Peripheral Nerve Stimulators
Take home messages
- Residual neuromuscular blockade is defined as a ToF ratio of <0.9
- It delays recovery, and can result in hypoxia, aspiration and increased post operative pulmonary complications
- It can also risk accidental awareness under general anaesthesia
Nerves are really cool
The fact that a squodgy 1.5 kilogram blob of fat and salty water is able to construct a faithful hallucination of its surroundings and then control the movement of other squodgy bits of fat, protein and bone in order to navigate through that reality in order to survive is frankly insane.
How it controls them is equally interesting.
Nerves run on electricity, albeit with ions rather than electrons, and this means two things:
- We can measure their activity (EEG, ECG, EMG)
- We can interfere with their activity (Nerve stimulators, cardioversion, ECT)
Today's topic of interest combines both of these points, as peripheral nerve stimulators simultaneously interfere with normal nerve function, while also allowing us to make an assessment of their function.
The shocking duo
You need to be aware of two types of nerve stimulators in your anaesthetic clinical practice, and the two different occasions upon which they are used:
- Those for assessing degree of neuromuscular blockade
- Those for assisting needle placement when performing a nerve block
Today's post focuses on the former - measuring neuromuscular blockade.
Why measure it?
If you slug a syringe of premium red label into your patient's vein, they're going to stop moving and stop breathing.
If I were to ask you 'how paralysed is your patient?' you can confidently respond with 'very'.
If I return in an hour and ask you again 'how paralysed is your patient?' you're probably not going to be so certain in your response.
Depending on the adequacy of your anaesthesia:
- They might be breathing
- They might start moving
- They might even be sat up extubated and talking, wondering what on earth I'm on about
The truth is it is very hard to tell exactly how much residual effect your muscle relaxant is having just by looking at the patient.
How can you assess muscle blockade clinically?
If the patient is awake and following commands, you can get them to do stuff with their muscles and see if it's any good.
- Sustained head lift (off the pillow for more than five seconds)
- Hand grip
- Tongue depressor test (grip it between the teeth and resist removal)
If the patient isn't awake, you can look at clinical signs, such as:
- Coughing on the tube
- Spontaneous respiration and tidal volumes >15 ml/kg
Clearly these will tell you that the patient is no longer fully relaxed, however they don't tell you much about any residual weakness that might be floating around and hence these are deemed 'inadequate' by the AoA.
Neostigmine or Sugammadex?
In reality the reason we're monitoring neuromuscular function in theatre is to answer this question - how are we going to reverse them?
Since sugammadex came off patent and is no longer financially ruining the hospital, the threshold for using it has dropped in a manner proportional to the price tag.
As a result, many junior anaesthetists are now foregoing the age-old (since 1958) tradition of using a nerve stimulator to formally assess the degree of residual block, and are choosing instead to 'bosh in some sugammadex'.
- 'Some' referring to 2mg/kg, or more pragmatically - 1 vial for everyone
Let's face it
In reality, this approach is unlikely to cause a problem most of the time, as long as you're giving between 2 and 4mg/kg and it's been at least forty minutes since you last injected anything from a red labelled syringe.
However.
It's a rather a sledgehammer approach that does carry with it a few drawbacks:
- It's still around £50 per vial
- Some people will react to sugammadex, who wouldn't have reacted to neostigmine and glycopyrrolate
- Some people will react to the rocuronium-sugammadex complex, even if they wouldn't have reacted to either of the two individual agents
- It interferes with hormonal contraceptives
This is without mentioning the lamentable loss of a core anaesthetic skill - twitching the patient - which very much remains highly examinable.
It was very much mandatory according to the Recommendations for Standards of Monitoring during Anaesthesia and Recovery 2015:
“A peripheral nerve stimulator must be used whenever neuromuscular blocking drugs are given. … A quantitative peripheral nerve stimulator is required to accurately assess the train-of-four ratio.”
This statement has softened somewhat in the new 2021 guidance:
"Quantitative neuromuscular monitoring should be used whenever neuromuscular blocking (NMB) drugs are administered, throughout all phases of anaesthesia from before initiation of neuromuscular blockade until recovery of the train-of-four ratio to > 0.9 has been confirmed"
So here it is.
