Capnography
Take home messages
- Capnography provides useful information about airway, breathing and circulation
- It's important to understand how it works, so that you can fix it when it goes wrong
- No trace, wrong place - take the tube out and try again
Why do we care about CO2?
There's not a whole lot of CO2 in atmospheric air, (hopefully).
CO2 is produced as a metabolic waste product by the tissues, and then carted off by the blood to the lungs, where it is dumped into the alveoli and hopefully exhaled out into the atmosphere.
It can't come from anywhere else in the body.
This means that if you put a CO2 sensor on the end of an endotracheal tube, and that sensor is detecting a rise and fall in CO2 concentration in time with the patient's breathing, then the endotracheal tube must be connected to the lungs, and therefore you can be pretty certain it's in the right location.
(Unless the patient has just downed a litre of Sprite - in which case you will briefly detect CO2 from the oesophagus, but it won't last for more than a breath or two...)
No trace, wrong place
If you have just intubated a patient, and you don't see a reassuring CO2 trace on the monitor, the safest thing to do is to take the tube out and re-intubate, even if clinically you think the tube is in the trachea.

How it works
- Capnometry is the measure of CO2 in exhaled gas
- Capnography is the display of this information as a waveform on the monitor
Most modern anaesthetic machines use infrared spectrometry to measure end-tidal CO2. Any molecule with two or more different atoms will absorb infrared radiation at a characteristic wavelength, which is useful.
For CO2 the magic wavelength is 4.3μm
Now, the Beer-Lambert law states that the degree of absorption is proportional to both the concentration of the gas, and the distance the light has travelled.
- Beer = concentration
- Lambert = distance
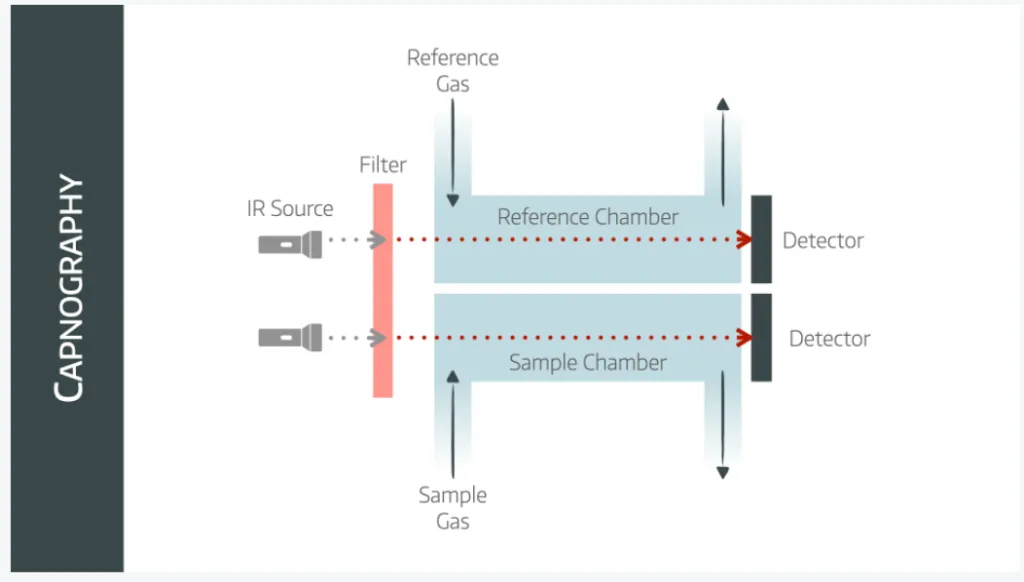
The emittor produces infrared light that passes through a sapphire lens that conveniently only permits 4.3micrometre wavelength light through.
This then passes through a test chamber and a reference chamber to a detector.
A microproccessing unit then compares the two samples and deduces the concentration of CO2 in the test chamber.
Clever stuff.
