Pacemakers

Take home messages
- Know what type of device you're dealing with, and why it's there
- Know what you need to do with it in theatre, and an emergency
- Know where your nearest cardiac physiologist is
What are they?
Put simply these little boxes of electrical cardiac wizardry have one function - to ensure the heart maintains a steady, regular rate and rhythm, without going too fast or too slow.
In their simplest form, they simply deliver a small electrical shock to wherever the lead has been implanted (hopefully some myocardial tissue) on a regular basis, in the hope that this triggers a meaningful contraction, to ensure the patient's heart rate doesn't drop too low.
As with all things in medicine, they have steadily become more complicated over the years, and now they have all sorts of fancy modes and models to achieve ever more nuanced heartbeats, and causing ever more stress for those unfamiliar with their intricacies and variations.
What are the different types?
Permanent pacemaker
- Little implantable box with two main parts - pulse generator and leads.
The pulse generator (box) has:
- A battery
- A transmitter and receiver
- A microprocessor
- A reed switch (how the magnet turns it off)
The leads can be:
- Single
- Multiple
- Unipolar or bipolar
The pacemaker delivers a tiny electric shock to whichever bit(s) of the heart the lead(s) are embedded into, either at a pre-programmed rate, or in response to a measured rhythm (more on this in a minute.)
Biventricular pacemakers
- Also called cardiac resynchronisation devices
- These are a particular type of pacemaker
- Used in symptomatic moderate/severe heart failure
- Where left ventricular ejection fraction is <35% with wide QRS
- By optimising timing between the right and left ventricle, it gives a more efficient stroke volume and therefore cardiac output
So what is an ICD?
- Implantable cardioverter defibrillator
- They detect and monitor cardiac electrical activity
- These can then pace or give shocks as required
- Most are used as secondary prevention after a cardiac arrest or ventricular arrhythmia, to prevent it happening again

If you look closely, you can see the moment professional footballer Anthony Van Loo's ICD kicks in and saves his life.
Ok and what's a loop recorder?
- Implantable device
- Diagnostic only
- No leads
- Used to try and diagnose whether an arrhythmia is the cause of someone's syncope or palpitations, or for monitoring atrial fibrillation
From these descriptions, we can infer that one would require a pacemaker, or similar device, when there is some issue with the heart's conduction system.
Which leads us nicely onto...
Why is it there?
'Because there's a conduction problem in the heart' is a true but insufficient answer - we need to know exactly what the problem is.
What are the indications for permanent pacemaker insertion?
- Symptomatic bradycardia secondary to AV node block (>50%)
- Sick sinus syndrome
AV node block can be first, second or third degree.
- First = PR interval >0.2 seconds, doesn't usually need a pacemaker
- Second = Dropped QRS segments, either after a gradually prolonging PR interval (Mobitz type I) or regularly every second or third beat or so (Mobitz type II) - May need a pacemaker depending on symptoms
- Third = No coordination between atria and ventricles, needs a pacemaker
A patient may have an implanted device for all sorts of reasons including heart failure or malignant arrhythmias, which are of particular pertinence to our anaesthetic, so have a dig through their notes if available, and talk to the patient if possible, about what it is you're actually dealing with.
