NAP 3
Take home messages
- Neuraxial blockade is safe, if you do it correctly, in the right patients
- The key to dealing with complications is early detection with proper monitoring
- As always, informed consent is very important
Central neuraxial blocks
Spinal anaesthesia will never not be absolute magic to me.
The idea that two millilitres of clear fluid can temporarily switch off the spinal cord is frankly bonkers, and I have the utmost respect for the pioneers that decided that injecting cocaine into their spine before sats monitors existed was a good plan.
"Hello, I know we've only just met, but my plan is to put a large needle really rather close to your spinal cord, and inject a drug that will make you paralysed and numb from the waist down, but I'm 99.999% certain it'll wear off and you'll be absolutely fine."
Central neuraxial blockade is rather terrifying if you think about it. But then again, lots of anaesthesia is rather terrifying if you think too much, so let's not dwell too much, and rather focus on how to do it properly.
The two main ways to perform central neuraxial blockade are:
- Epidural
- Spinal
And the only real difference is how deep the needle goes.
An epidural usually results in a thin plastic catheter being left in the epidural space, allowing a continuous infusion or top-up doses to be given, meanwhile a spinal anaesthetic usually involves a single injection into the cerebrospinal fluid in the subarachnoid space.
Of course, you can also put a catheter into the subarachnoid space, and indeed many countries do this on a regular basis, however it's less commonly used in the UK (the main reason being accidentally inserting the epidural needle a smidge to far during a labour epidural)
A classic OSCE/CRQ question
What are the boundaries of the dural space at the L3/4 vertebral space?
- The epidural space is a continuous, potential space that extends from the foramen magnum of the skull superiorly to the coccygeal membrane inferiorly, and its boundaries can be identified as anterior, posterior and lateral
Anterior
- Posterior longitudinal ligament, vertebral bodies and intervertebral discs
Posterior
- Ligamentum flavum and laminae
Lateral
- Pedicles and intervertebral foraminae
What layers would your needle pass through?
- Skin
- Subcutaenous fat
- Supraspinous ligament
- Interspinous ligament
- Ligamentum flavum
- Epidural space (stop here for epidural)
- Dura
- Arachnoid
- CSF
Just because life isn't stressful enough, it is possible to get a subdural block as well, if you get unlucky enough that your needle peels the arachnoid and dura matres apart.
And yes - matres.
Is it safe?
You can tell by the look on some patients' faces when you introduce them to the concept of a needle near the base of their spinal cord, that there is clearly some risk, and therefore potential for serious harm.
There are also many potential benefits:
- Avoiding risks of general anaesthesia
- More rapid recovery
- Better post operative pain relief
- Quicker mobilisation
- Reduced post operative delirium
"Why am I itchy?"
"Ah yes, that'll be the heroin."
While exceedingly effective and generally considered very safe, it was clearly a sensible idea to formally study the procedures we're performing and work out if we're missing anything, and where improvements can be made.
Enter NAP3
The Third National Audit Project, on behalf of the RCoA, aimed to study the "Major Complications of Central Neuraxial Block in the United Kingdom", and was conducted by Dr Cook et al. over the course of 2009.
It was a big study, involving over 300 UK hospitals, and represents an enourmous and very important piece of work that will guide anaesthetic practice for years to come.
What questions did NAP3 aim to answer?
- What neuraxial procedures are we doing in the UK and how much?
- How often are there problems with permanent consequences?
- What happens to these patients?
The main aim of this project was to assess the incidence of permanent harm as a result of an anaesthetic needle inserted near the spinal cord, so remember it won't necessarily completely account for the complications, both minor and major, that were temporary in nature.
Over 700,000 needles were introduced to the ligamentum flavum.
- 46% spinal
- 41% epidural
Just under half (45%) were obstetric.
Over the entire year, from 700 000 procedures, there were 84 major complications, and potentially 30 permanent injuries as a result.
Did anyone die?