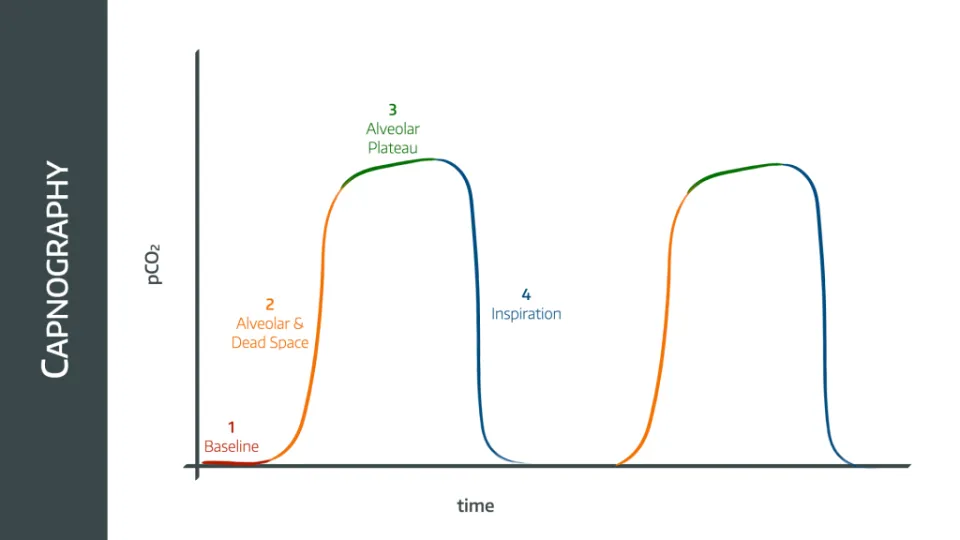
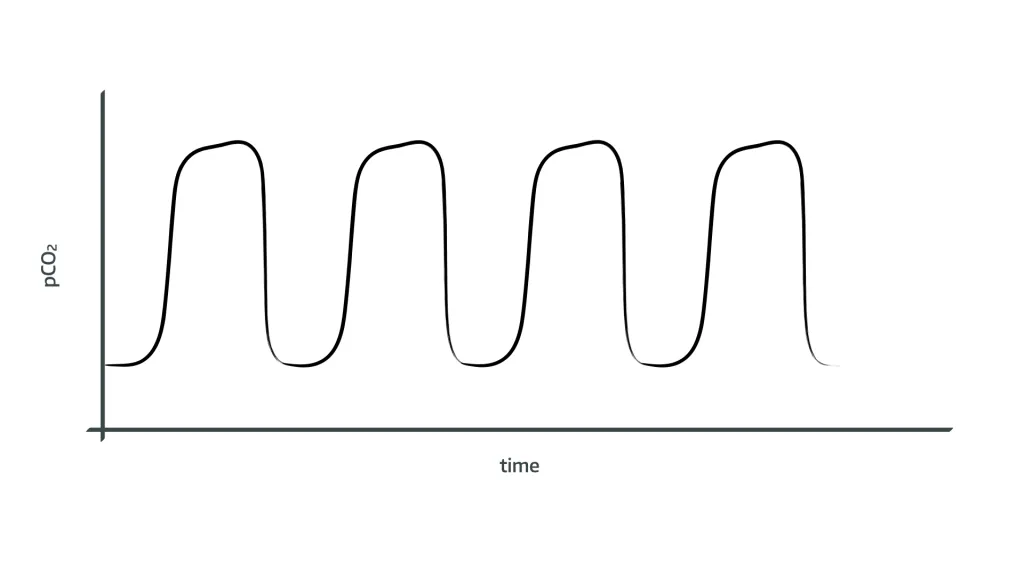
A Normal ETCO2 Trace
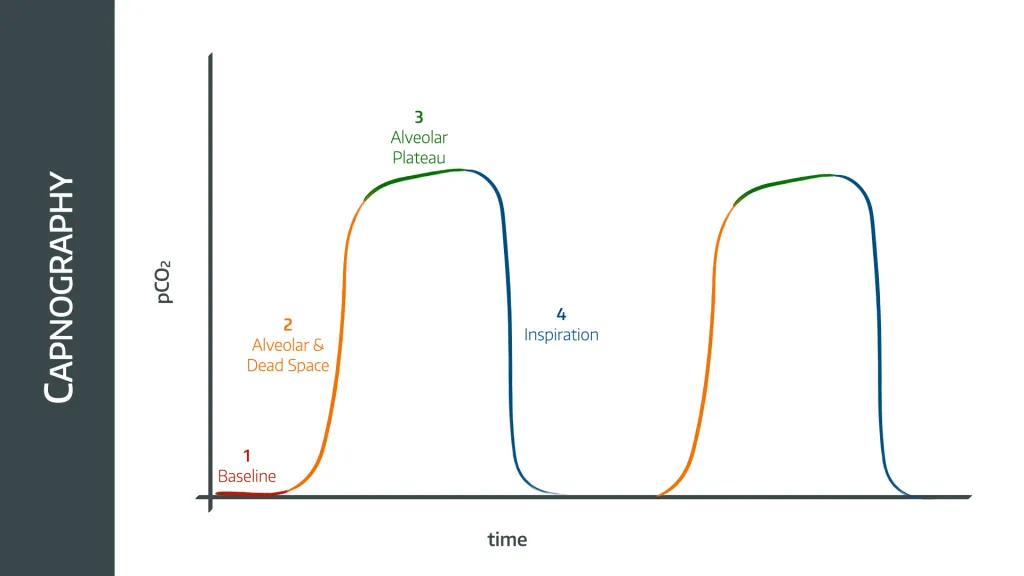
- During inspiration (phase 4), the CO2 sampling line detects the fresh gas flow as it flows into the lungs. This hopefully contains no CO2, and so the graph rapidly drops to zero
- As the patient then exhales, the first part of the exhaled gas is from the trachea and upper airways that are not involved in gas exchange (dead space), so this has no CO2 either (end of phase 1)
- As exhalation continues, gas from the alveoli with the shortest time constants (meaning the ones that empty first) begins to reach the sampling line, mixed together with the dead space gas from other areas in the lung, and the concentration of detected CO2 starts to rise (phase 2)
- As more alveoli empty, the CO2 level rises until it reaches a plateau (phase 3)