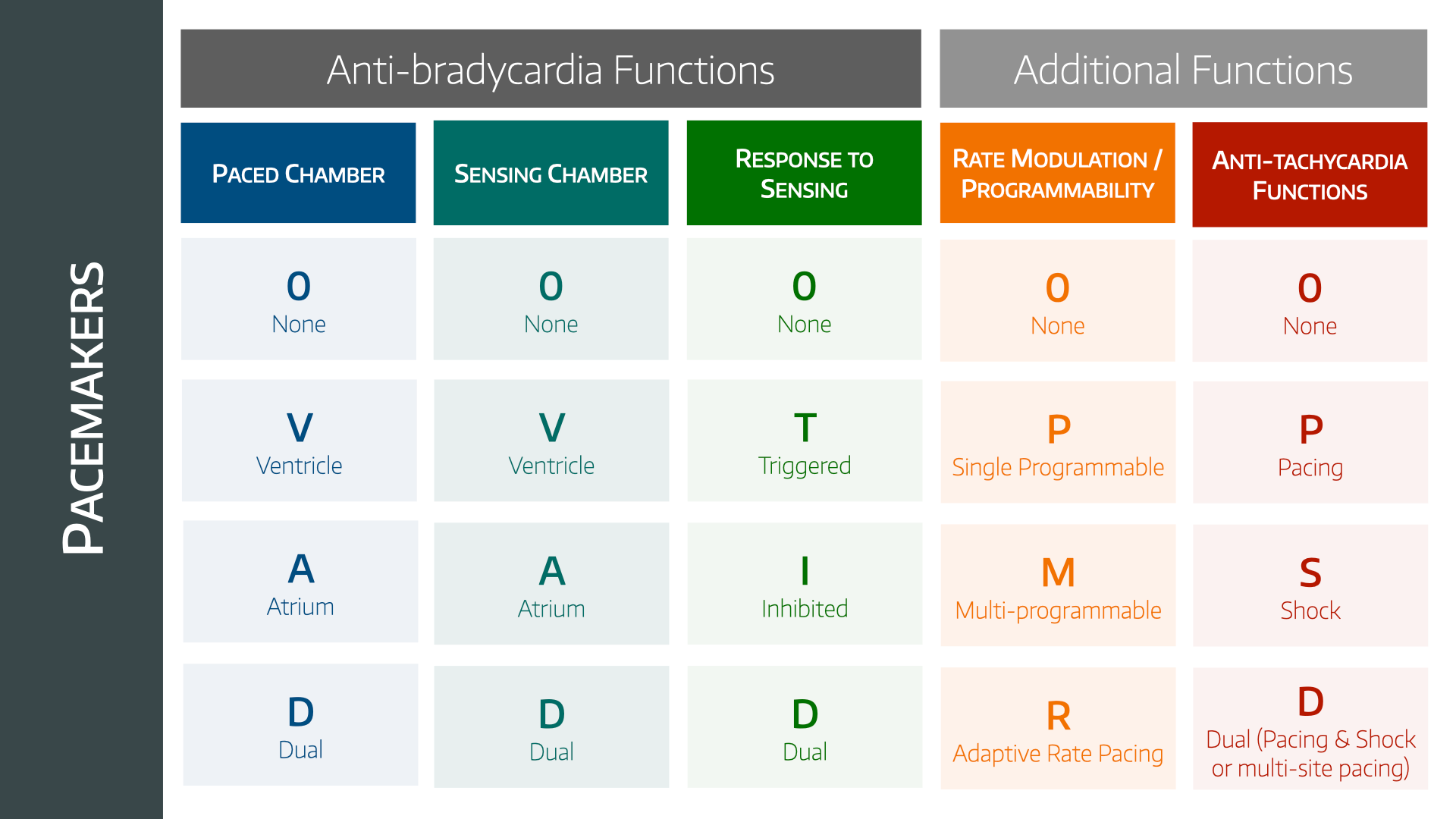
The codes
You need to understand (and be able to drone on about) the coding nomenclature for permanent pacemakers, when really we all know that the answer is 'talk to the electrophysiologist'.
What are the pacemaker codes?
Ah the elusive codes that you revise every six months and promptly forget within three days.
- Five letters
- The first three are about how it prevents bradycardia
- The last two are about how it prevents tachycardia
The letters in order describe:
- The chamber paced - A, V or D for dual
- The chamber sensed - A, V, D for dual or 0 for none
- The response to sensing - Triggered, Inhibited, Dual or 0
- The rate modulation or programmability - 0 for none, P = single programmable, M = multiprogrammable, R = rate modulation
- The anti-tachycardia function - 0, Pacing, Shocking, Dual or Multi-site pacing
Pretty much every pacemaker follows this PSR RA coding.
An example of rate modulation would be having an accelerometer inside the pacemaker that detected movement, which is assumed to be activity, and therefore causes the pacemaker to increase the pacing rate accordingly.
