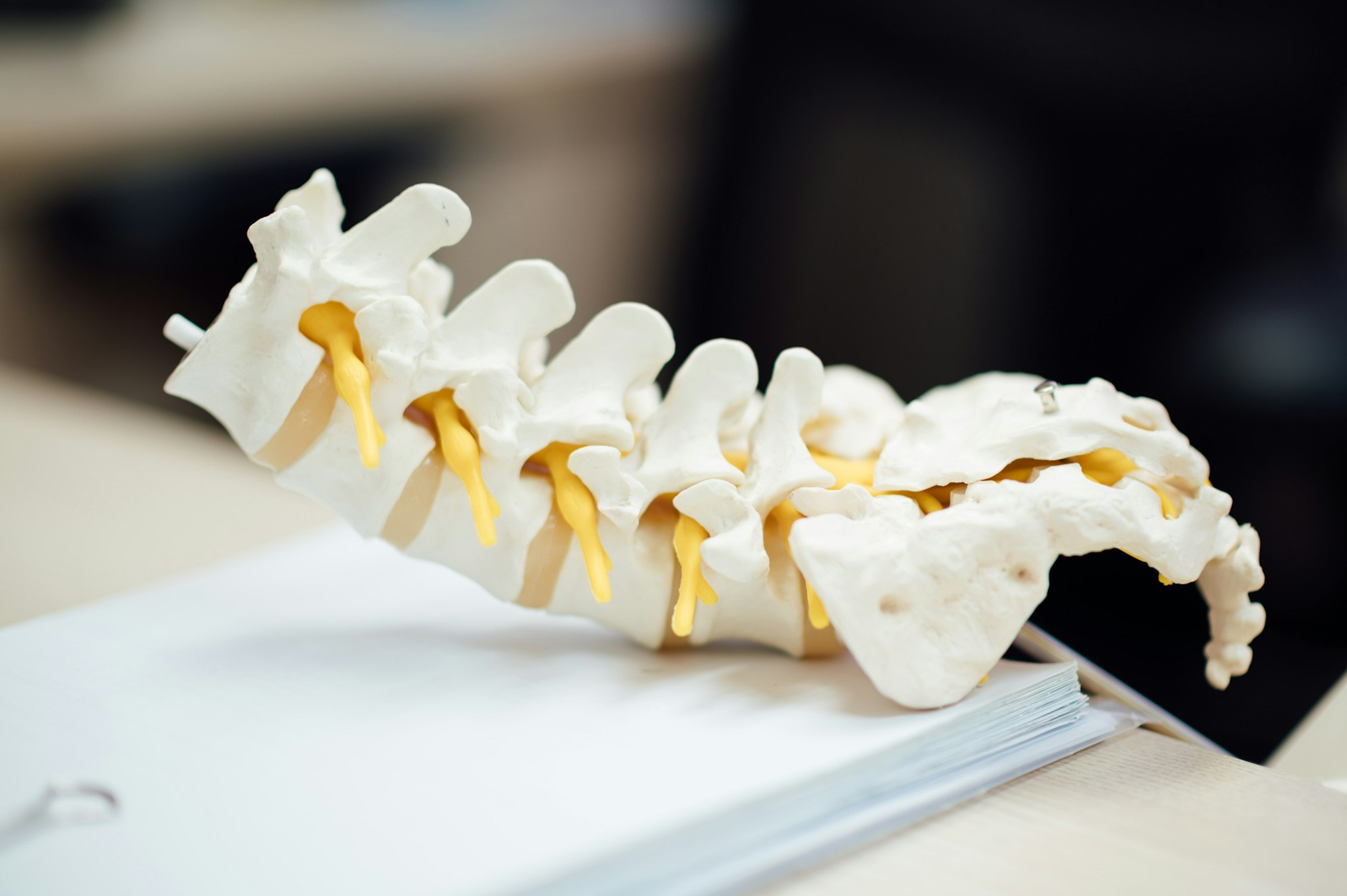
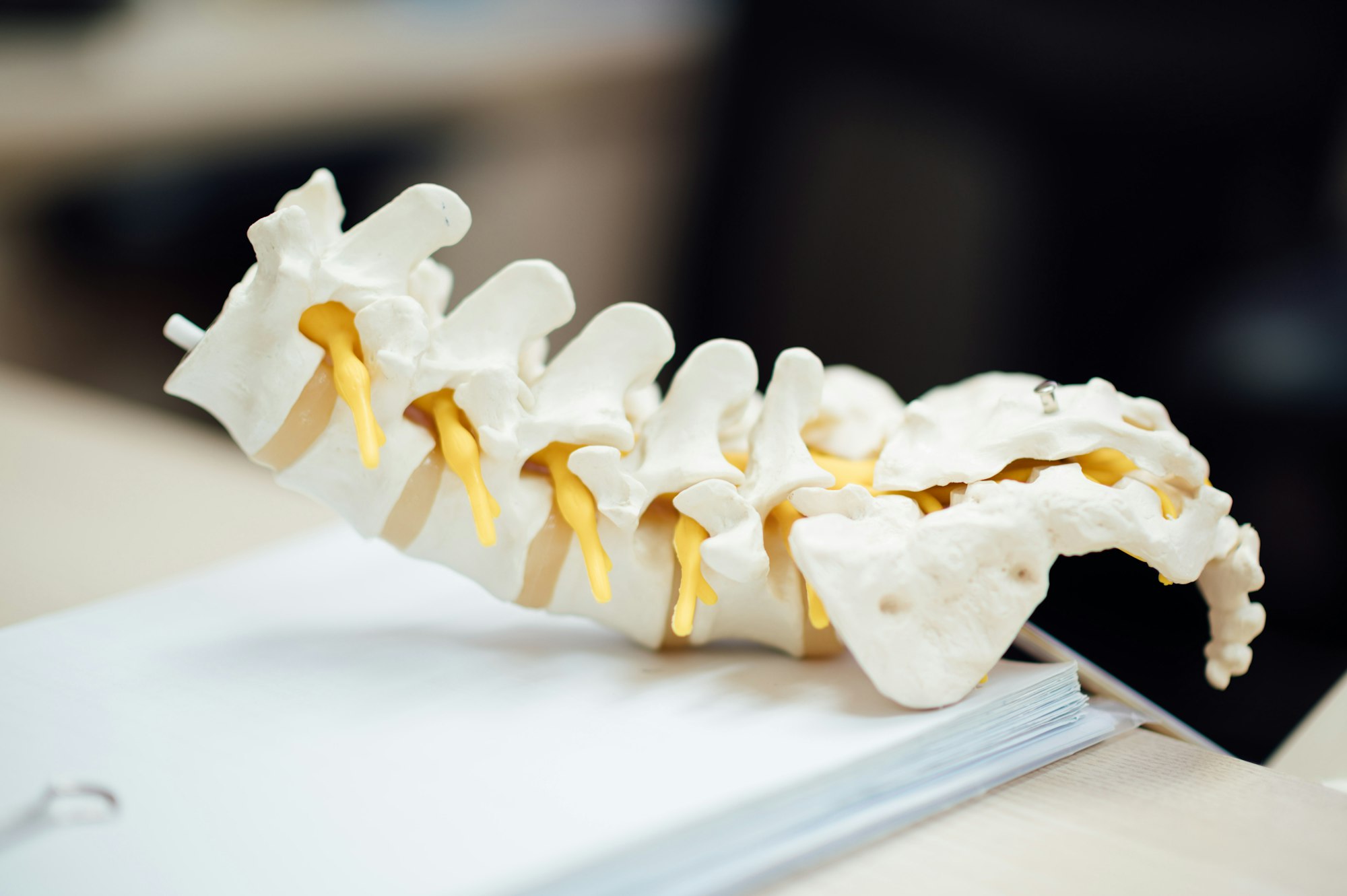