- At this point there is no dead space gas remaining, and only alveolar gas emptying into the circuit
- Those alveoli with the longest time constants will have picked up slightly more CO2 during this time, and therefore will have a higher concentration of CO2, meaning the plateau is not quite flat
- This continues until the next inhalation
- The peak ETCO2 is measured at the end of phase 3
What is happening here and what should be done about it?
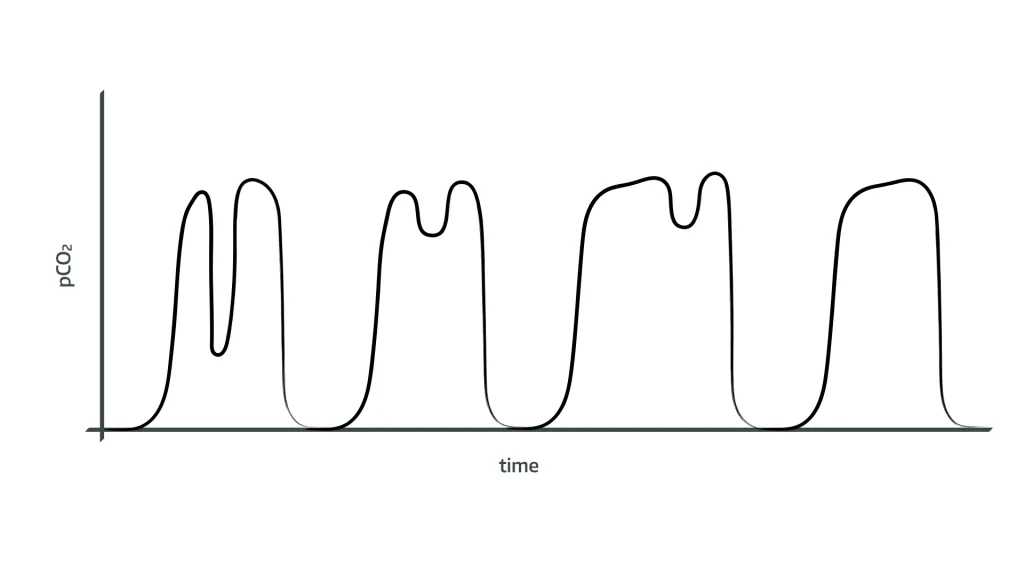
- The patient is starting to make their own respiratory effort, causing dysynchrony with the ventilator
- Either switch off the ventilator and allow patient to breathe spontaneously
- Or administer sedation, opiates or muscle relaxation if not wanting patient to breathe spontaneously
- The respiratory rate on the ventilator can also be increased to lower the PaCO2, and reduce the respiratory drive to stop the patient from breathing
What does rebreathing look like on the end tidal CO2 trace?