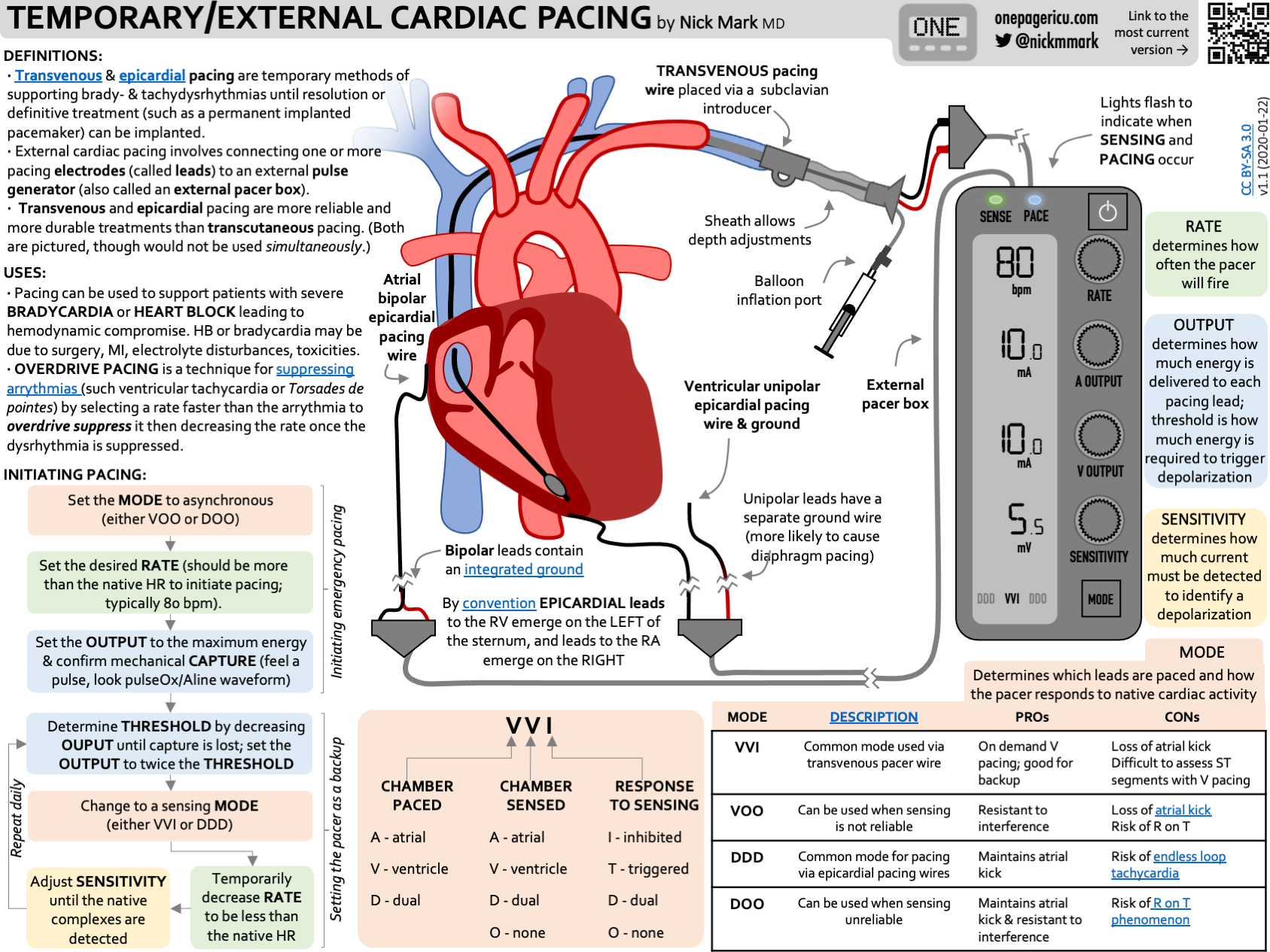
What are some common pacing modes?
