Venous Thromboembolism

Take home messages
- VTE causes around 60 000 deaths per year
- Up to 25% of inpatients develop a DVT
- Formal VTE assessment is mandated by NICE
Meet the Father of modern pathology
Behold - Rudolf Virchow - physician, anthropologist, pathologist, prehistorian, biologist, writer, editor, and politician, who you'll probably recognise from his eponymous node and triad fame.
Hey, it was the 1800s, when the entirety of medicine was a glorified pamphlet.

I can't decide what's cooler - the glasses, the beard, or the fact that his colleagues referred to him as the Pope of Medicine.
He was first to figure out the pathophysiology of pulmonary thromboembolism, nonchalantly coining both embolism and thrombosis in the process.
Contrary to popular belief, Ol' Rudy didn't actually devise the triad himself, it was named in his honour much later in the 1950s (we think) long after he had died.
The triad
These are the three things you need to be able to regurgitate in the exam, to show you understand the fundamentals of why blood clots when it shouldn't.
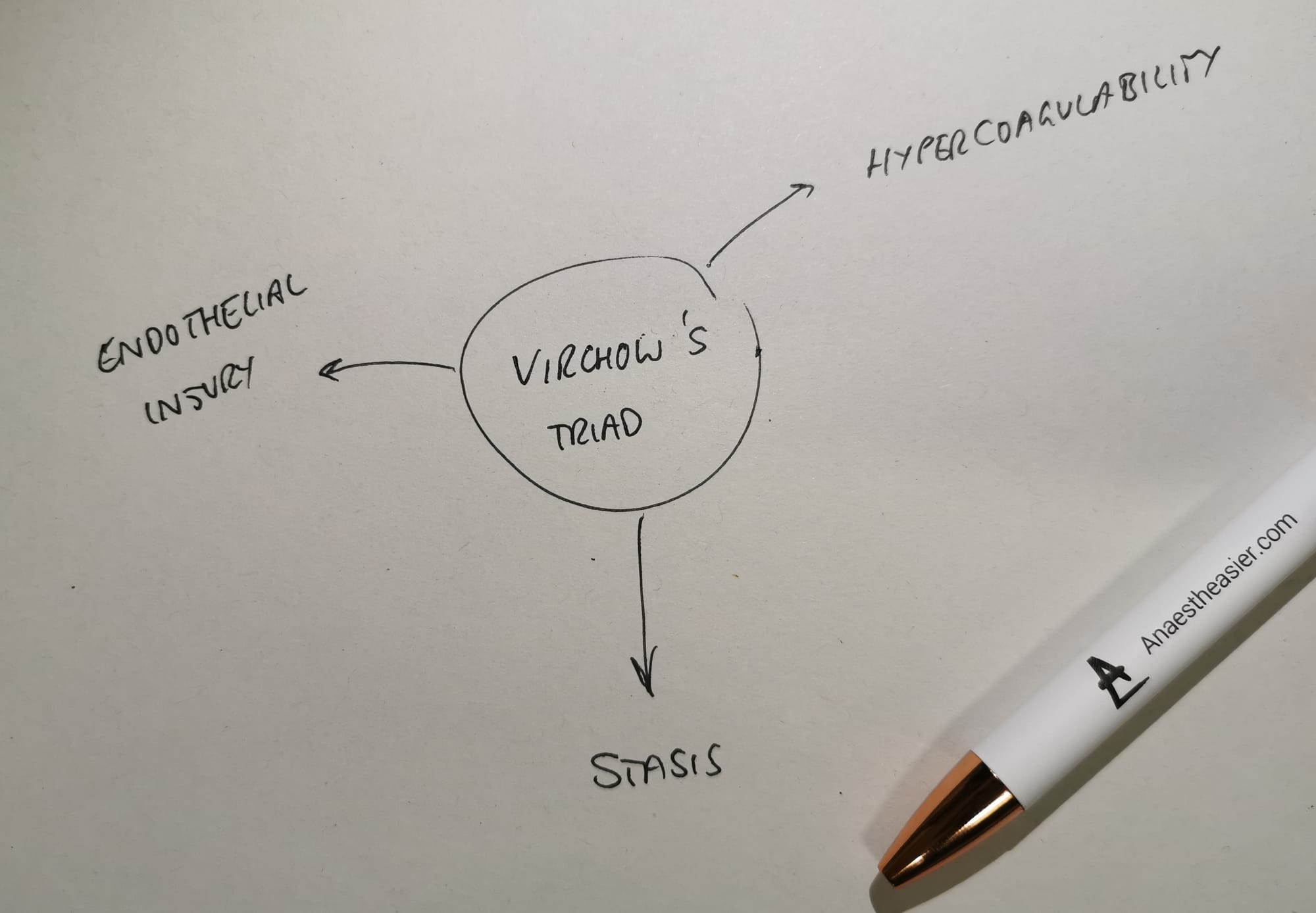
Blood, being in a constant state of clotting and unclotting, doesn't need much of a deleterious change in its environment to tip it too far in the wrong direction.
