Airway Stenting

Take home messages
- Up to 30% of patients with lung cancer will develop central airway obstruction during the course of their disease
- Different materials, coatings and functionalities between stents determine how they behave and interact with surrounding tissue
- As the anaesthetist, you need to be able to adapt your plan to suit the procedure, patient and pathology as required
Podcast episode
It's all plumbing
When you think about it, a vast proportion of medical intervention is essentially some variation of plumbing, where an important tube is one of the following:
- Blocked
- Broken
- Leaking
The airway is no different.
If you have a blocked central airway, then one option, as with all tubes in the body, is a stent.
- By central, we're referring to the trachea and two main bronchi
These useful tubes can be employed for a variety of pathologies - malignant or not - for problems within the lung itself, and those caused by extra-pulmonary pathologies.
The idea of a stent is simple - it's a stiff tube that applies outwards force from inside the lumen of the tube, opening it up and relieving obstruction.
A spot of History
As far as medical history goes, airway stents are very young.
The first attempt at a stent for the airway was in the form of the Montgomery T-tube, crafted only in the 1960s, and it looks like this.
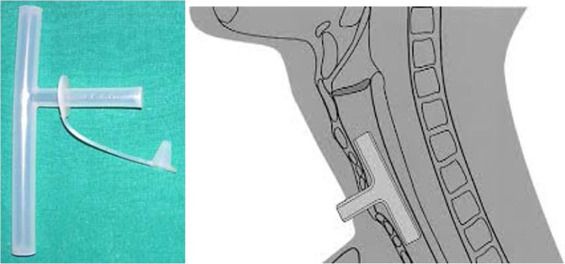
It's pretty good to be fair, and is still in use for subglottic stenosis.
It wasn't until 1987 when Dumon first brought a true endoluminal stent into play.
Types of Stent
You can categorise airway stents into different groups depending on:
- What they're made of (metal, silicone or both)
- How they work (fixed diameter, or self-expanding)
- Whether they're covered or uncovered
Covering materials
- Polyurethane
- Polytetrafluorethylene (Teflon)
- Silicone
This will affect how the stent interacts with the surrounding tissue.

