The Urology Robot

Take home messages
- The robot means reduced blood loss, less pain and a shorter stay for the patient
- It also, however, makes things a tad more complex for you as the anaesthetist
- Positioning, Pneumoperitoneum, Paralysis and Preload are paramount
Enter the robot
As with everything in modern life, the robot is becoming ever more ubiquitous, particularly in urology, which is the most likely list you'll find yourself on when encountering your new cyborg colleague.
So why use a robot?
Because it's a surgeon with four arms, dead steady hands and wrists that go all the way around, that's why.
For an increasing number of surgeries it's being found that a well-trained surgeon can achieve better results for their patient when employing the help of their their silver sidekick, including:
- Reduced blood loss (usually)
- Smaller incisions
- Less post operative pain
- Faster recovery time
- Shorter hospital stay
- Lower infection risk
The robot has 'anti-tremor' mechanisms that compensate for human muscle movements, as well as super-flexible wrists that provide a surgeon with unprecedented access to a variety of important bodily structures in a confined space, while the binocular 3D vision system gives better depth perception than flat laparoscopy screens.
All round a jolly sensible idea if you ask us.
Who uses it?
- Urology - prostatectomy and cystectomy*
- Gynaecology - hysterectomy, myomectomy
- General surgery - hernia repair, bowel resection
- Thoracic surgery - lung resection
- Cardiac surgery - mitral valve repair
*They still need a urine dip before surgery
A Spot of History
In 1985 the first brain biopsy using a robot was performed, the idea being that millimetre precision and a hand steadiness that would make a Parisian street performer proud would result in more accurate biopsies.
Clearly it worked, because it sparked a veritable revolution in surgical robot development, as people began to realise it was more than likely that robots of the future could easily outperform human hands if given the right investment and attention.
If you're interested, the robots we have in widespread use at present remain within the level 1 autonomy category, according to the US Department of Defence 5 point scale. Level 1 means the robot is a direct extension of the surgical supervisor, with no autonomous control of itself.
The interesting and equally terrifying concept of a level 5 robot, with zero human involvement whatsoever, is still a little way off, but it's not exactly inconceivable that one day your entire operation and anaesthetic could be entirely automated.
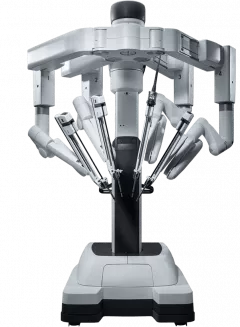
The Da Vinci robot has three bits
Well it has substantially more bits than that, but you only need to know about the following three for your career and exams:
- Master console where the surgeon sits (disconcertingly far away in the corner)
- Robotic surgical manipulator (docked to the patient)
- Visualisation tower
These DC-comic-universe-sounding components unsurprisingly take up rather a lot of room, so the ergonomics of your theatre become even more important than usual and you'll often find there are a limited number of theatres in which it can be used.
To cut a long story short, the surgeon controls the robot via the master console, which is usually in the corner of the room but could be in literally another country.
The robot is then docked to the patient once they're fully anaesthetised and positioned (just to check they're not going to slide down the table)
A surgical assistant is still needed to change the instruments and provide general encouragement.
So what's the big deal?
Surely having a robot with smaller, steadier and spinnier hands scrubbed instead of a human is only going to make life easier for the anaesthetist?
Well hold your horses just one second.
Robotic surgery is not without its own cohort of risks and complications, and it does need a fair bit of thinking about when deciding whether or not it's appropriate for the patient in front of you.
Disadvantages of robotic surgery include:
- Reduced access to your patient
- Large, expensive machine requiring extra staff straining
- Physiological strain of extreme positioning and pneumoperitoneum
- Increased risk of AKI and venous gas embolism
- Insidious bleeding can go unnoticed
- Increased intracranial pressure (again, position and pneumoperitoneum)
If the patient flinches, normally the surgeon will instinctively back up or at least pause for a second, but the robot? Those extra-steady hands might be an issue.
Coughing or flinching can cause damage to surrounding structures and potential catastrophy.
While not directly as a result of the robot itself, the physiological impact of the strange positions required can have a significant impact. The most common being lithotomy with steep Trendelenburg positioning (up to 45 degrees for RALP procedures).