- If blood isn't flowing smoothly, it clots
- If blood is exposed to the collagen beneath the endothelium, it clots
- If there is another pathophysiological process going on that makes blood intrinsically more clotty, then guess what - it clots
We only really started paying proper attention to post op DVT risk in the 1930s, whereupon we started getting patients moving as soon as possible after surgery.
Then in the 1950s, along came heparin, followed by low molecular weight heparin in the 80s, which transformed VTE prophylaxis as one might imagine.
Then in the 1990s we started to see proper risk stratification with the Caprini and Padua prediction scores.
Then the GOATs of VTE, the DOACs joined the show properly in the 2010s.
Who gets it?
Anyone can get a DVT at any time, such is the nature of life and the inherent risk of pumping viscous living fluid thorough a squidgy human body.
That being said, there are specific risk factors that make thrombus formation much more likely.
Risk factors for venous thromboembolism
If you want to look really swish, break this down into the triad.
Stasis
- Trauma
- Long distance travel
- Surgery
- Paralysis and immobility
- Varicose veins
- Heart failure
- Age
Hypercoagulability
- Thrombophilia - Factor V Leiden, Protein C/S deficiency
- Malignancy
- Oestrogens
- Tamoxifen
- Chemotherapy
- Smoking
Endothelial injury
- Surgery
- Indwelling lines
How to prevent it
An injection a day keeps Virchow away.
It's not especially complicated - pick a component of the triad and see if you can modify it.
- Stasis - get blood moving
- Endothelial injury - minimise unnecessary trauma/indwelling lines
- Hypercoagulability - treat the causative issue and artificially thin the blood
Easy.
What interventions can reduce venous stasis?
- TED stockings
- Intermittent calf compression devices
- Bed exercises
- Early mobilisation
The key is to get the soleus muscle pumping as soon and as often as possible.
How can you reduce hypercoagulability?
- Ensure patient is well hydrated
- Treat infection
- Ensure patients with sickle cell are very well oxygenated
- Pharmacological thromboprophylaxis
How can we prevent VTE in hospital inpatients?
- Risk assessment for all admissions, both elective and emergency
- Risk assessment for each procedure
- Tailored prophylaxis regime for each patient
- Combination of mechanical and pharmacological prophylaxis
- Treat and prevent the three components of Virchow's triad - hydration, mobilising, pain relief
- Regular review
Mechanical options
We underestimate just how important the soleus muscle pump is for generating venous return from the legs and feet.
Working together with the valves, this muscle pump squidges blood back up the legs against gravity.
For a 6ft man with a leg measurement of 32 inches, that's nearly 60mmHg when standing upright, just to get the blood up to the pelvis.
It's easy to see, therefore, how quickly stasis can develop when we put patients in bed and leave them there for a few days.
To combat this we have a couple of options to mimic the soleic pumpage effect:
- Stockings that provide constant pressure
- Intermittent compression devices that mimic muscle contraction more closely
- Foot impulse devices that stimulate the plantar venous plexus
Which one you use will depend on the patient, the procedure and the protocols of your local institution, just remember there are some patients for whom mechanical thromboprophylaxis is contraindicated:
- Severe peripheral vascular disease
- Local skin infection, graft or necrosis
- Stroke
- Severe peripheral neuropathy
Pharmacological options
There are a number of agents available for your use to prevent unwanted internal clottage.
How you choose which one to use will depend on:
- The patient and their renal function and HIT risk
- The surgery and its bleeding risk profile
- The hospital and how much money it has
What options are there?
- Unfractionated heparin
- Low molecular weight heparin
- Warfarin
- Direct factor 10a inhibitors
- Aspirin
- Fondaparinux
- Dextrans
- Lepirudin
- Danaparoid
Unfractionated heparin
- Natural anticoagulant from pig gut or cow lung
- Big polysaccharide up to 40 kDa
- Binds antithrombin to form a complex that inhibits factors 10a and thrombin
- Given BD or TDS
- Usually subcut
- Monitor aPTT and platelets
- Reversible
- Better in patients with renal failure
- Higher bleeding risk than LMWH
- Can cause heparin-induced thrombocytopaenia (HIT)
Low molecular weight heparin
- Smaller versions of heparin up to 8 kDa
- Mainly only affect factor 10a
- Lower risk of HIT and bleeding
- Given subcut OD or BD
- If you want to monitor something - antiXa assay and platelets
- Renal clearance so caution in renal failure
Warfarin
The ol' reliable.
