Paediatric Mediastinal Mass
Take home messages
- Keep them spontaneously breathing
- Positioning is seriously important
- Have a rigid bronchoscope (and someone to use it) ready
This topic was examined in the CRQ exam in:
Why is it a problem?
It might seem obvious that having a mass in the front of your chest isn't ideal, however you need to be able to explain the pathophysiology of why it isn't ideal.
The main concerns are twofold:
- Airway obstruction
- Cardiovascular compromise
Neither of which are much fun in a little one. Then add into the mix the metabolic strain of a potentially rapidly-growing malignancy, tumour lysis syndrome and super-added infection and you've got yourself quite the Sunday afternoon.
Both the airway obstruction and cardiovascular compromise occur as a result of compression of the trachea, bronchi and great vessels by an extrinsic mediastinal lesion and children - what with their spongy squeezy tubes - are much more susceptible to this compression than their sclerotic elderly counterparts.
As a result, you might find yourself anaesthetising a child for some such operation either to biopsy said lesion or remove it.
What causes it?
- Hodgkin lymphoma
- Non-Hodgkin lymphoma
- Acute lymphoblastic leukaemia
- Germ cell tumours
- Vascular malformations
- Teratomas
- Neurogenic tumours
How to anaesthetise them
MDT plan
- Anaesthetics
- Intensive care
- ENT
- Paediatric surgeons
- Cardiothoracics
- Oncology
- Patient and family
History
Aside from your usual anaesthetic history to determine their baseline anaesthetic risk, you want to explore their symptoms that might suggest significant intrathoracic airway or SVC compression.
- Cough when supine
- Orthopnoea
- Stridor
- Wheeze
- Syncope
- Upper body oedema
Imaging
CT is imaging modality of choice. You'll probably already have a chest xray as well.
- This can be tricky in a child that doesn't want to lie flat or still
- Might need to be lateral or prone
- Tracheal compression of >70% is high risk
- Pericardial effusion and great vessel compression also indicate high risk
Echocardiography can also be used to assess effusions, compression and ventricular function.
Spirometry is of variable use in demonstrating airway obstruction.
Anaesthetic considerations specific to mediastinal masses
- Keep the patient spontaneously breathing
- Ideally have IV access already in case you lose the airway during induction
- Sevoflurane inhalational induction
- Avoid nitrous - bone marrow suppression
- Avoid muscle relaxants - they reduce chest wall tone and predispose to airway collapse
- Be on the lookout for tumour lysis syndrome - check with oncology whether dexamethasone is appropriate
- Might be a good time to put a Hickman or equivalent in, as this kid is going to need long term IV access
- Glycopyrrolate to treat secretions from ketamine
- Midazolam to offset the bonkers from ketamine
- Wide awake extubation
Intraoperative considerations
- Positioning - head up, lateral, prone - depending on child's comfort*
- Blood loss - discuss transfusion beforehand, lots of IV access
- Airway management
- Duration of procedure
*Ask the child what position is most comfortable to lie in, so you know what position to move them into if you lose the airway - see below.
Local anaesthesia
Good luck doing anything with a distressed child awake under local anaesthesia, especially one with an obstructed airway who can't lie flat.
You can add in sedation:
- Ketamine - 1-2mg/kg then 0.5 mg/kg as required
- Dexmedetomidine - 1mcg/kg then 0.25-2mcg/kg/hour infusion
These maintain respiratory drive and cardiovascular tone while providing good analgesia and decent sedation.
The appropriateness of sedation and local as a plan is going to depend on the child and the procedure. It works well in a compliant slightly older child for a short peripheral biopsy.
If you lose the airway
This is clearly bad news, but there's a few things you can do to retrieve the situation:
- 100% oxygen - kinda goes without saying
- Reposition - head up, lateral, prone, anything to pull the mass away from the airway that it is currently occluding
- CPAP
- Try and restore spontaneous ventilation (tricky)
- Rigid bronchoscopy - this is most likely going to be ENT
What about if there's cardiovascular collapse?
Aside from your usual causes of haemodynamic compromise in an anaesthetised child, there's the added risk of compression-induced complete loss of right ventricular preload.