The Anatomy
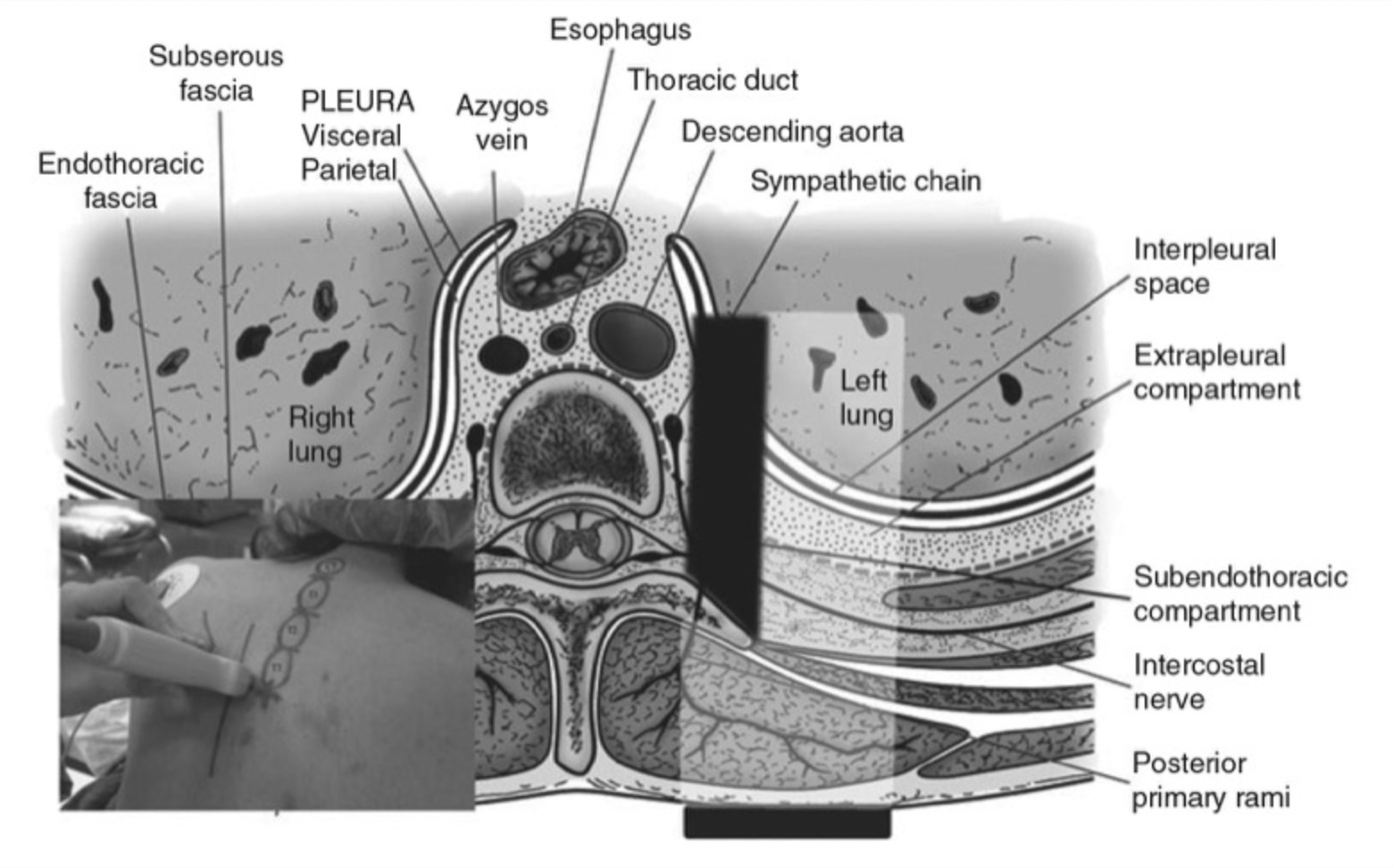
The paravertebral space is a strange anatomical location.