The two most substantial physiological insults to the body during robotic urologic surgery are pneumoperitoneum and the steep Trendelenburg (head down) positioning, and to add insult to injury they each make the effects of the other worse as well.
What are the contraindications to robotic surgery?
There aren't really any absolute contraindications, however the following are strong relative contraindications:
- Obesity class 3
- Severe ischaemic heart disease
- Severe valvular disease
- Severe respiratory disease
- Known raised intracranial pressure
What issues might you face as the anaesthetist?
As always, when answering nebulous and vague questions such as this, one must categorise or die.
Anaesthetic issues
- Reduced access to the patient
- Need for complete immobility (muscle relaxation)
- Effects of pneumoperitoneum
- Analgesia
- Steep Trendelenburg position*
- Fluid restriction
*Intracranial pressure, periorbital oedema, increased risk of regurgitation
Surgical issues
- Logistics of docking the robot
- Damage to surrounding tissues
- Bleeding sometimes harder to spot
- Difficult communication with surgeon using console*
*This is somewhat mitigated by the machine's microphones and speakers, but if we're already concerned that surgeons become tasked focus when performing normal surgery, imagine what it's like when they can only see the screen, with zero peripheral perception of the patient.
SIM scenarios where the theatre team practices the process of docking, undocking and dealing with unexpected scenarios is a thoroughly good idea if feasible.
Patient issues
- Often have substantial comorbidities
- May not tolerate extremes of position or pneumoperitoneum
- High BMI may present challenges for table position and mechanism
The kidney problem
The kidneys thoroughly enjoy fluid as a general rule, as does the heart, however the airway, face and lungs very much disagree on this point, so when you tip your patient as close to upside down as makes no difference, the argument tends to heat up a bit.
So we compromise, and say that the kidneys have to go without for a little while, but they get rewarded with lots of fluid afterwards, if they're good.
- Intraoperative fluids should be used judiciously, and in general restricted, to prevent or at least minimise the extent of facial oedema and airway swelling
- You also want to reduce urine production while the surgeon is fixing ureters or the urethra where possible
- Strict input-output monitoring and thorough post-operative rehydration is critical
The blood problem
What are the cardiovascular effects of patient positioning during robotic urologic surgery?
The steep head down positioning causes the following effects:
- Increased central venous pressure
- Increased pulmonary artery pressure
- Increased pulmonary capillary wedge pressure
- Increased venous return
- Increased cardiac output
Meanwhile pneumoperitoneum causes the following:
- Increased systemic vascular resistance
- Increased venous resistance in IVC
- Reduced venous return
The overall impact is one of reduced cardiac output.
- These procedures have potential for substantial blood loss, and you're not going to have easy access to the patient once the robot is all docked and ready to go, so decent IV access is a must, and for prolonged procedures you need to think about keeping your patient warm, so plug in a fluid warmer
- An arterial line to monitor invasive blood pressure comes very highly recommended, and remember to adjust your transducer height once the table is tilted to whichever extreme position they need that day
- Have atropine on standby for when the pneumoperitoneum begins, as patients can develop profound bradycardia with or without arrest
How to manage the airway
Tube 'em.
The positioning, the need for muscle relaxation, the need to keep the patient's breathing tightly controlled, the raised airway pressures, the pneumoperitoneum...
Need any other reasons?
Just be sure to monitor your airway pressures and tidal volumes to check your tube hasn't slid its merry way down (or up) into a bronchus once the table is essentially vertical.
There aren't any specific ventilatory requirements, so the standard use of PEEP, lung protective tidal volumes (6-8ml/kg) and ensuring the CO2 isn't rising is fine.
Post op
- As always, a multimodal analgesia approach is advised for post operative pain control - a caudal sited just after general anaesthesia can work well
Useful Tweets and Resources
Robotic surgery is now so advanced that is possible to remove the shell from an uncooked egg and suture a defect. This can be done remotely via a keyhole approach using WiFi.pic.twitter.com/qovSQfI8z9
— Keith Siau (@drkeithsiau) September 11, 2023
What is the best #ventilationstrategy for robotic urologic and gynaecological surgery? New review by Chiumello et al #roboticsurgery #narrativereview #perioperative #anaesthesiahttps://t.co/Eb0YczQWMH pic.twitter.com/OP4LiGygqz
— British Journal of Anaesthesia (@BJAJournals) August 24, 2023
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.