Things you can try:
- IV fluids
- Lighten anaesthesia
- Prone position
- Sternotomy to relieve the pressure*
*Please don't sternotomise a child by yourself, let someone with some surgical qualifications do it.
Can we use ECMO?
One can always try ECMO, however how much use it ends up being is debatable.
The two main issues neatly summed up are:
- Trying to pre-emptively cannulate an unsedated child is less than fun
- It takes too long to do it in an emergency
Post op
It goes without saying that a child who has undergone major thoracic surgery with high risk of airway obstruction should go to HDU or ICU.
It's not exactly day case surgery now is it?
Usually if the mass has been removed then the risk of airway and major vessel compression is removed with it, however there are always post op complications waiting to happen so it's far better to be vigilant.
Here's a related CRQ on paediatric stridor
From our wonderful colleagues at frca-revision.com
Useful Tweets and Resources
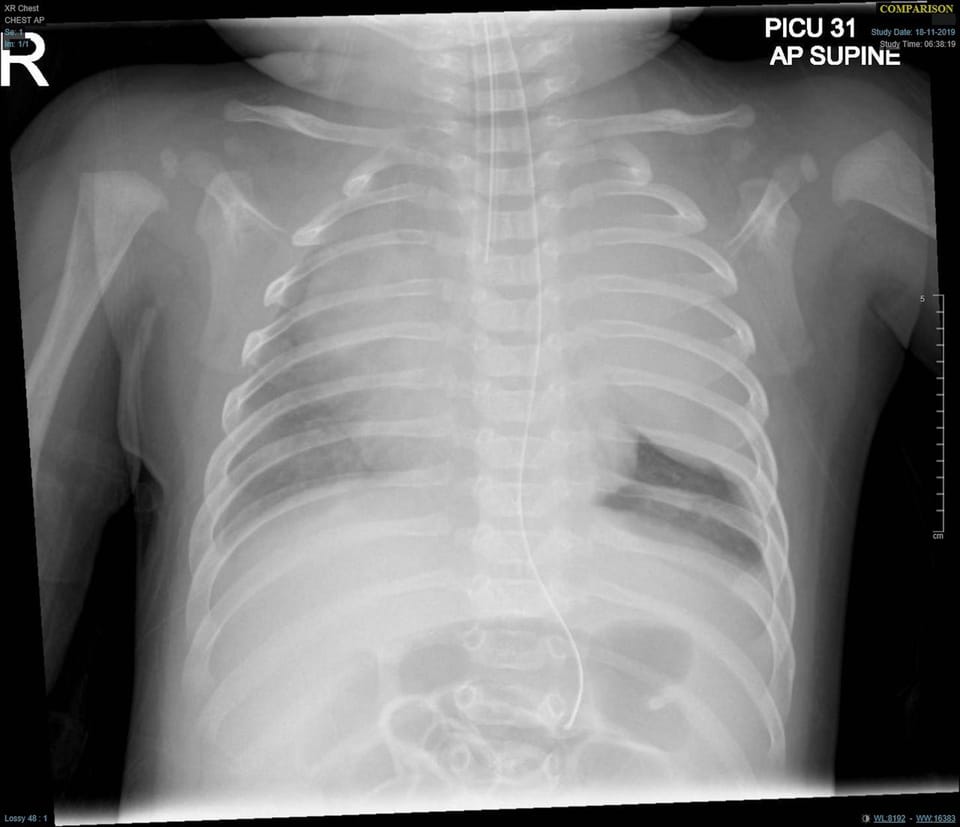
What is the diagnosis? For detail, read: Superior vena cava syndrome in an infant with large intrathoracic mass https://t.co/udy1DxSoC3 pic.twitter.com/mbJJMaQ0Em
— Igor Konstantinov (@konstantinov_ie) June 8, 2025
What rescue techniques can be used in a situation of airway or cardiovascular collapse in a paediatric patient with an anterior mediastinal mass?#BJAEducation paper on anterior mediastinal masses in children:https://t.co/OZbonDoZG8#PaedsAnaes #PedsAnes
— British Journal of Anaesthesia (@BJAJournals) January 22, 2019
References and Further Reading

Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
Anaestheasier® is a registered trademark.