- Trace appears normal in shape
- Consistently raised baseline and raised peak ETCO2 because the patient is inhaling CO2, that was previously exhaled, and then adding more to it
- This will steadily climb unless something is done about it, either by increasing fresh gas flow or replacing the soda lime in the breathing circuit
What does airway obstruction look like on the end tidal CO2 trace?
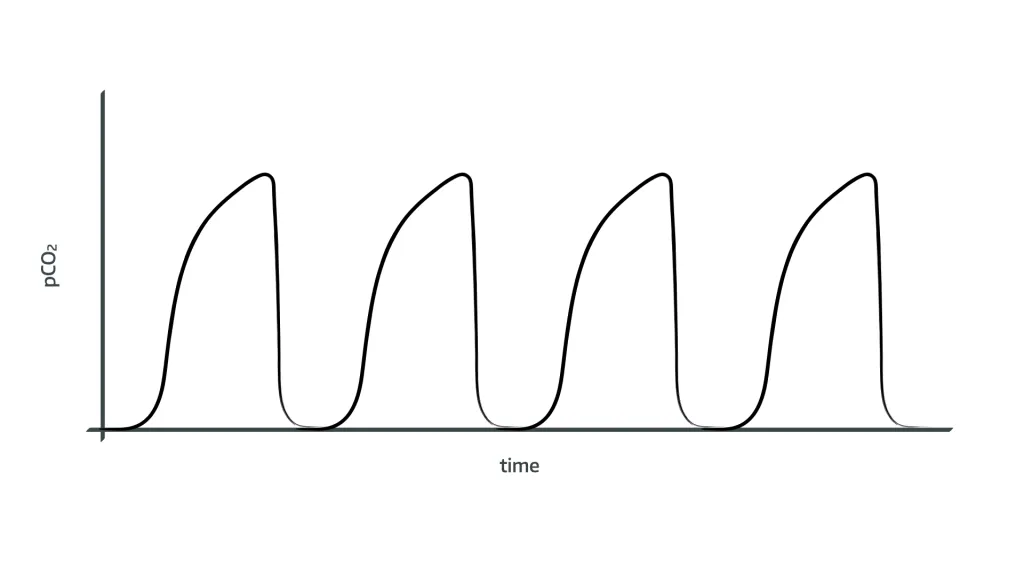
- Upward sloping plateau phase as CO2 takes longer to drain from obstructed small airways
- May also have higher peak if CO2 is being retained and PaCO2 increasing (severe bronchospasm)
What might cause a rapid loss of end tidal CO2 trace?
Thinking about this logically, if no CO2 reaching the detector, then one of three things has happened:
- Either there is circulatory failure, and CO2 is not reaching the lungs
- Cardiac arrest
- Profound Shock
- Massive pulmonary embolism
2. Or there is ventilatory failure, and CO2 is not leaving the lungs
- Airway obstruction
- Bronchospasm
3. Or there is an equipment issue, and CO2 is not reaching the analyser
- Disconnection of breathing circuit
- Kinking of sample tube meaning gas not reaching analysing chamber
What might be the the cause of a low end tidal CO2?
Again, this can be a patient problem or an equipment problem, similar to the question above, but not to same severity. Possible causes include:
- Reduced ventilation
- Airway obstruction
- Bronchospasm
- Reduced cardiac output
- Excessive fresh gas flow
What might be the cause of a high end tidal CO2?
If too much CO2 is reaching the analyser then either the patient is producing too much, or its being allowed to accumulate in the patient by inadequate ventilation, or it's not being cleared out of the breathing circuit effectively.
