Stellate Ganglion block

This is an exam-focused post aimed particularly at the Final FRCA SOE.
For a structure and procedure that one is unlikely to think about outside of a chronic pain clinic, the stellate ganglion is weirdly omnipresent in exam-land, probably because it allows rapid assessment of your anatomical, autonomical, procedural and physiological knowledge all in one go.
So here's everything you need for the exam.
Tell me a bit about the Stellate Ganglion
There are around twenty four sympathetic ganglia that form the sympathetic chain running down the lateral aspect of the vertebral column.
Stellate, meaning star, refers to the craggy spiky ganglion immediately anterior to the transverse process of C7.
It is an amalgamation of the inferior cervical sympathetic ganglion, and the first thoracic (and sometimes the second too) ganglion.
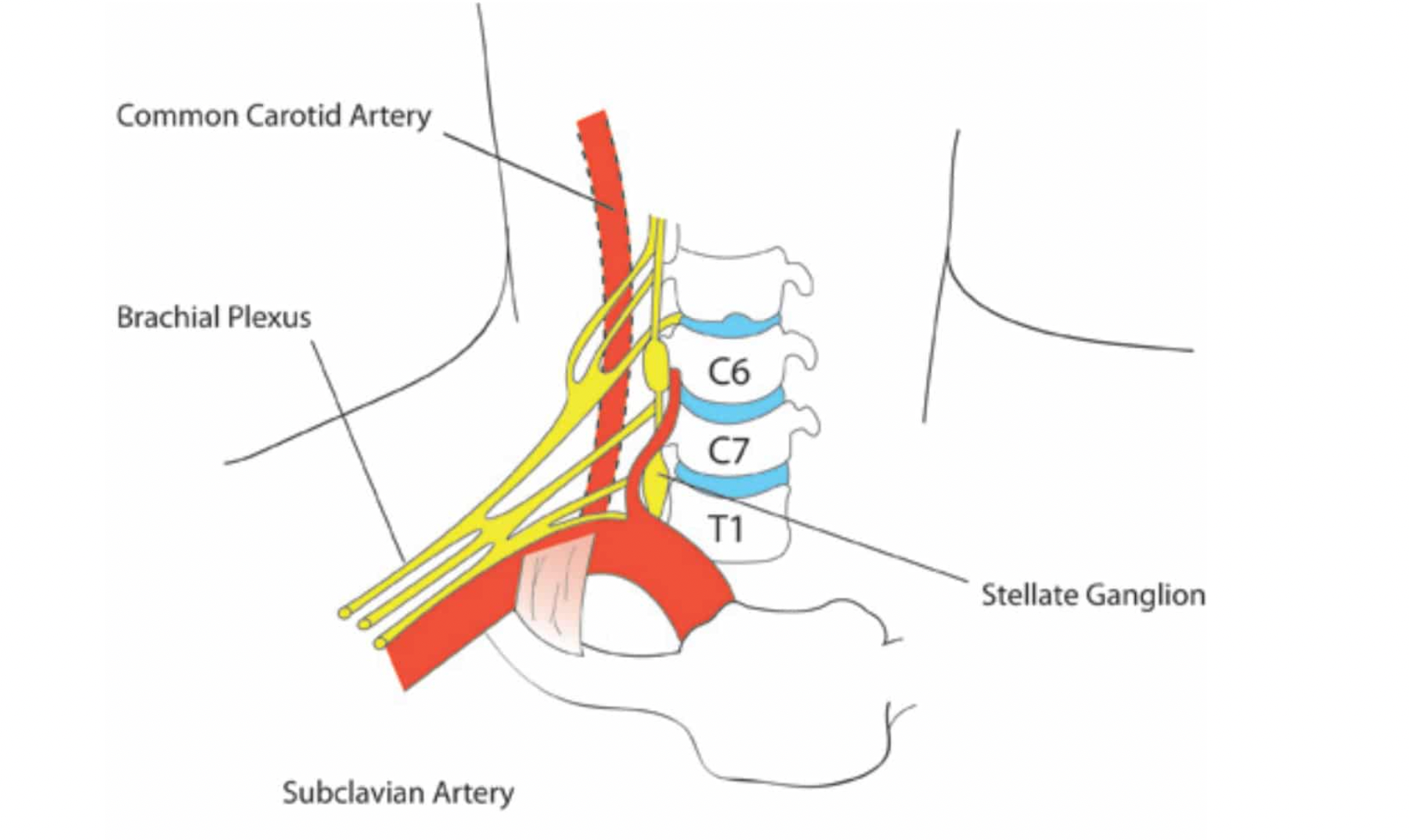
It receives pre-ganglionic sympathetic fibres from T1-T6 and provides sympathetic supply to the head, neck and upper limb.