- Oral drug
- Vitamin K epoxide reductase inhibitor (not a vit k inhibitor)
- Prevents recycling of Vitamin K1
- Prevents production of factors 2, 7, 9 and 10 as well as proteins C and S
- Unpredictable effect
- Interacts with other drugs
- Monitor with INR
- Bridge with heparin or similar for three days to avoid warfarin skin necrosis (transiently pro-coagulant as anticoagulant factors are inhibited first)
DOACs
- Oral
- OD or BD dosing
- No effect on platelets
- No routine monitoring but can measure prothrombin time
- Predictable effect on coagulation
- Licensed for VTE prevention in elective hip and knee replacement
- Appears to be better than LMWH at preventing clots, with lower bleeding risk
Aspirin
- Oral daily dose of 75 - 300mg
- Salicylate
- Irreversible inhibition of cycloxygenase 1, preventing thromboxane A2 production and platelet aggregation
- Reduces risk of DVT and PE compared to doing nothing, but nowhere near as effective as heparin or equivalent
- Carries similar bleeding risk
- No idea what the best dose is and it doesn't do a good enough job to prevent clots by itself
- Not recommended
Fondaparinux
- Synthetic pentasaccharide
- Very similar structure to heparin's antithrombin binding site
- Directly inhibits factor 10a
- Single subcut dose per day
- Much lower risk of HIT
- Seems to be better than LMWH in preventing clots but higher bleeding risk
- Monitoring not routinely required but can do antiXa assay
Dextrans
- Polysaccharide
- Sticks to red blood cells and platelets
- Makes them less sticky
- Also boosts activity of antithrombin
- Also work as plasma volume expanders
- Have to be given IV at large volumes (1500ml) to have any anticoagulant effect
- Generally only used intraoperatively
- Risk of reactions and fluid overload
Not recommended.
Lepirudin
- Recombinant hirudin
- Derived from yeast
- Direct thrombin inhibitor
- Used in patients with HIT
- Given as continuous infusion
- Measure activity with aPTT
- Aim for ratio of 2 - 3
Danaparoid
- A weird heparinoid mix
- Inhibitors factor 10a
- But different chemical structure to LMWH
- Higher risk of bleeding
- BD subcut injection
- Monitor with antiXa assay but not routinely needed
- Risk of HIT so monitor platelets
Regional anaesthesia
This is a double-edged sword. You can reduce the risk of venous thromboembolism with regional anaesthesia (and avoiding a GA), however if you're doing a spinal you need to be cautious about timings with regards to pharmacological prophylaxis
- Regional anaesthesia causes a temporary sympathectomy
- This causes vasodilatation and reduced peripheral vascular resistance
- This improves peripheral blood flow and reduces venous stasis
Education
We're always advised to try and ensure our patients are as informed as possible about their healthcare and treatments.
- Patients should be given written and verbal information before and after surgery
- In particular they should be alerted to the signs and symptoms to watch out for
- They also need to be educated on how to administer thromboprophylaxis at home
Tell me about caval filters
"Hello dearest patient, you seem to be having trouble keeping your blood flowing smoothly."
"I'd recommend we pop a titanium spider in your biggest vein, to catch all the flying clots and nom them all up."
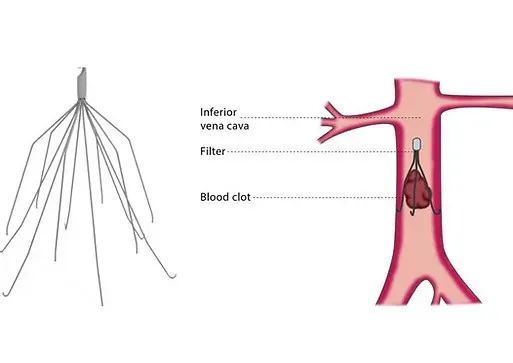
The theory here is very simple. If you have a load of clot flying from the peripheral circulation towards the heart, it's better to catch them with a net in the IVC than let them block the pulmonary artery or saunter through a PFO and cause a massive stroke.
However
I attended a 'bleeding and clotting' conference a couple of years ago, at which one of the keynote speakers - a wisened haematologist - astutely remarked:
- "If you put a lump of metal in the IVC, it's going to generate a load of clot"
- "If we'd found a metal that didn't, we'd be making heart valves out of it and doing away with blood thinners"
- "IVC filters are essentially pointless"
This made a lot of sense at the time, and they are associated with a greater increase of recurrent DVTs, however there are still specific occasions when IVC filters are used for the management of thromboembolism.
Indications
- Known large proximal DVT and
- Embolism within last month and
- Can't have anticoagulation
Makes sense I guess.
Useful Tweets and Resources
The @MayoClinic Perioperative Venous Thromboembolism Prophylaxis Recommendations: Stratified by Surgical Specialty and Estimated VTE Risk#SoMe4Surgery #MISIRGlobalSurgery @SWexner @NeilFlochMD @DrThawaba @jmills1955 @AntoninoSpin pic.twitter.com/uwPwZ7Mw17
— MISIRG (@MISIRG1) October 6, 2021
Download the ESA App on Perioperative VTE Prophylaxis! This FREE & user-friendly App is dedicated to physicians working in perioperative environments and in surgical intensive care units. Search iTunes and Google Play using the term "ESA: VTE Prophylaxis" and get started today! pic.twitter.com/eSCJq3IR7L
— ESAIC (@ESAIC_org) July 3, 2019
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
Anaestheasier® is a registered trademark.