The blue bit looks worryingly close to the very fast red bit.
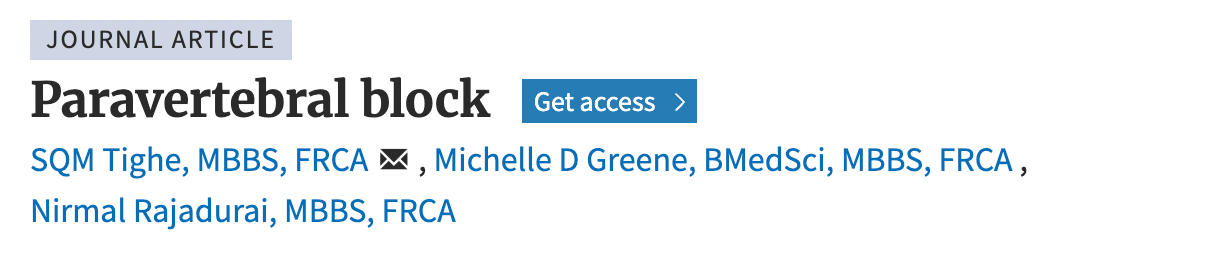
As you can see, and guess from the name, you're aiming just off to the side of the vertebra, into a potential space immediately posterior to the parietal pleura.
The goal is to block the spinal nerves as they emerge from the intervertebral foramen.
Describe the anatomy of the paravertebral space
- A triangular wedge shaped space either side of the vertebral column
- The anterolateral border is the parietal pleura
- The posterior border is the superior costotransverse ligament
- The medial border is the posterolateral aspect of the vertebral body, the intervertebral disc and intervertebral foramen
The thoracic paravertebral space is fairly continuous with loose connective tissue and fat, allowing cranial and caudal spread of injected local anaesthetic.
It will also spread to the epidural space medially and the intercostal space laterally.
A single injection should afford you four to six dermatomes of spread.
Caudal spread is limited by the origin of the psoas muscle.
What are the contents of the paravertebral space?
- Fatty tissue
- Intercostal vessels
- Anterior rami of intercostal nerves
- Dorsal rami of intercostal nerves
- Sympathetic chain
- White and grey rami communicantes
Tell me about the anatomy of the target nerves
- There are eleven intercostals and one subcostal nerve (T12) on each side
- These leave the intervertebral foramina and immediately divide into anterior and posterior divisions
- The anterior divisions start between the pleura and posterior intercostal membrane, then pass between the inner and innermost intercostal muscles, then finish up as an anterior cutaneous branch of the thorax
- The posterior divisions split into medial and lateral branches and supply the muscles and skin of the posterior chest wall
The vast majority of paravertebral blocks are thoracic blocks.
You can technically do a paravertebral block at a cervical or lumbar level as well, however there isn't any reliable communication between each vertebral level in these areas, so you don't get nearly as much spread of local anaesthetic, and end up having to do multiple injections.
So most practitioners tend to stick to thoracic.
The block
This versatile block has several tricks up its paravertebral sleeves:
- It can be done uni- or bilaterally
- It can be a single shot or a catheter with repeated doses or infusion
- It can be done at a variety of spinal levels
- It can be done when epidurals cannot (e.g. coagulopathy)
So how does it work?
We don't really know.
We know that the bolus injection of local anaesthetic enters the paravertebral space and swills around the rami communicantes, the sympathetic chain and the intercostal spinal nerves.
However it's probably doing other things as well:
- Some is drifting medially into the epidural space, and acting as a low-dose thoracic epidural
- Some is spreading laterally to the intercostal space, adding a cheeky smidge of intercostal block into the mix
- Some of it slips north and some slides south to hit the vertebral levels above and below, usually two or three levels in each direction
Overall it doesn't really matter as long as the patient is comfortable and they don't have a raging pneumothorax.
