Oxygen and Face Masks

Given these are the some of the simplest pieces of lifesaving airway equipment that we use very pretty much every day, we're taught remarkably little about the nuances of facemasks - and other oxygen delivery devices - and why we have all of these different types for different scenarios.
In this post we go through the commonest types and explain why they exist and when to use them.
"Why do you talk about percentage oxygen, but on the ward we talk about litres of oxygen?"
Variable vs Fixed
These terms are thrown around and not hugely well understood, so we thought we'd go over it quickly here.
Fixed
A fixed oxygen delivery device gives a set, known oxygen concentration or FiO2 (Fraction of inspired oxygen), and we generally express this as either a percentage (45% FiO2) or as a decimal (0.45).
These devices are either part of a breathing system where the oxygen concentration can be measured and controlled, such as with an anaesthetic machine, or they provide very high flows of known oxygen concentration, such as a venturi mask.
Fixed performance devices
- Venturi masks
- High flow nasal oxygen
- CPAP and Non-invasive ventilation
- Invasive ventilation
Variable
A variable oxygen delivery device gives a set volume of oxygen per minute, but the actual concentration received by the patient's lungs depends on many other factors, such as
- Their breathing pattern, respiratory rate and depth
- whether they're breathing through their nose or mouth
- whether they're actually keeping the mask on at all
As a result, for these devices we generally talk in terms of flow rate of oxygen in litres per minute supplied to the patient. Clearly the more litres per minute, the higher the % oxygen concentration, but the variability means you can never be sure exactly how much they're getting.
Variable devices
- Nasal cannulae
- Simple (Hudson) mask
- Non-rebreathing mask
Most of the time, a variable device is absolutely fine to use, because you can just adjust the volume per minute of oxygen supplied to target the patient's oxygen levels.
However if you have a critically ill patient, or a patient with a specific respiratory disease that means they need careful titration of their oxygen levels, you'll want to use a fixed performance device.
Variable devices
Nasal Cannulae

The simplest way to give a patient oxygen, these little plastic tubes sit at the entrance to the nostrils and enrich the inhaled air with up to 4 litres per minute of oxygen, up to a maximum of around 30% oxygen.
Benefits
- Cheap
- Simple
- Easily available
- Generally well tolerated by patient
- Patient can eat, drink and talk
Downsides
- Cool and dry the nasal mucosa causing pain and bleeding if used at more than 4 litres per minute or for a very long time
- Can cause discomfort
- Very variable oxygen delivery, especially if patient mouth breathes
- Frequently found halfway up patient's forehead or in ears
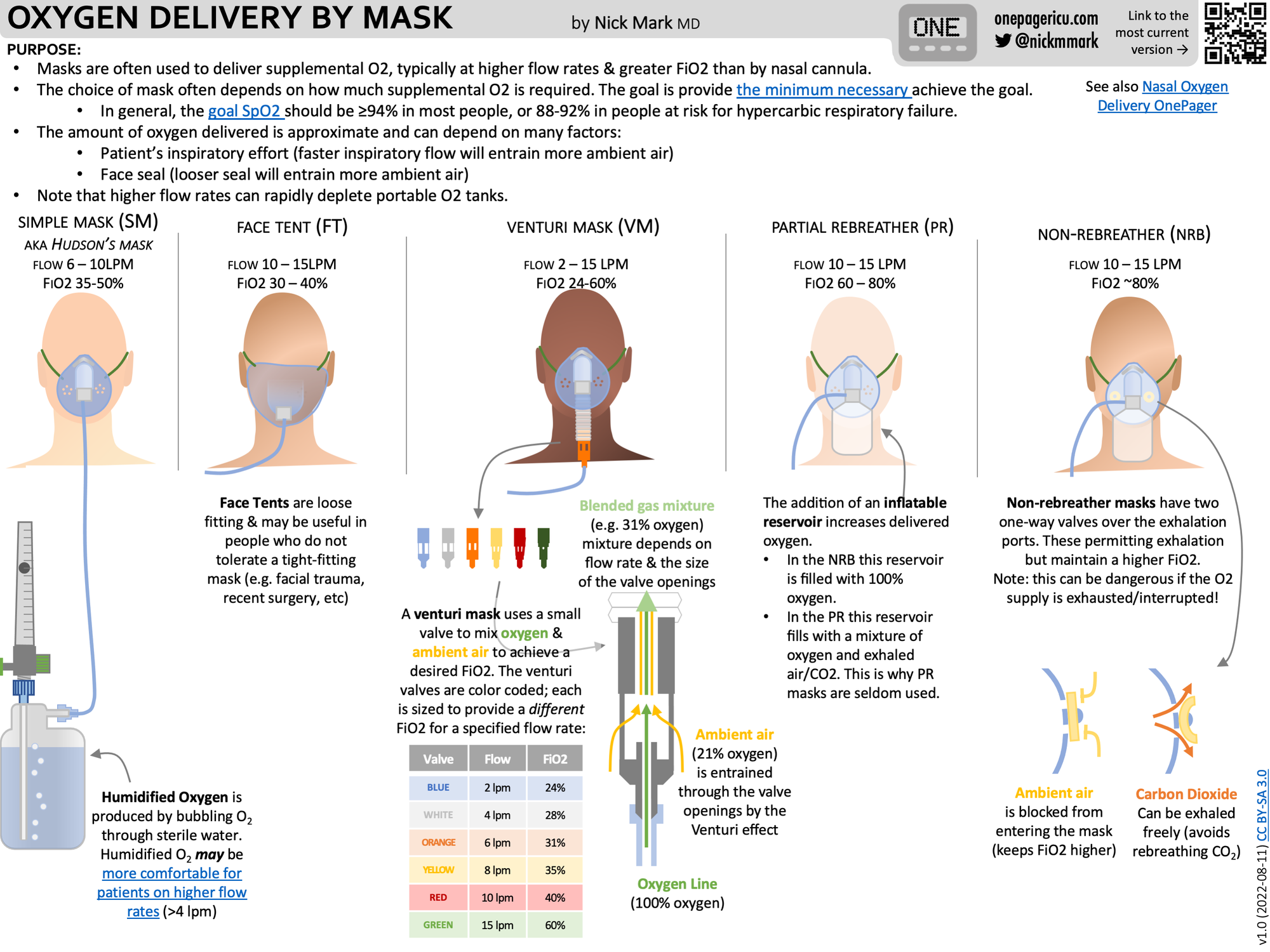
Standard Face Mask (Hudson)

