TURP syndrome

Take home messages
- Transurethral resection of the prostate (TURP) usually involves irrigation with fluid to improve visualisation for the surgeon, and excessive systemic absorption of this fluid can lead to TURP syndrome
- TURP syndrome is thought to occur in between 1 and 8% of TURPs
- Symptoms are neurological and cardiovascular in nature, with agitation, seizures, coma and fluid overload being the main issues
- Hypo-osmolality is more important than hyponatraemia as a cause of central nervous system symptoms
- The most important treatment is recognising the problem and stopping the fluid irrigation as soon as possible
Anatomy
The prostate is an approximately 20g lump of glandular and non-glandular tissue encircling the male urethra as it leaves the bladder.
It has a mixture of secretory acini and smooth muscle and it produces seminal fluid.
It is split into four McNeal zones:
Fibromuscular zone
- 5%
- Integrates with urogenital diaphragm
- Very rarely affected by cancer
Transitional zone
- 5%
- Encircling urethra
- BPH usually affects this zone, and so classically presents with urinary symptoms
Peripheral zone
- 70%
- Cancer tends to affect this zone
- This means cancer rarely presents with symptoms
Central zone
- 20%
- Containing seminal ducts
TURP
- TURP remains the surgical gold standard for the treatment of benign prostatic hyperplasia (BPH)
- It works well if the prostate is less than 60g in size
- If the prostate is larger than 80g, then HoLEP (Holmium laser enucleation of prostate) is better
What does a TURP involve?
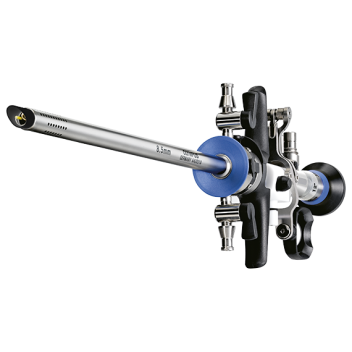
- A diathermy loop is passed through a resectoscope in the urethra
- The idea is that tissue is shaved off without damaging the prostatic capsule
- Usually takes about 60-90 mins
- There is continuous irrigation with fluid to clear debris and blood, and optimise visualisation
- A 3 way catheter is then left in to irrigate for 24 hours
What intraoperative problems can occur during a TURP?
- TURP syndrome can occur between 15minutes and 24hours from procedure start
- Bleeding is often hard to calculate as it is washed away
- Myocardial infarction
- Hypothermia
- Prostate capsule perforation
- Bladder or urethra perforation
- Penile erection
Anaesthetic Technique
- If you are asked in an exam what the gold standard anaesthetic technique for TURP is - say spinal
- If you are asked by your consultant for the TURP list that you're doing tomorrow, what technique you're going to use, probably go with 'GA and IGel'
- (clearly, don't just spout this answer for every patient, but the reality is that many sites do TURP under GA)
- There's little evidence between superiority of spinal vs GA
- Note that the surgeon often uses lithotomy position with head down tilt, so GA may require intubation
What are the benefits of regional anaesthesia in TURP?
- Patient can stay awake, so neurological symptoms of TURP syndrome can be spotted sooner
- Early recognition of bladder perforation or capsule tear, as the patient will complain of new shoulder pain or periumbilical pain
- Reduced risk of respiratory complications by avoiding GA
- Good post operative analgesia
How is pain carried from the prostate to the brain?
- Pain mainly carried from prostate, prostatic urethra and bladder mucosa via S2-S4 sacral nerves
- Bladder distension pain travels via T11-L2
- The sensation of needing to urinate travels via parasympathetic fibres from S2-S4
- So a block height of at least T10 is required to be sufficient to cover for bladder distension pain
What post operative issues can occur with TURP?
- TURP syndrome (from 15 mins to 24 hours post incision)
- Bladder spasm
- Ureter spasm
- Clot retention
- Haemorrhage
- Deep vein thrombosis
- Myocardial infarction
- Post operative cognitive dysfunction
What is TURP syndrome?
During TURP, the irrigation fluid is absorbed by the bladder and urethra, at a rate of approximately 20ml per minute.
Clearly, therefore, this can lead to quite significant volume overload in susceptible patients with cardiac disease, especially with prolonged surgery.