Example stent names
- A - Hood stent
- B - Nova-Stent
- C - Polyflex
- D - Dumon bronchial stent
- E - Dumon hourglass tracheal stent
- F - Silmet stent
- G - Dynamic Freitag stent
- H, and I - patient-specific stents
It's important to know the differences because they behave in different ways, for example metal stents end up more deeply embedded into the tracheal mucosa, meaning they're more likely to stay in place and not migrate, but there is a greater incidence of tumour invasion.
Self-expanding stents can be inserted with a flexible bronchoscope, while others need a rigid scope.
In the future it's likely that there will be wider-spread use of biodegradable stents that don't need removal, they simply disappear over time.
Reasons to stent
As mentioned above, an obstruction to an airway can be due to an intraluminal obstruction, a mural pathology causing the wall of the tube to encroach on its internal diameter, or an extrinsic pathology causing compression from the outside.
Indications for airway stenting
- Neoplasia - Airway, oesophagus, thyroid, lung, metastasis
- Anastomotic strictures after lung resection or transplantation
- Airway stenosis after tracheostomy
- Tracheomalacia - acquired or congenital
- Mounier-Kuhn syndrome (tracheobronchomegaly)
- Asthma
- Emphysema
- Toxin exposure
- Chronic compression - goitre
Breast and lower GI cancers often metastasise to the airway. Most of the time, stenting for neoplasia is palliative, but can be very effective.
Before you begin
As you might expect, patients needing airway stenting often have complex and advanced disease, as well as their other comorbidities.
Often they're having a stent fitted because they're not able to undergo definitive resection.
As the anaesthetist, part of your job is to work out how best to adapt your plan to the patient's pathology, unique airway concerns and the operative requirements from the surgeon - whether they're going to need rigid or flexible bronchoscopy.
How would you prepare a patient pre-operatively for airway stenting?
- MDT management - anaesthetist, respiratory team, thoracics, radiology
- Oncology +/- palliative care team input
- Understanding of ceiling of care and treatment goals
- Informed consent, understanding of risks and benefits
- Appropriate imaging - Multi-detector CT with 3D reconstruction
- Understanding of what type of stent, and method of insertion (flexible bronchoscopy can be done under sedation)
- Adequate rescue planning for airway management should complete obstruction occur
- Optimisation of co-morbidities
- Lung function testing and Echocardiography are often helpful
This may be one of those times that you whip out the old jet ventilator.
If you can't ventilate or oxygenate adequately, remember ECMO is there as a back up option, and should ideally be available at short notice.
Losing the airway
Clearly this is your primary concern in an airway stenting case.
Yes the cardiovascular physiology, renal bits and bobs and pain control remain as important as ever, but this is a uniquely dangerous situation when it comes to risk of losing the airway completely.
Your job is to be adaptable and to anticipate the possibility of complete airway obstruction, as well as what you're going to do about it.
Conscious sedation vs General Anaesthesia
If the stent can be inserted using a flexible scope, then it's likely that conscious sedation (plus airway topicalisation) will suffice, and you have that extra layer of safety in that the patient will generally manage their own airway.
You can add in THRIVE for good measure if you like.
But if the patient needs rigid bronchoscopy then you're most likely looking at a general anaesthetic, and a deep plane of anaesthesia at that. This causes relaxation of the respiratory muscles including trachealis, particularly if muscle relaxants are used.
This could mean complete airway obstruction soon after induction, so it's sensible to induce in theatre, with your surgeon on standby with the bronchoscope for airway rescue if needed.
Pain control and complications
Generally patients don't suffer too badly with post-operative pain, and hopefully their breathing is at least a little easier with their newly-stented airway.
One thing to be cautious about is any respiratory distress or insufficiency, as this might represent stent failure.
The stent could have:
- Migrated
- Obstructed
- Broken
And it's easy to attribute respiratory failure in recovery to the lasting effects of anaesthesia, rather than immediately thinking of complications of the procedure itself, so it pays to keep your wits about you.
Other complications of airway stenting
Early complications
- Airway obstruction
- Trauma due to bronchoscopy
- Barotrauma from ventilation
- Bleeding
- Air embolism
- Pneumothorax and tension pneumothorax
- Hypoventilation and hypoxia
Late complications
- Stent migration
- Stent breakdown
- Stenosis
- Erosion into surrounding tissue
- Chronic infection
- Granuloma formation
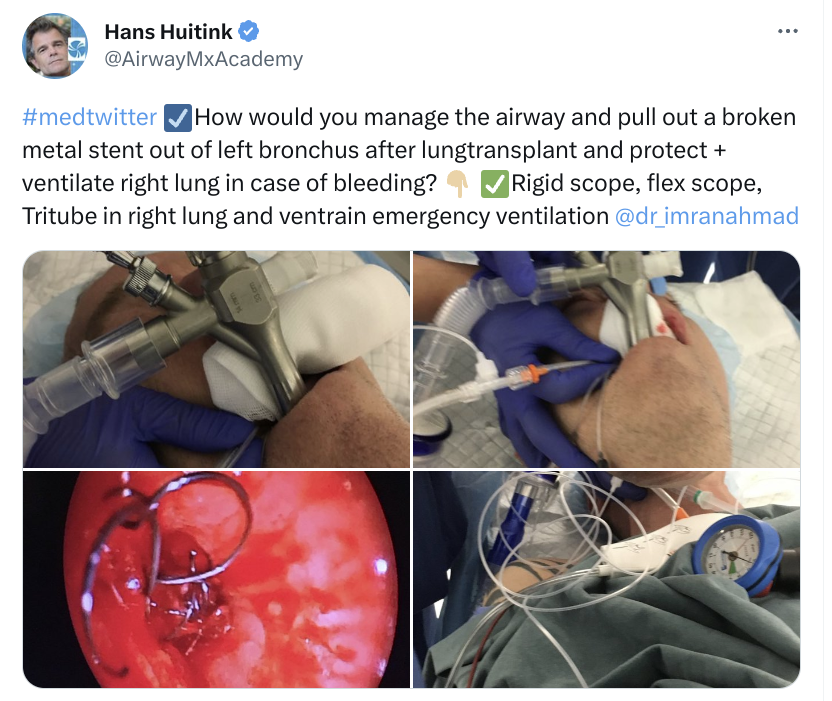
Useful Tweets and Resources

References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.