- Inadequate ventilation
- Tidal volume or respiratory rate too low
- Excessive dead space
2. Increased CO2 production
- Sepsis
- Malignant hyperthermia
- After deflating tourniquet
- ROSC
3. Rebreathing of CO2
- Exhausted Soda lime
- Inadequate fresh gas flow
- Circuit failure eg inner tube dislocation in Bain Circuit
What are the two different types of infrared capnography?
This is a common Primary FRCA question so it's worth understanding the different types and their respective advantages and drawbacks.
Sidestream and Mainstream
Sidestream analysis draws 150 ml/min from the main breathing circuit near the patient end via a long thin clear plastic tube. It needs a water trap to prevent interference from water molecules and has an exhaust port to return the gas to the circuit after analysis.
- Benefits are that the circuit is lighter, and the expensive delicate components are protected within the anaesthetic machine
Mainstream analysis meanwhile needs a bulky sampling chamber attached directly to the breathing circuit at the patient end.
- Needs heating to 41ºC to avoid water condensation
- Technically more accurate, and faster, but not used much for the above reasons
What are the problems with infrared spectroscopy?
Don't get me wrong - infrared analysis is very good, but as with all monitoring, it's not flawless.
Collision broadening
- Molecules that are in close proximity will exert forces upon one another that can change their respective energy levels and have a ‘blurring’ effect on the wavelengths absorbed, giving alterations in the amount of light received by the detector
Nitrous Oxide
- If there is nitrous oxide present in the sampling chamber, CO2 can transfer some of the absorbed energy to the nitrous molecules, and then absorb some more, thereby giving a falsely high absorption reading, and overestimating the CO2 concentration
- Nitrous also has a similar absorption wavelength (4.5 micrometres) to CO2 but most machines have compensation mechanisms in place for this
Variation in emission and detection of infrared radiation by equipment
Double beam analysers usually employ a reference chamber that contains no CO2, which allows subtraction of artefact signals, thereby correcting for
- The amound of IR radiation emitted
- The sensitivity of the detector
- Changes in the lens behaviour
Water and alcohol can cause interference
So either the gas is dried, or a specific wavelength chosen away from water’s maximal absorption frequency is used
Some common Primary FRCA OSCE questions
What are the five components of an infrared CO2 analyser?
- Sapphire Sampling/Reference Chamber (sapphire only allows light of wavelength 4.28μm)
- IR Source / Emitter
- Detector
- Microprocessor
- Display
What information does capnography tell you in a cardiac arrest?
- Confirms airway location and patency
- Respiratory or ventilatory rate
- Assess quality of CPR
- Identifying ROSC
How else can you measure CO2 in a gas sample?
- Photoacoustic spectroscopy
- Piezoelectric absorption
- Refractometry
- Raman scattering
- Mass Spectrometry
How does an infrared CO2 analyser work?
- The emittor produces infrared light that passes through a sapphire lens that only permits 4.3micrometre wavelength light through
- This passes through a test chamber and a reference chamber to a detector
- The detector passes the electrical signal to a microprocessor and then to the display as a continuous graph known as a capnograph
Which gases are exhaled during each phase of the capnography waveform?
- Phase 2 - dead space and alveolar gas
- Phase 3 - alveolar gas
Useful Tweets and Resources
Some STILL need reminding
— Cliff Reid (@cliffreid) September 30, 2022
Capnography: No Trace = Wrong Place
Spread the message from @doctimcook to
All anesthetists
All intensivists
All emergency physicians
All pediatricians who intubate
All cardiac arrest teams
All prehospital teamshttps://t.co/KKdrzt1jjV pic.twitter.com/BYXTvSGXJL
As part of the @RCoANews campaign, we ask you to watch our short video on capnography.
— Royal College of Anaesthetists (@RCoANews) November 26, 2021
Always remember 'No Trace = Wrong Place' & actively seek to exclude oesophageal intubation when a flat capnograph trace is encountered.
📽️https://t.co/drFFG8CVSQ pic.twitter.com/R9E7EQ64dk
Looking for free revision questions?
Check out the fabulous FRCA-revision.com where you can find a whole host of useful questions and explanations.

References and Further Reading


Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Try the toolkit for free