Why bother monitoring neuromuscular function?
- To see if your patient is safe and ready to extubate
- To allow appropriate reversal of residual neuromuscular blockade
- To adjust muscle relaxant infusions on the intensive care unit
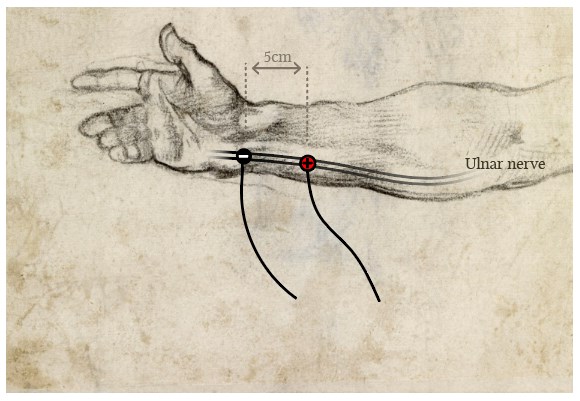
Where do I put the electrodes?
- The negative (black) electrode goes distally, close to the nerve
- The positive (red) electrode is more proximal and further away
- Avoid sticking them directly above muscle, as this will just twitch the muscle directly without involving the neuromuscular junction
Choose a reliably superficial nerve with a known muscle group to assess:
- Facial nerve near parotid - orbicularis oculi
- Ulnar nerve near wrist - adductor pollicis
- Tibial nerve behind medial malleolus - flexor hallucis longus
How many twitches?
In short, what we're going to do is rain electrons down onto a known nerve, supplying a known muscle, with a shedload of voltage through the skin sitting vaguely nearby.
The plan is to induce an action potential that will be transmitted along the nerve to the muscle, the activity of which will then give us an indication of how active the neuromuscular junction is.
Sounds simple enough.
What are the components of a peripheral nerve stimulator?
- Console with control panel
- Power source (battery)
- Wires
- Electrode clips
- ECG stickers
Which muscle groups are most sensitive to blockade?
- The small muscles of the eye and larynx are most sensitive
- The large muscles of the limb are far less sensitive
- The diaphragm is least sensitive, due to enormous redundancy in the number of nicotinic acetylcholine receptors for obvious evolutionary reasons
This means that testing the facial nerve and twitching orbicularis oculi is a more accurate representation of the laryngeal muscles, while testing the ulnar nerve and twitching adductor pollicis is better for assessing residual weakness in the respiratory muscles.
We want to generate a supramaximal stimulus, to ensure all the neighbouring neurons are recruited and activated together, to trigger as many neuromuscular junctions as possible give us the most accurate measurement of muscle function.
We could just fire a single bolt of voltage at our nerve and see if the muscle twitches or not. This would give a fairly simple 'yes' or 'no' answer to whether the neuromuscular junction is doing anything, but it doesn't really tell us how much neuromuscular blocking agent is still hanging around.
For this we need a more nuanced approach.
Train of Four
Four identical supramaximal stimuli are delivered at 0.5 second intervals (2 Hz) and the number of twitches observed corresponds to the percentage of receptor blockade.
- 0 twitches is >95%
- 1 twitch is 90%
- 2 twitches is 80%
- 3 twitches is 75%
- 4 twitches is <75%
So four powerful twitches does not mean the patient does not need reversal, it means that up to 75% of their receptors are still full of rocuronium.
ToF Ratio
Non-depolarising muscle relaxants demonstrate fade, where sequential neuromuscular impulses decrease in amplitude as a result of pre-synaptic receptors being blocked as well.
These pre-synaptic receptors normally increase the amount of acetylcholine released on subsequent impulses, so if they're blocked by the roc, the number of vesicles released will reduce, and so will the strength of contraction.
ToF ratio simply compares the size of the first and last twitch in the train of four.