What analgesia does a paravertebral block provide?
- Ipsilateral
- Segmental (depending on where you inject it)
- Somatic and sympathetic
It's useful for both acute and chronic pain originating from one side of the thorax or abdomen.
What are the advantages of paravertebral block over epidural?
- Similar pain relief
- Fewer neurological complications - PDPH, radicular pain, paraplegia, nerve palsy
- Less sedation, nausea and vomiting
- Less cardiovascular instability
- Much less urinary retention
- No motor block of lower limbs
- Better pulmonary function (as not bilateral) and fewer pulmonary complications
- Can still be done when an epidural is relatively contraindicated (coagulopathy, systemic infection)
What are the surgical indications for paravertebral block?
- Thoracotomy
- Sternotomy
- Breast surgery
- Renal and Ureteric surgery
- Cholecystectomy
- Orchidopexy
- Fundoplication
- Appendicectomy
- Hernia repair
Anything you might consider an epidural or spinal for, as long as it's only on one side, unless you're doing bilateral blocks.
What are the non-surgical indications for paravertebral block?
- Rib fractures
- Lung contusion
- Benign and malignant neuralgia
- Complex regional pain syndromes
- Hyperhidrosis (sympathetic block rather than pain control)
What are the specific contraindications to paravertebral block?
- Known malignancy in the paravertebral space
- Empyema
- Local infection over site of block
- Known significant kyphoscoliosis or other anatomical abnormality
- Complex or multiple thoracic surgical history that may distort anatomy
The Procedure
As with any regional anaesthetic procedure, you're going to start with the exasperatingly familiar exam answer of ensuring you have the following:
- Informed consent
- Correct site and side marked
- IV access
- Adequate monitoring
- Emergency resuscitation equipment and drugs
- Skilled assistance
What positioning options are there for this block?
- Sat up leaning forward (ideal)
- Prone
- Lateral
At what level should you perform the block?
- T4 for sternotomy (bilateral)
- T6 for thoracotomy
- T10 for abdominal procedures
For specific pain conditions, consider an injection at the dermatomal spinal level, plus further injections two spaces above and below.
Describe the landmark technique for a paravertebral block
- Mark 2.5 to 3 cm lateral to the spinous process
- Inject local anaesthetic
- Advance Tuohy (or similar catheter needle) perpendicular to the skin
- Contact the transverse process (usually around 4cm) and note that this is the transverse process of the vertebra below (because the thoracic spinous processes point steeply caudally)
- Walk the needle superiorly or inferiorly off the transverse process