What are the anatomical relations of the stellate ganglion?
Anterior
- Sternocleidomastoid muscle
- Subclavian artery (at its inferior pole)
- Carotid sheath
Posterior
- Anterior scalene muscle
- Brachial plexus fascial sheath
- Neck of first rib
- Transverse process of C7
- Vertebral artery
- Longus colli muscle
Lateral
- Superior intercostal artery and vein
- Ventral ramus of first thoracic nerve
Medial
- Prevertebral fascia
- Vertebral body of C7
- Oesophagus
- Lymphatics
Inferior
- Pleura
Why do I need to know about it?
Many pain signals travel with sympathetic fibres, in particular:
- neuropathic
- vascular
- visceral
Hence we often target sympathetic structures (stellate ganglion, coeliac and aortoiliac plexus) in procedures for chronic neuropathic pain.
It supplies a wide area including the face, neck and upper limb, making it very helpful when you need to reduce sympathetic activity in those areas.
It's a relatively simple and effective block when performed well, and it's commonly encountered in the chronic pain clinic.
What are the indications for a stellate ganglion block?
- Neuropathic pain - CRPS, post herpetic neuralgia, shoulder-hand syndrome, phantom limb pain
- Ischaemia - upper limb ischaemia, Raynaud's disease, scleroderma, frostbite, thromboangitis obliterans
- Inadvertent intra-arterial injection into the radial artery
- Refractory angina
- Hyperhidrosis
- Hot flushes
- Migraine
- PTSD
What are the contraindications?
- Patient refusal
- Allergy to any of the relevant medications used
- Significant anatomical deformity of the neck
- Recent myocardial infarction
- Significant coagulopathy
- Glaucoma
- Severe lung disease or issues with contralateral phrenic nerve that may make ipsilateral nerve palsy disastrous
Can I just needle it at C7?
Well you can, if you want to jump straight into tiger country and play with the vertebral artery and vein, dome of the pleura and inferior thyroid artery.
This is the paratracheal approach, and frankly - it's madness.
- Palpate the carotid pulse 2cm lateral to the suprasternal notch and 2cm above the clavicle
- This is your needle insertion point
- Use one hand to gently press the carotid sheath laterally
- Advance the needle perpendicularly (straight back) until you hit the transverse process of C7
- Pull back about 0.5 cm, aspirate and inject 15-20 ml of low concentration local anaesthetic (e.g. 0.125% levobupivacaine)
- Hope for the best
Yes, you will probably skewer the thyroid, might puncture the pleura and a few vessels on the way, might miss entirely and might inject into the vertebral artery.
So maybe don't do this approach?
Why is C6 better?
C6, or more specifically Chassaignac's tubercle - the transverse process of C6 - is the preferred landmark for performing a stellate ganglion block.
At this slightly higher level, the vertebral artery and vein are now tucked snugly inside the vertebral foramen of C6, keeping them relatively out of harm's way.
You're also a whole vertebral level further away from the lungs, and there's less thyroid to prang, which is nice.
The aim is to inject into the correct fascial plane and allow the local anaesthetic to descend gracefully onto the stellate ganglion below.
- Palpate Chassaignac's tubercle at the level of the cricoid cartilage
- Gently move the carotid sheath laterally and the trachea medially
- Insert needle between them and aim perpendicularly (straight back) to hit the bone
- Withdraw by 0.5 cm and aspirate and inject
How do I know if it worked?
It's more tricky to figure out if a sympathetic block has worked, compared to a sensory nerve block like the interscalene, because you don't get the same definitive sensory changes.
The generally accepted signal of success is development of ipsilateral Horner's syndrome (ptosis, miosis, enophthalmos, anhidrosis) demonstrating that sympathetic supply to the face has been interrupted.
Landmark vs Ultrasound
While there are a host of blocks where one could theoretically argue that ultrasound isn't drastically safer or more effective than a landmark technique, the stellate ganglion block certainly isn't one of them.