- The fourth twitch must be 90% of the power of the first in order to be reasonably reassured that airway reflexes will be intact
Depolarising agents do not cause fade (unless you caused phase 2 block but we'll ignore that for now) and so will simply produce four twitches of equal magnitude, and the magnitude will depend on how much recovery of function has occurred.
Here's the graph you need to be able to draw in the exam
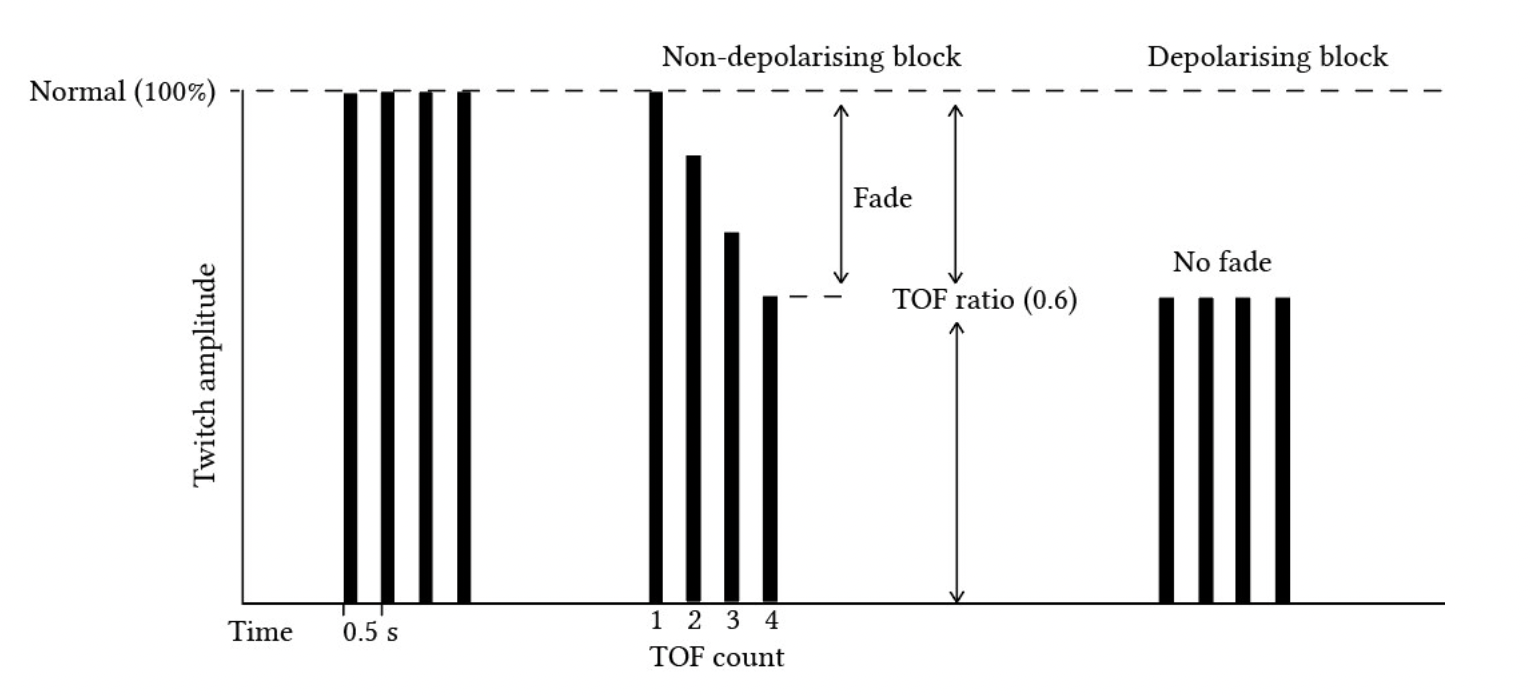
In reality, you're going to have a very hard time distinguishing a TOF ratio of 0.9 from one of 0.7 just by looking at the patient moving when you zap them, as it's very hard to estimate muscle function just by looking at them.
This is why other methods exist as well.