- Use a loss of resistance technique, or advance at most 1.5cm to feel a pop as the superior costotransverse ligament is breached
- Aspirate and cautiously inject local anaesthetic
- Advance catheter (if used) to leave 2 to 3 cm in the paravertebral space
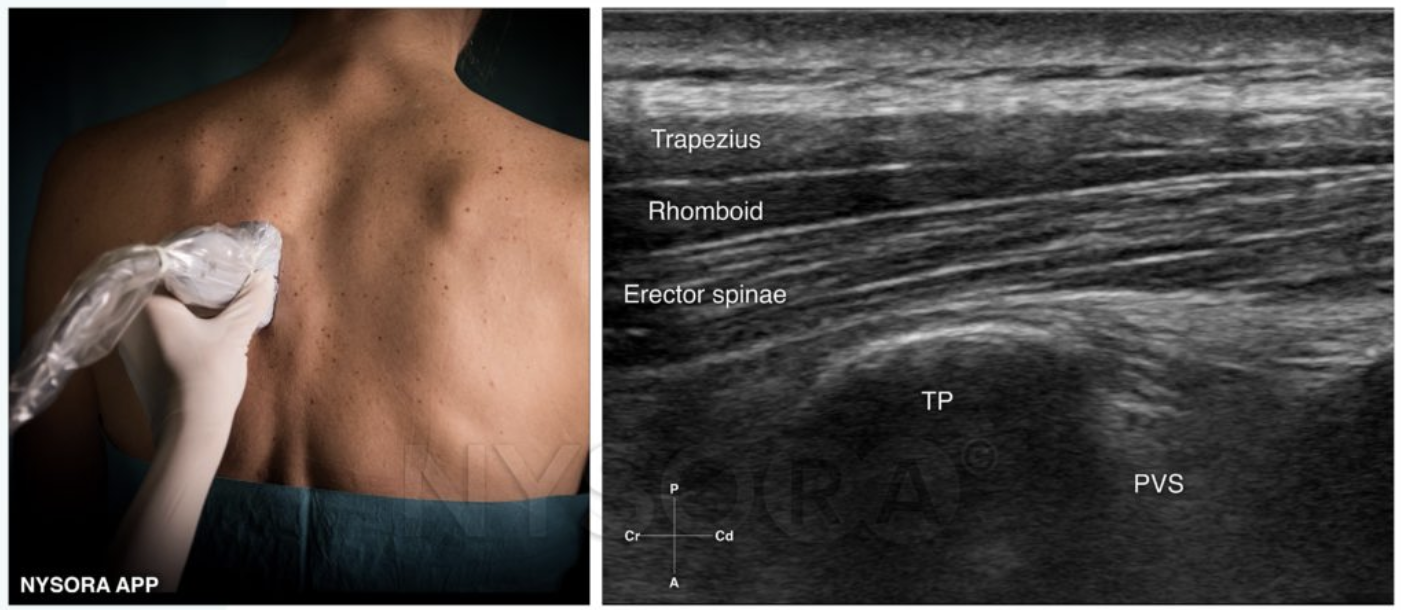
Describe the two commonly used ultrasound techniques
Longitudinal oblique
- In plane technique
- US probe is placed craniocaudal around 5cm from the midline
- Ribs and pleura identified
- Move probe medially until convex ribs change to square transverse processes
- Rotate probe slightly so that cranial end is more medial and tilt probe slightly laterally
- Advance needle in plane, caudally to cranially
- After breaching the superior costotransverse ligament with the needle, injection of local anaesthetic will displace the pleura downwards
You can visualise this technique in the NYSORA video below.
Transverse
- In plane technique
- US probe placed axially immediately lateral to midline
- Identify rib and move probe caudally to find intercostal space
- Visualise pleura and internal intercostal membrane
- This membrane is continuous with the superior costotransverse ligament
- Needle is advanced from lateral to medial towards the transverse process
- Visualise the pleura being pushed away
What are the advantages of using ultrasound?
- Lower risk of trauma to surrounding structures
- Greater confidence in location of needle, local anaesthetic and catheter
- Faster onset
- Longer block duration
- Smaller volume of local anaesthetic required
- Lower failure rate
- Fewer complications
- Improved patient comfort
What are the complications of paravertebral block?
- Failure (up to 5%)
- Damage to surrounding structures
- Pneumothorax
- Haemothorax
- Local anaesthetic systemic toxicity
- Intravascular injection
- Epidural injection
- Intrathecal injection +/- high spinal
- PDPH
- Stellate ganglion block if high thoracic
Here's NYSORA's awesome video
(Shared with permission as always)
Related SOE questions
What are the causes of pain after thoracotomy?
- Wound (incisional) pain
- Visceral pain via vagus nerve
- Referred pain to ipsilateral shoulder from diaphragm and pericardium
- Neuropathic pain from intercostal inflammation or nerve damage
- Chest drain pain via intercostal nerves
What levels do you need to block for a VATS procedure?
- T3 to T8 depending on exact operation site
What levels do you need to block for thoracotomy?
- Muscle sparing thoractomy is T2 to T9
- Posterolateral thoracotomy T3 to T8
As an example, to block T3-8, you'd probably need to do three injections, with up to 10ml at T3, T5 and T7 each.
What levels do you need to block for mastectomy?
- T1 to T6
Related posts
References and Further Reading