Ultrasound guided stellate ganglion blocks:
- Are vastly safer
- Are more effective
- Need far less local anaesthetic (3-5 ml vs 15-20 ml)
Watch the video shared below for an excellent demonstration of the ultrasound guided technique.
It's essentially the same set up as an interscalene brachial plexus block, but you pass through the anterior scalene to the fascia just next to the longus colli muscle, where the sympathetic chain lies.
This approach requires far less local anaesthetic (around 3 - 5 ml) and allows you to identify and avoid the crucial red bits of the neck, making it inherently safer.
What are the complications of a stellate ganglion block?
- Failure of the procedure
- Pneumothorax
- Brachial plexus block
- Recurrent laryngeal nerve block (hoarseness)
- Phrenic nerve block (breathlessness in fragile patients)
- Vagus nerve block (hypertension and tachycardia)
- Bleeding and haematoma (from vertebral artery specifically)
- Intravascular injection*
- Local anaesthetic systemic toxicity*
- Intrathecal injection
- Deep cervical plexus block
*It only takes 2-3 ml of local anaesthetic in the vertebral artery to induce seizures.
Some more SOE questions
What are the four parts of the sympathetic chain?
The paravertebral sympathetic chain is divided into four parts.
- Cervical - superior, middle and inferior ganglia
- Thoracic - multiple thoracic ganglia
- Lumbar - prevertebral ganglia
- Pelvic - sacral ganglia
The inferior cervical ganglion and first thoracic ganglion fuse to form the stellate ganglion.
T1 - T5 supply the cardiac, pulmonary and aortic plexus, and hence you start to see a bradycardia when your spinal anaesthetic creeps above T4.
Why does sympathetic blockade help with vascular pain?
By inducing a forced vasodilatation, pain induced by microvascular ischaemia can be alleviated to at least some degree.
- Diabetic patients may have micro-circulatory dysfunction
- Arterial occlusive disease can improve, especially if due to excessive arterial vasospasm
- Venous ulcers may improve with improved local blood supply
What types of sympathetic block do you know?
Ah the delightful old categorise or die.
Sympathetic blocks can be divided by purpose:
- Diagnostic
- Therapeutic
- Prognostic
Or they can be divided by permanence:
- Short term
- Long term
Diagnostic blocks
Used to determine how much of the pain is sympathetically mediated. There's no point going to the hassle of a sympathetic block if it isn't going to help.
These blocks are done under image intensifier guidance to ensure a pure sympathetic block (with no somatic block) is achieved.
As you might imagine, patients often have crossover with somatic and sympathetic pain, so diagnostic blocks can prove elusive and tricky.
Therapeutic blocks
These can be temporary, using local anaesthetic agents, or neurolytic, using phenol or ethanol. They can also employ radiofrequency ablation. The more permanent blocks are usually reserved for cancer and peripheral vascular disease, and should be used with extreme caution in other situations, as you might expect.
Prognostic blocks
A bit like diagnostic blocks, these are used to test what effect a block is going to have - improved blood flow, sweating, pain etc - to see if a block is a good plan or not.
If you're going to plan a definitive procedure based on prognostic blocks, you need multiple prognostic blocks to confirm a consistent response.
Short and long term blocks
These can be used for short term analgesia, in which case local anaesthetic agents will be employed.
They can also be for long term relief, where phenol or alcohol may be used.
- Phenol will destroy sensory and motor nerve fibres by denaturing proteins
- With time these fibres can regenerate, so it's not necessarily a permanent block
- Alcohol will destroy more of the cell body, and will give a denser block of longer duration, but also causes more neuritis
Techniques such as radiofrequency ablation will provide a more permanent block.
How does IV regional sympathetic blockade work?
Kind of like a Bier's block.
The limb is exsanguinated (internally) and isolated with an arterial tourniquet, after which a drug (usually guanethidine) is infused into the venous system of the limb.
Guanethidine blocks noradrenline reuptake and depletes the post-ganglionic nerve stores, reducing sympathetic activity once the blood flow is re-established.
What non-anaesthetic drugs can be used to target the sympathetic nervous system?
- Guanethidine
- Ketorolac
- Phentolamine
- Phenoxybenzamine
- Nifedipine
- Clonidine
References and Further Reading

Related Posts