This is what we generally refer to when we say a 'facemask' - it's the basic version of the device found on most wards.
- Simple and easy to use, it's a great way to quickly give oxygen to an unwell patient
There are however two downsides:
- Rebreathing
- Variable oxygen delivery
Rebreathing
- Much like a paper bag, if you have an enclosed mask over your face and exhale into it, when you next inhale, some of that gas is going to get drawn back into your lungs
- To counter this, the mask has little holes on the side to allow exhaled gas to escape
- There is also a fresh gas supply, via the little plastic tubing, that connects to the oxygen supply, which replaces the exhaled gas in the mask and helps to push it out through the holes
- If the fresh gas flow is less than 5 litres per minute then there will be significant rebreathing, so these masks should be used with at least 5l/min flow
If the patient has an enormous respiratory rate, however, then their exhaled gas is likely to get drawn back in again before it has a chance to be flushed out, so there will be some rebreathing even if high oxygen flows are used.
Variable oxygen delivery
- You can pipe up to 15 litres per minute through the plastic tubing to the mask - this is 100% oxygen
- However when a patient inhales, the inspiratory flow can be up to 50 litres per minute
- These extra 35 litres are supplied by the surrounding room air, which is sucked in or entrained through the holes in the mask, and therefore dilutes the oxygen supply
- The faster the patient's breathing, the greater this effect, and the lower the overall oxygen concentration
That being said, these masks are a useful initial therapy for an unwell patient until a more comprehensive plan is in place, so don't be afraid to pop one on - just make sure you supply at least 5 litres per minute!
Non-Rebreathing Mask

You'll notice some similarities to the standard Hudson facemask, with the addition of a bag, and the replacement of the small holes on the side with flap valves.
This bag fills up with fresh oxygen, and the idea is that when the patient inhales, there is enough oxygen in the bag and coming through the piping to supply the patient's inspiratory flow, with minimal room air being entrained and diluting the oxygen.
The flap valves then allow the exhaled gas to escape, without letting room air in.
It remains a variable performance device, however as there is not a completely tight seal around the mask, so some room air does inevitably get drawn in, and you can't be sure of the exact percentage oxygen concentration being supplied.
Equally, despite the name, there will always be an element of rebreathing at very high respiratory rates, albeit small.
That being said, they're a lot better than the standard masks, and reliably supply up to approximately 80% oxygen, so definitely use them for a sick patient if you have one to hand.
Fixed Devices
Venturi Mask

