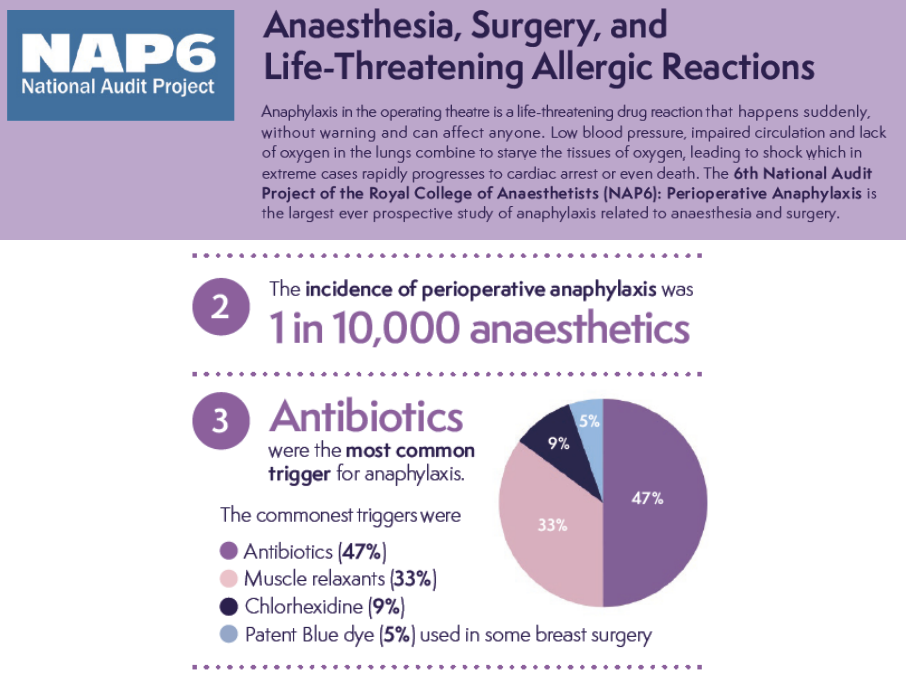
NAP 6
Take home messages
- The four most common triggers of perioperative anaphylaxis are antibiotics, muscle relaxants, chlorhexidine and patent blue dye
- Anaphylactoid reactions appear clinically similar, without the tryptase release
- Keep your wits about you - hypotension was the commonest presenting feature
Anaphylaxis is terrifying
We even said so in our post all about anaphylaxis, where we go through the ins and outs of the condition itself.
Today's post is a little different - we're talking specifically about the sixth national audit project, investigating specifically perioperative anaphylaxis.
As far as studies go, it's a big one - with over 11 000 anaesthetists reporting from over 300 hospitals in the UK.
In the UK we do about 3 million anaesthetics each year.
The big four
Let's get straight to it - the four classes of agent most commonly implicated in triggering perioperative anaphylaxis are:
- Antibiotics - 47%
- Neuromuscular blocking agents - 33%
- Chlorhexidine - 9%
- Patent Blue Dye - 4.5%
This only adds up to 93.5% - the remaining triggers included colloids, ondansetron and even our beloved propofol in one case.
Interestingly, latex didn't really feature.
Antibiotics
One would assume that a penicillin would be the likeliest culprit here, however teicoplanin was disproportionately implicated in NAP 6.
Despite only being used in 12% of cases, it caused 38% of the reactions in the antibiotic category.
Co-amoxiclav did manage to come in close second however, with a reaction rate of 8.7 per 100 000 administrations (Teicoplanin was 16.4).
Interestingly, teicoplanin was given in many cases because of a 'penicillin allergy', and ended up going on to cause a reaction itself. Given that it seems that over 90% of 'penicillin allergies' are not genuine allergies, it would likely have been safer to give the penicillin instead.
Muscle relaxants
No suprises here - suxamethonium was responsible for nearly twice as many reactions as other agents, and interestingly it tended to present with bronchospasm.