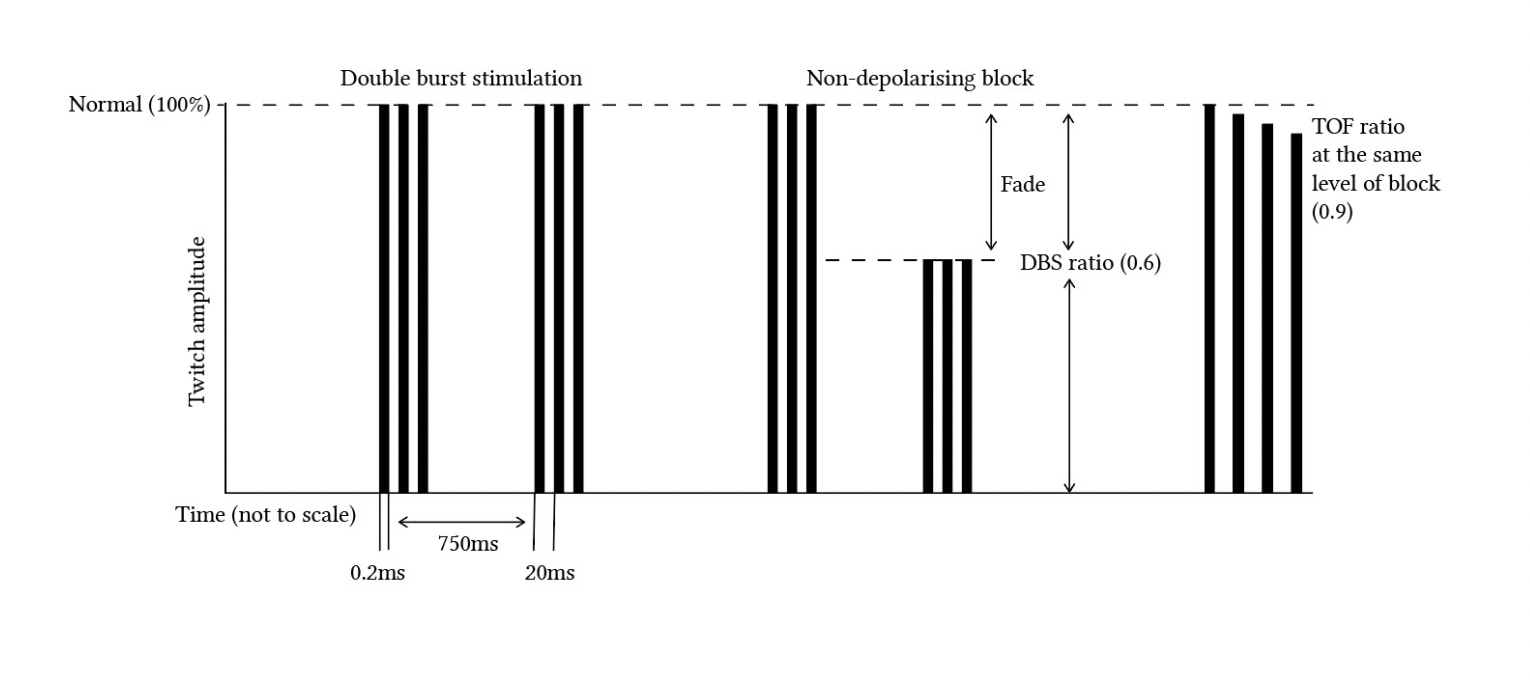
Double Burst
Two brief tetanic bursts at 50Hz are fired, separated by a 750 ms gap.
The idea here is that any fade will be much more evident between these two bursts than during a train of four test.
- Double burst is more sensitive at detecting residual block than train of four
It's far easier to see a difference between these two twitches than between the train of four.
Tetany
If you're not seeing any twitches at all with the other modes, and you're certain your electrodes are in the right place, the machine has enough battery and is delivering a sensible current, then you can try tetanic stimulation.
- A stimulus of 50 - 100 Hz for 5 seconds will often give enough oomph to pick up a muscle contraction that the other modes miss
Post-Tetanic Count
If you do decide to use the tetany button, you'll flood the neuromuscular junction with acetylcholine and may see a response.