VVI
- Ventricle is paced
- Ventricle is sensed
- If no impulse detected then pacemaker will trigger at a pre-determined rate
- If there is an impulse, then the pacemaker is inhibited
DDD
- Atrium and ventricle are paced
- Atrium and ventricle are sensed
- If both are functioning well, the pacemaker will sit back and just listen
- If either isn't functioning well, the pacemaker will kick in for that chamber
VOO
- The ventricle is paced at a set rate with no regard for intrinsic activity
- This is used in surgery as it won't be interfered with by diathermy etc
What is capture?
The box can generate an electric impulse, but whether that impulse actually achieves anything meaningful is another matter.
- Electrical capture means that the impulse has transmitted through the conducting system
- Mechanical capture means this has resulted in a meaningful myocardial contraction
Unsurprisingly, we only really care about mechanical capture.
As a general rule, upon insertion, pacemaker installers (a.k.a. cardiologists) will turn down the current generated by the pacemaker until there is loss of mechanical capture, and then set the current at 2 - 3 times this value, to ensure it doesn't lose capture out in the wild.
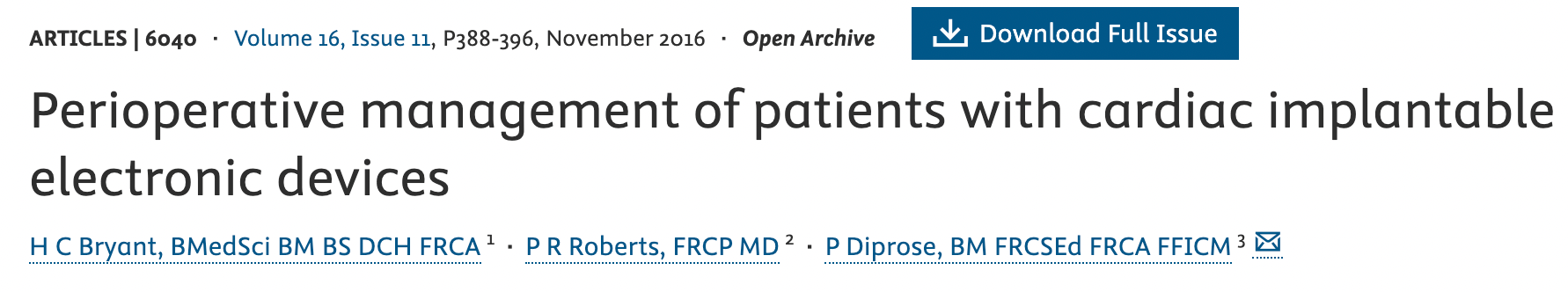
How to anaesthetise them
Now let's say you're anaesthetising a patient with a pacemaker for some completely unrelated, non-cardiac operation.
The fact that they have a pacemaker in the first place usually means they also have a whole load of other stuff going on.
What do I need to know about my patient's pacemaker?
- Why do they have it in the first place?
- Is it working?
- How long have they had it?
- When was it last interrogated?
- How much battery life does it have?
- What rate is it set to?
What other history is important?
- What has the cardiologist said in the last clinic letter?
- How is the patient's exercise tolerance?
- What symptoms are they having? - chest pain, syncope, orthopnoea
- What other comorbidities do they have?
- What medications are they on?
- Have they needed any cardioversions, ever or recently?
What investigations may be of value in a patient with a pacemaker?
- ECG to assess intrinsic rhythm and rate, and whether pacemaker active
- Echo to assess LV and valve function
- Bloods including electrolytes, particularly magnesium, and digoxin level if relevant
- CXR for evidence of heart failure and to check position of pacemaker and leads*
- Recent angio reports to give an idea of how bad their coronaries are
*You can also tell the difference between an ICD and a PPM on the CXR by the presence of shock coils on the leads.
What do I do with the pacemaker in theatre?
Whether you're going to have to adjust or deactivate the pacemaker for the procedure depends on a few factors.
Type of device
- A standard pacemaker can often be left alone
- A CRT or ICD usually may need deactivating
How much electromagnetic interference do you expect?
- If you're using a tiny spot of bipolar diathermy on a leg - you can probably leave it alone
- If you're doing lots of thoracic or upper abdominal diathermy - might need to adjust it
How the pacemaker reacts to impulses
- If the pacemaker has been programmed to ignore everything and deliver shocks at a set rate, then it's not going to be dramatically affected by external electricity
- If it has a complex sensing set up with rate modulation then it will need deactivation so that the chaotic surgical signals don't confuse it
Can I use the big magnet?