According to the authors of the study:
- ‘Pessimistically’ there were 13 deaths or paraplegias,
‘optimistically’ five - The incidence of paraplegia or death
was ‘pessimistically’ 1.8 per 100,000 (1.0–3.1) or 1 in 50,000
and ‘optimistically’ 0.7 (0–1.6) or 1 in 140,000.
In the 30 patients with permanent harm:
- 60% occurred after epidural block
- 23% after spinal anaesthesia
- 13% after CSE
More than 80% of these patients had a CNB placed for perioperative analgesia.
- Over 60% of those with injuries deemed severe at the time saw complete resolution of the problem.
This meant a risk of permanent injury somewhere between 1:24 000 and 1:54 000
What are the complications of epidurals?
The following were the main complications as detailed in the NAP3 audit project
- Failure to work - 1 in 20 will require resiting
- Hypotension - 1 in 50
- Headache - 1 in 150
- Nerve damage - Temporary 1 in 2000, Permanent 1 in 15 000
- Epidural Abscess - 1 in 50 000
- Meningitis - 1 in 100 000
- Paralysis - 1 in 250 000
How common are vertebral haematomas after CNB?
- Incidence of vertebral canal haematoma after neuraxial blockade was 0.85 per 100 000
What are the contraindications to performing an epidural?
As always, the key is to categorise your answer - and for any contraindications questions, you should always mention that these can be absolute and relative
Absolute
- Patient refusal
- Allergy to local anaesthetic
- Raised intracranial pressure
- Local infection over injection site
- Severe systemic sepsis*
- Neurological problems with the spine such as spina bifida
- Inability to monitor safely
Relative
- Previous neurosurgery or spinal deformity
- Severe cardiovascular disease such as aortic stenosis that won't tolerate a drop in systemic vascular resistance
- Clotting problems
- Anticoagulant medication
- Coagulopathy
- Low platelets
*There is much debate about what constitutes 'systemic sepsis' that is severe enough to contraindicate neuraxial procedures. We're probably too cautious, especially when you consider the fact that a lumbar puncture is often a standard part of a sepsis workup, particularly in paediatrics.
Key Findings and Recommendations
The following points are from the NAP3 executive summary which can be found below.
- Two-thirds of patients with complications reported to the project made a full recovery
- Patients with vertebral canal haematoma and spinal cord ischaemia had a poor prognosis, with most patients being left with significant disability after these complications
- The incidence of complications in children, and after CNB for chronic pain or obstetric indications seems to be extremely low
- The majority of complications after perioperative CNB occurred after epidurals
- Perioperative epidurals represent approximately 1/7 of all CNB, but accounted for more than 50% of complications leading to harm
- Combined spinal epidurals seem to be disproportionately harmful
- Several reported cases illustrate that failure to identify and understand the relevance of inappropriately weak legs (including unilateral weakness) after CNB or during continuous postoperative CNB can lead to avoidable harm.
- Delays included failure to monitor, poor understanding of abnormal findings (by nurses and doctors), poor interdepartmental referral processes, scanning equipment which was routinely unavailable out of hours or broken, and lack of availability of beds in tertiary referral centres for patients requiring specialised emergency surgery.
- A care bundle for CNB might usefully be developed
Overall central neuraxial blocks, when performed correctly, are pretty damned safe.
Many of the issues that arose as a result of poor monitoring or preparation are potentially preventable, which provides an immediate avenue for improvement.
Useful Tweets and Resources
As always we have scoured social media for useful bits and bobs to help your learning, and here's what we've found.