Furthermore, if the fluid used is glycine 1.5%, which is hypotonic, then it will steadily drop the sodium concentration as well as the osmolarity of the blood. It is mostly the drop in osmolarity that then leads to the neurological symptoms seen in TURP syndrome.
To compound this effect, the added intravascular volume leads to a natriuresis, which further contributes to the hyponatraemia
How common is it?
Probably more than we realise
Given every patient will absorb at least a moderate (around a litre) amount of fluid, and many of theses procedures are done under general anaesthesia, it is likely that many of the patients with mild symptomatic TURP syndrome go unrecognised.
That being said, the estimated incidence of mild to moderate TURP syndrome is up to 8%, which carries a mortality of less than 1%.
Severe TURP syndrome meanwhile carries a 25% mortality.
What are the features of TURP syndrome?
Neurological
- Restlessness
- Headache
- Burning sensation in hands and face
- Visual disturbances
- Convulsions
- Nausea and vomiting
- Coma
Cardio/Respiratory
- Reflex bradycardia
- Tachypnoea
- Hypoxia
- Pulmonary oedema
- Congestive heart failure
If severe it can also lead to coagulopathy, which can be detected early if you have the luxury of TEG or ROTEM.
How can we reduce the risk of TURP syndrome?
Symptoms and severity of TURP syndrome correlate directly with the volume of fluid absorbed, so the aim of the game is to reduce how much is absorbed into the systemic circulation.
How to reduce absorption of irrigation fluid
- Maintain normal blood pressure
- Short procedure time
- Minimise blood loss
- Reduce hydrostatic pressure of irrigation fluid
- Shouldn’t be more than 70cm above the patient and ideally not in a pressure bag
- Avoid capsular perforation or bladder perforation
Perforation of a viscus allows large volumes into peritoneal cavity or retroperitoneal space where it is then rapidly absorbed (of course you then also have the added problem of perforation to deal with...)
What should I do if my patient develops symptoms of TURP syndrome?
This is one of those cases where you would politely request that the surgeon stops the procedure if it is safe to do so, and more importantly stop the irrigation.
- Depending on your personal level of experience and confidence, you might call for help early, or crack on an manage it yourself - but probably best to at least let someone know...
Treat any bradycardia and hypotension as you would normally, and convulsions can be managed with benzodiazepines and magnesium as required.
Treat a sodium level of less than 120mmol per litre.
If the patient develops pulmonary oedema of signs of overload then judicious use of furosemide can help, and hypertonic saline is the back up option.
What are the features of an ideal irrigation fluid?
- Transparent
- Non-conductive of electricity
- Non-toxic and non-irritant
- Cheap and easy to manufacture
- Easy to sterilise
- Stable to store and transport
- Isotonic
- Non-haemolytic once absorbed
How well does glycine 1.5% compare to an ideal irrigation fluid?
- It is transparent, cheap, non-conductive, easy to sterilise and non-haemolytic
- It is potentially toxic, however, as glycine is an inhibitory neurotransmitter (non-essential amino acid)
- Can cause seizures and visual disturbance at high plasma concentrations
- It is also hypotonic at 220 mOsmol/kg
- NaCl conducts electricity but is otherwise pretty spot on (Not so much of an issue when using bipolar diathermy)
Most TURPs are now done using bipolar diathermy and saline or other crystalloids as irrigation fluid, so hopefully TURP syndrome is on the decline, however the FRCA exam loves a bit of glycine...
References and Further Reading


Useful tweets
Nice reference of TURP syndrome: https://t.co/IeAYRqunCi
— Joel M. Topf, MD FACP (@kidney_boy) February 7, 2019
#UroSoMe #tweeturology
— Antoine Kass-Iliyya (@antoinekass) April 30, 2019
Advantages of green light over TURP
Day surgery
Bloodless operation, no reported blood transfusion
Avoids TUR syndrome
↓Retrograde ejaculation
↓ED
↓Catheterisation
↓Hospital stay
"Goliath study", TURPvsGreen L. 2y f/u, no difference in voiding metrics
If you're not yet a member of Anaestheasier - there's a free 14 day trial if you want to give it a risk-free try, plus you get all of our PDF and flashcard resources for free as well as a mega discount on our Primary FRCA toolkit...