Atracurium, meanwhile generally caused a hypotensive picture.
There was one case of anaphylaxis that was thought to have been caused by sugammadex.
Chlorhexidine
Chlorhexidine tended to give a more insidious, slower onset reaction, and was fatal in one case during the study.
This was likely due to a combination of not spotting it early, and assuming it was caused by something else - only 25% of chlorhexidine reactions were correctly attributed to chlorhexidine.
Interestingly there was almost never any bronchospasm, and the presenting sign was almost always hypotension.
Patent Blue Dye
Much like chlorhexidine, the reactions triggered by patent blue dye were generally slower onset.
Again - no bronchospasm and mainly hypotension as the presenting issue.
Nobody died from anaphylaxis to the blue stuff, however six needed ICU admission.
So what does it look like?
Anaphylaxis looks different in the operating theatre than in the emergency department.
Instead of a wheezing, gasping patient with a swollen tongue clutching a cereal bar wrapper in their hand, you're often only alerted to the problem by an alarm beeping, suggesting one of your many physiological parameters just isn't quite right.
What were the commonest presenting features of perioperative anaphylaxis in NAP 6?
- Hypotension - 46% (but all patients became hypotensive at some point)
- Bronchospasm - 18%*
- Tachycardia - 9.8%
- Hypoxia - 4.7%
- Bradycarida - 3%
- Loss of ETCO2 trace - 2.3%
*This was particularly the case in morbidly obese patients and those with underlying asthma
Rash and itching were generally uncommon.
What was the mortality of perioperative anaphylaxis in NAP 6?
- There were 40 cardiac arrests*
- There were 10 deaths
*Note that CPR should be started if the systolic blood pressure is less than 50 mmHg
The presenting rhythm in most cases was pulseless electrical activity, frequently with bradycardia.
What features were associated with worse outcomes in perioperative anaphylaxis?
- Increasing age
- Increasing ASA grade
- Obesity
- Ischaemic heart disease
- ACE inhibitor or Beta-blocker
Do you have an anaphylaxis kit?
Many trusts have a dedicated anaphylaxis trolley, bag or kit of some sort, with everything you need for when it all goes horribly wrong.
NAP 6 found that only 37% of hospitals had a specific treatment pack - so if this applies to your hospital, there's another QIP for you.
It's nice to have a specific kit for someone to run and grab, because you're most likely going to be tied up trying to oxygenate the patient and coordinate the patient management, and you don't have much time.
How quickly does perioperative anaphylaxis generally present?
- In over 80% of cases, the reaction presented itself within the first 10 minutes of exposure to the triggering agent
- In 1-2% of cases, the delay lasted over an hour
Reactions triggered by muscle relaxants were particularly fast onset.