Hold up, the answer is maybe.
Most implantable devices have a reed switch that will be triggered by placing a magnet over the device, however what effect this has will depend on the model.
- It might deactivate it completely
- It might put it into a default asynchronous mode
- It might start running diagnostics
Usually removing the magnet puts it right back to what it was doing before you got involved, and doesn't ruin everything, but you don't know unless you ask.
Loop recorders
You don't need to deactivate a loop recorder as there is zero risk of it shocking a patient by accident, however you can still damage the machine with lots of interference, so it's still a good idea to check with a cardiac physiologist first.
When it goes wrong
Let's say that despite being the fantastic and diligent anaesthetist that you are, the pacemaker still malfunctions during the operation and starts handing out boosts like an enthusiastic grandmother on halloween.
What can you do?
- You can start by knowing where the nearest cardiac electrophysiologist is before you begin the operation
- You can try percussive pacing
- Isoprenaline
- Adrenaline
- Some other form of pacing - transthoracic, transvenous or transoesophageal
Useful Tweets and resources
Here's an awesome infographic shared with permission from onepagericu.com
References and Further Reading



Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
Members Area
Test your knowledge!
Member-only Downloads
FRCA Questions
What are the causes of AV node block?
- Ischaemia
- Degenerative (hypertension)
- Infiltrative (amyloidosis)
- Iatrogenic (AV node ablation)
What are the indications for ICD insertion?
Anyone who is considered at high risk of sudden death from ventricular arrhythmia including:
- Familial Long QT syndrome
- Brugada syndrome
- Cardiomyopathy
- Some congenital heart disease
What is meant by the sensitivity of a pacemaker?
- The minimum intrinsic electrical activity in the atrium or ventricle that the pacemaker can detect
- Depends on the chamber being sensed and the type of leads in use
- If it is set incorrectly, it can either under-sense and not kick in when required, or over-pace when it's not needed
- This can lead to harmful tachyarrhythmias
Over-sensing is the main concern in theatre with regards to electromagnetic interference. The pacemaker may think that the diathermy is the heart's own activity and forget to pace, or a defibrillator may think it's a malignant rhythm and start trying to correct it with chest lightning.
Where are permanent pacemakers usually sited?
- Subcutaneously inferior to left clavicle
- Wires are transvenous via the left cephalic or subclavian vein
- In children they may be in the abdominal wall instead
- The atrial lead is usually in the right atrial appendage
- The ventricular lead is usually in the right ventricular apex
- A biventricular pacemaker will need a left ventricular lead as well, which is passed through the coronary sinus from the right atrium
What are the complications of pacemaker insertion?
- Lead displacement
- Pneumothorax
- Infection
What are the intraoperative risks associated with pacemakers?
Electrical interference
- Inappropriate triggering may lead to tachycardia
- Some pacemakers measure thoracic impedance, and so there maybe interference from the ventilator
- Diathermy - Risk of burns and damage to PPM, Bipolar is safest, Monopolar plate must be at least 15-20cm away from the PPM, Small current for short period of time must be used
Mechanical interference
- Shivering or fasciculations can interfere with pacemaker function
- Biochemical - Hyperkalaemia risks VT or VF, hypokalaemia risks loss of capture
Magnets
- Different pacemakers will respond differently to different magnets, so each should be checked on an individual basis
What are the indications for perioperative cardiac pacing?
Heart block
- Third degree (total)
- Symptomatic second degree
- First degree with LBBB or Bifascicular block (RBBB + either LAFB or LPFB)
MI
- Acute anterior MI
- Acute MI with Mobitz II heart block
Sick sinus syndrome
Faulty permanent pacemaker
Why are bipolar leads safer than unipolar leads?
- Unipolar leads have a cathode wire, and use the box itself as the anode
- Bipolar leads have an anode near the tip of the cathode wire
- This dramatically reduces how susceptible the pacemaker is to electromagnetic interference