If you then try another mode again (such as ToF or single twitch) immediately after, all that excess acetylcholine swilling around in the synaptic cleft may be sufficient to produce a visible twitch, that wasn't visible before the tetany.
- This is called post-tetanic facilitation
- 15 twitches of post-tetanic count is equivalent to a normal ToF count of 2
- If you see fewer than 5 twitches when stimulating after tetany, then the patient is profoundly blocked
It is a useful technique for ensuring a patient is still deeply paralysed during high-stakes surgery where any movement at all is bad news for all involved.
The numbers you need to know
- The threshold current to detect a muscle response is around 15 mA
- A supramaximal stimulus is usually around 50-60 mA
- The single twitch mode will deliver at 0.1 Hz
- A decrease in twitch height will appear at 90% receptor occupancy
- Train of Four fires at 2 Hz and repeats every 10 seconds
- Double burst fires two 50Hz impulses 750 ms apart
- Tetany fires at 50-100Hz for 5 seconds
How much sugammadex?
- You gave a full intubating dose two minutes ago - 16 mg/kg
- No twitches on ToF, PTC of 2 or less - 4 mg/kg
- PTC >2 or any twitches on ToF - 2mg/kg
Some sources say you can use 1 mg/kg if four twitches are visible, however this isn't universal guidance, and of course the manufacturers want you to use as much as possible so will always recommend 2 mg/kg.
Does a peripheral nerve stimulator guarantee recovery of muscle function?
Sort of but not really.
A qualitative nerve stimulator can technically only tell you that the ToF ratio has dropped to less than 0.4.
- This is not technically complete recovery
- The patient may have some residual weakness in certain circumstances
However if you have competently used a nerve stimulator to guide your use of reversal agents, and have subsequently tested again with demonstrable improvement in muscle function, then you can be fairly certain you've done a good job.
What's the best way to monitor neuromuscular blockade?
Technically we should all be using quantitative monitoring, including:
- Acceleromyography - measures thumb acceleration and derives force
- Electromyography - intramuscular electrical activity
- Mechanomyography - isometric adductor pollicis contraction
Essentially these all monitor the same thing in much more detail and more often, and generate a graph over time to demonstrate just how paralysed the patient is.
Your department may or may not have one of these in a cupboard somewhere.
What if I can't see any twitches?
- The patient might be fully paralysed*
- Check the settings to ensure the stimulus is large enough
- Check the battery
- Check the wires
- Confirm the electrodes are attached where you intended them to be
- Consider moving them to another site (face, tibia, wrist)
*If you have given magnesium or gentamicin, then rocuronium will last a lot longer
What are the complications of using a peripheral nerve stimulator?
- It hurts if the patient is awake
- You might interpret the information incorrectly
For example, poorly placed electrodes may lead you to think the patient is fully paralysed and lead to inappropriate administration of enormous and expensive quantities of sugammadex.
The patient may then go home and get pregnant because their hormonal contraceptive didn't work because the sugammadex interfered with the progesterone and you forgot to give them this leaflet (or your trust's version).
Here's our video
Please note that I get the electrodes the wrong way around in this video:
- Black should be on the nerve
- Red should be further away
I apologise and will sort this in due course.
Nerve stimulators for regional anaesthesia
We'll briefly discuss these here, with just the bits you need to be able to pull out in an exam to keep things simple.
Did I touch a nerve?
Yes, yes you did. With a blunt needle attached to a little electric box and a couple of electrodes.
You did it on purpose because it's safer than stabbing a nerve.
Most blocks are generally done under ultrasound guidance these days, however the use of a nerve stimulator is still very much employed by senior consultants, and thus remains examinable content.
- The most important characteristic is that the stimulator provides a constant current despite the changing resistances of the tissues that the needle passes through
Resistance in tissues can change between 1 kOhm to 20 kOhm so if the voltage were constant, the current would vary by a factor of 20.