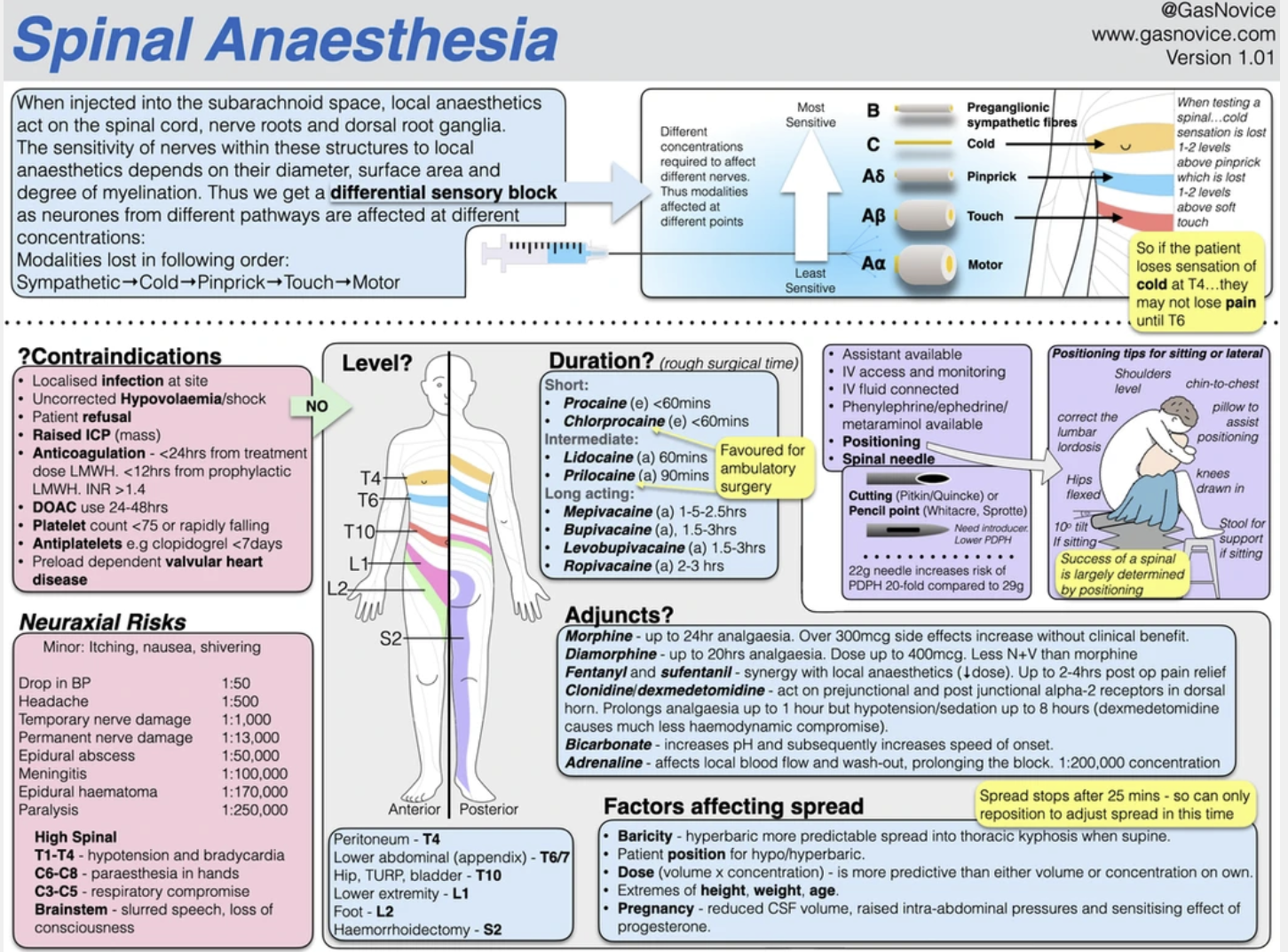
A great infographic
Here is a brilliant infographic from Chris Hellyar, click the image to go to the full resolution version on his website - embedded with permission here:
NAP 3 executive summary
This pdf is the executive summary of NAP3, freely available from the NAP website here, posted again here for your convenience, with permission from the authors.
If in doubt - NYSORA
There really isn't any beating NYSORA when it comes to teaching regional anaesthesia, so be sure to subscribe to their channel and watch literally everything they've ever made - you won't regret it.
A Final CRQ
Here's a CRQ for the Final FRCA written paper on the topic of wrong sided blocks from the lovely people at FRCA-revision.com
References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.