Don't be stingy with the fluids
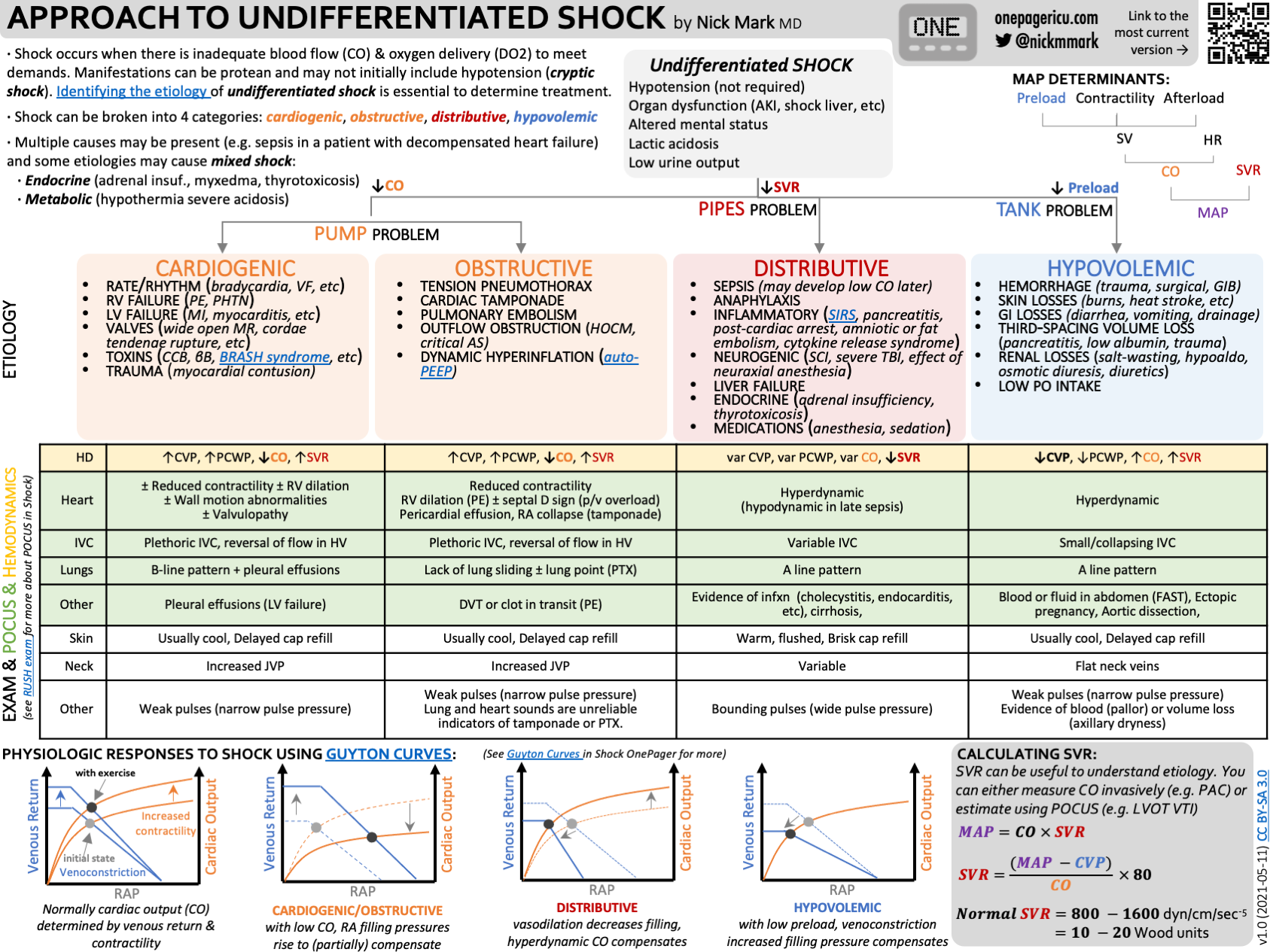
Anaphylaxis causes a rapid and profound distributive shock as a result of histamine-induced vasodilatation.
Therefore the ideal solution is to counteract with a vasoconstrictor, hence we give adrenaline (among other reasons).
However the sudden relative hypovolaemia particularly in the major vessels can be managed at least in part by rapid administration of balanced crystalloid solutions, and you may well need to give multiple litres of the stuff.
What should I do next?
So you've given the adrenaline, removed the trigger, filled the patient up with fluid and they seemed to have stabilised.
- Take a deep breath
- Postpone surgery unless essential
- Take tryptase levels
- Assume you're going to need a vasopressor infusion
- Admit to ICU
- Tell the patient
- Refer for formal investigation
Useful Tweets and Resources
NAP 6 infographic freely available here
An awesome infographic on a patient presenting with shock
Check out Dr Nick Mark's absolutely brilliant infographics here
How to manage CPR in the operating theatre
Many thanks to Chris Hellyar over at gasnovice.com for allowing us to share his very thorough guide.
References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