Other important features:
- The output should be monophasic, meaning the current only flows in one direction
- The frequency of the stimulator should be adjustable
- It should clearly display the current being delivered (0.1 to 5 mA)
- There should be an indicator to demonstrate the integrity of the electrical circuit, to show it's working
- It should be battery operated
Where do I put the electrodes?
The negative electrode attaches to the needle, so that maximum current density is at the tip of the needle, and needs only a quarter of the current to stimulate the nerve than if the positive electrode were attached to the needle instead.
What is rheobase and chronaxie?
- The minimum current required to stimulate a nerve is called rheobase
- Chronaxie is the duration of current stimulus needed to stimulate the nerve at twice the rheobase
- Large A motor fibres have a shorter chronaxie of 0.05 - 1 ms
- A and C fibres have a chronaxie of 0.15 and 0.4 ms respectively
This means you can use a shorter pulse in an awake patient, to elicit muscle movement without eliciting pain.
What thresholds do I use?
Some anaesthetists start high (around 2 mA) and then reduce the current as they get closer to the nerve of interest.
Others stay below 1 mA from the start - ask the consultant you're working with.
You're interested in eliciting a muscle twitch with less than 0.5 mA, when the needle is less than 2 mm from the nerve.
This isn't 100% reliable as a rule, however, so we'd always recommend using ultrasound as well, to reassure yourself you haven't shoved the needle right into the nerve.
What happens when I inject?
Well you're going to aspirate first, of course, to check you're not in a blood vessel, the intrathecal space or a kidney, and then inject cautiously and slowly.
- The volume of local anaesthetic will physically displace the nerve and thus the twitch will disappear almost immediately
- The pressure required to inject will be constant and low
If it doesn't disappear, then the needle may be in the nerve and should be withdrawn a little.
What are the recommendations for monitoring during recovery of anaesthesia?
- Adequate supervision requires that an anaesthetist should be present throughout the conduct of anaesthesia or the administration of procedural sedation
- General anaesthesia requires minimum monitoring of ECG, SpO2, NIBP and capnography, which should be checked for correct function and begun before induction of anaesthesia and continue throughout anaesthesia, transfer to the post-anaesthesia care unit (PACU) and recovery
- Age-adjusted minimum alveolar concentration (MAC) should be monitored during use of inhaled anaesthetic drugs
- Capnography should be continued until any artificial airway is removed and a response to verbal contact re-established
- Regional anaesthesia requires minimum monitoring of ECG, NIBP and SpO2 which should begin before the procedure, and should be continued for at least 30 min after block completion
- Procedural sedation requires minimum monitoring of ECG, SpO2 and NIBP
- Capnography should be used during procedural sedation whenever there is loss of response to verbal contact
- Transfer requires minimum monitoring of ECG, SpO2 and NIBP
- If an airway device remains in place capnography should be used during the transfer of anaesthetised or sedated patients, including from the operating theatre to the PACU
- Quantitative neuromuscular monitoring should be used whenever neuromuscular blocking (NMB) drugs are administered, throughout all phases of anaesthesia from before initiation of neuromuscular blockade until recovery of the train-of-four ratio to > 0.9 has been confirmed
- Processed electroencephalogram (pEEG) monitoring should be used when total intravenous anaesthesia (TIVA) is administered together with a NMB drug
- It should start before induction and continue at least until full recovery from the effects of the neuromuscular blockade has been confirmed
- It should be considered during other anaesthetic techniques including inhalational anaesthesia and for the high-risk patient
- Capillary blood glucose and ketone monitoring should be immediately accessible in every location where patients are anaesthetised and blood glucose should be measured at least hourly in patients with treated diabetes
- Alarm limits for all equipment should be set to patient-specific values before use
- Audible alarms should be enabled during anaesthesia
- An anaesthetic record should be made with an accurate summary of information provided by all monitoring devices
- We recommend automated electronic anaesthetic record systems and that these be integrated into the hospital’s electronic health record system
- Additional equipment and monitoring that anaesthetists should have access to should include blood gas analysis and haemoglobin measurement and flexible bronchoscopy (for confirmation of tube placement in the airway).
Here's our post on muscle relaxants
Here's our post on awareness

References and Further Reading