The venturi effect is weird.
We've explained it here:
@anaestheasier Bernoulli's principle in 60 seconds #bernoulli #venturi #medicine #FOAMed #TipsForNewDocs #FiY1 #medschool #anaestheasier #anaesthetics #novice #anaesthesia #revision #pharmacology #FRCA #anesthesiologist #anaesthesialife #anesthesialife #odp #studentodp #emergency #crna #student #surgery #or #nurse #theatre #physics
♬ BARELY BREATHING - Grant Averill
The entrainment ratio is the key feature here. The blue nozzle only requires 2 litres of oxygen per minute, because it has an entrainement ratio of 25:1, so for each litre of oxygen, it drags 25 litres of room air with it, meaning a total flow delivered to the patient of 50 litres per minute.
Because this is higher than the patient's inspiratory flow rate, no extra room air is dragged along for the ride, and you can be sure that the patient is receiving 24% oxygen.
What flows and oxygen concentrations are supplied by each venturi mask?
- Blue (2 - 4 l/min oxygen) - 24% oxygen at 50 - 100 l/min
- White (4 - 6 l/min) - 28% oxygen at 44 - 66 l/min
- Yellow (8 - 10 l/min) - 35% oxygen at 45 - 65 l/min
- Red (10 - 12 l/min) - 40% oxygen at 40 - 50 l/min
- Green (12 - 15 l/min) - 60% oxygen at 24 - 30 l/min
Note that because each nozzle has a certain entrainment ratio, if you put, a greater initial flow of oxygen through it, it will drag more air in and still give the same concentration of oxygen, just with a total flow.
If you want to increase the oxygen concentration, you have to change the nozzle.
This is useful when you want to titrate a specific oxygen concentration, such as in the case of COPD or other advanced respiratory disease where you don't want to give too much oxygen.
CPAP and NIV
CPAP (continuous positive airway pressure) and NIV (Non invasive ventilation - aka BIPAP - bi level positive airway pressure) are similar but technically different techniques, and we've explained it in our video below.
Many patients have CPAP machines at home for management of obstructive sleep apnoea. The extra airway pressure helps hold the upper airway at the back of the mouth and nose open, and prevents the snoring and airway obstruction that's causing the problem.
Key points:
- Tight fitting mask forms a closed system - the patient cannot breathe any extra room air in
- This allows a fixed concentration of oxygen to be delivered, with the added benefit of pressure to help open up the airways
- In the case of BiPAP or Non-invasive Ventilation, there is also an inspiratory pressure that provides ventilatory support to the patient as well
High flow nasal oxygen
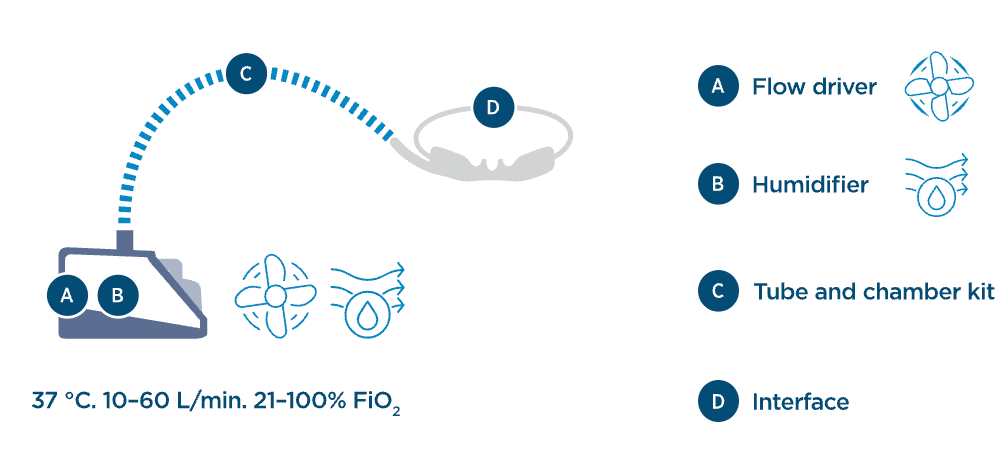
Also known by brand names such as Optiflow, or specific anaesthetic techniques such as THRIVE (Transnasal humidified rapid-insufflation ventilatory exchange), High flow nasal oxygen is the big brother to nasal cannulae, with the following advantages:
- Warmed and humidified air prevents cooling and drying of respiratory tract
- High flow provides up to 5cmH2O of positive end expiratory pressure (PEEP - see our video here)
- High flow ensures fixed delivery of known concentration of oxygen up to 100% FiO2
If you'd like to learn more about HFNO in anaesthesia and intensive care, check out this tutorial of the week
So which should I use for my patient?
Don't overthink it to start with, if a patient is hypoxic then just give them some oxygen with what you've got available.
- If they're acutely desaturating then put a facemask on (ideally non-rebreathing) with 15 litres of oxygen and call for help
- If they're just needing a little top up of oxygen because they've got a nasty pneumonia, start with nasal cannulae and adjust as needed
- If they've got type II respiratory failure with a rising CO2 level, think about BiPAP (This will likely need intensive care or critical care outreach team invovlement, so let them know!)
A super useful infographic from Dr Nick Mark
References and Further Reading

