Liver disease in pregnancy

Take home messages
- Liver disease in pregnancy isn't common, but can be very serious
- It might be completely unrelated to the pregnancy
- N-acetylcysteine improves outcomes in acute liver failure and does not appear to cause harm in the obstetric population
A terrifying duo
Obstetrics is scary, with delicate patients that can go downhill sportingly quickly should something go wrong.
Liver disease is scary, with delicate patients that can go downhill sportingly quickly should something go wrong.
So when you get liver disease during pregnancy it's all rather tense indeed.
What are your priorities as the anaesthetist?
- Figure out the cause
- Watch the coagulation like a hawk
- Deterioration can be rapid and precipitous
- Drug metabolism and handling is different
- Aspiration risk is higher
- Be ready for major haemorrhage
How do I figure out what's causing it?
If you think the liver is playing up, you first need to decide whether it's directly related to the pregnancy, or whether it's a separate liver disease process that's just coincidentally flaring up right now.
Pregnancy related
- Acute fatty liver of pregnancy
- HELLP syndrome
- Obstetric cholestasis
- Pre-eclampsia with liver dysfunction
Not pregnancy related
- Hepatitis - viral, autoimmune, drug induced
- Budd-Chiari syndrome
- Acute on chronic liver disease - alcohol, drugs, autoimmune
What are the normal changes in pregnancy?
You get lots of physiological changes during pregnancy as the mother's body prepares for labour, delivery and then subsequently feeding another human being.
Much of this is driven by increases in progesterone and oestrogen, affecting the whole body including the liver.
- Transaminases drop by around 25% during pregnancy, then increase postnatally
- ALP increases in the third trimester (produced by the placenta)
- GGT increases in the postnatal period
As a result, liver disease can be rather tricky to spot, especially when palmar erythema and spider naevi are normal features of pregnancy as well.
What do the different conditions look like?
If you're the labour ward anaesthetist, and you think something liver-y is going on, it's usually one of the following four conditions, each with their own pattern of blood results.
Acute fatty liver of pregnancy
- ALT increased by up to 15 times normal
- Bilirubin increased by up to 15 times normal
- Bile acids usually normal
HELLP syndrome
- ALT increased by up to 30 times normal
- Bilirubin increased by up to 10 times normal
- Bile acids usually normal
Pre-eclampsia with hepatic impairment
- ALT increased by up to 5 times
- Bilirubin usually normal
- Bile acids usually normal
Intrahepatic cholestasis of pregnancy
- ALT increased by up to 8 times
- Bilirubin usually normal
- Bile acids increased by up to 15 times
What on earth is hepatic angina?
This is a severe right upper quadrant pain occurring in parturients with severe pre-eclampsia, which should be taken terribly seriously as it potentially heralds impending liver dysfunction.
What are the indications for platelet transfusion in HELLP syndrome?
- If patient is actively bleeding
- To facilitate surgery
- To facilitate insertion of invasive lines
How do you treat HELLP syndrome?
- Same as you would for severe pre-eclampsia
- Supportive ABC management
- Correct the correctables (clotting, anaemia, platelets, sugar, electrolytes)
- Deliver the foetus
Acute Fatty Liver of Pregnancy
You might have been able to work this out from the name, but this disease process involves progressive fat accumulation within hepatocytes during the third trimester.
- Some consider it to be a variant of pre-eclampsia
It is thought to occur as a result of dysfunctional fatty acid metabolism, and it affects between 1 in 7 000 and 1 in 20 000 pregnancies.
Left unchecked, this will descend into liver dysfunction and ultimately multiple organ failure.
- The mortality has thankfully dropped from 85% down to around 15% for the mother
- The perinatal mortality remains around 25%
Who gets it?
You'll have probably noticed the same group of risk factors cropping up for all sorts of pregnancy-related ailments:
- Multiparity
- Diabetes
- Pre-eclampsia
- Cholestasis
- Family history
There's also:
- Low BMI <20
- Male baby
- Long chain acetyl CoA dehydrogenase deficiency (literally a condition where fat builds up because you can't break it down)
What does it look like?
As with many insidious liver conditions, the presentation can be vague and non-specific:
- Nausea
- Vomiting
- Fatigue
They will almost certainly also have:
- Hypertension
- Proteinuria
- Pruritus
Bloods may also show:
- Metabolic acidosis
- Hyperlactataemia
- Hypoglycaemia
What are you looking for in the history and examination?
History
Symptom onset, duration and severity
- Abdominal discomfort
- Itching
- Dark urine
- Pale stools
- Fatigue
- Recent drugs, travel or other illness
- Family history of liver problems
Examination
- Stigmata of chronic liver disease
- Ascites
- Jaundice
- Right upper quadrant pain
How is it diagnosed?
- Use the Swansea criteria
You need at least six of:
- Vomiting
- Abdominal pain
- Ascites
- Polydipsia/polyuria
- Elevated transaminases
- Encephalopathy
- Leucocytosis
- Hyperammonaemia
- Hyperbilirubinaemia
- Renal dysfunction
- Coagulopathy
- Hypoglycaemia
- Microvesicular steatosis on biopsy (probably not gonna use this one much in a DGH labour ward)
There also needs to be no other decent explanation for the patient's symptoms.
How would you manage a patient with acute fatty liver of pregnancy?
- ABCDE assessment to begin with, as always
- HDU or ICU environment on Labour ward
- IV access
- Cautious IV fluid resuscitation as required - risk of ARDS and peripartum cardiomyopathy
- Correct hypoglycaemia
- Correct coagulopathy - use TEG/ROTEM if possible
- Deliver the foetus - general anaesthesia if coagulopathic
- Expect renal and hepatic function to get worse over next 48 hours
- May require intubation for encephalopathy or respiratory failure
- May require renal replacement therapy - if refractory acidosis, fluid overload, hyperkalaemia or symptomatic uraemia
Platelets generally remain fairly steady in AFLP, compared to HELLP where they can drop precipitously.
Non-pregnancy related liver stuff
Viral hepatitis
- Commonest cause of liver dysfunction and jaundice during pregnancy worldwide
- Can be Hepatitis A, B, C, D, E, G, HSV, CMV, EBV
- Most of the time it's Hep E to blame
- Vertical transmission to the foetus is possible
- It can also be reduced through immunisation (for Hep B)
- Presentation is similar to non-obstetric patients, however HSV hepatitis appears to be more severe in pregnancy
- Obstetric complications include intrauterine growth restriction, premature rupture of membranes and delivery and increased perinatal mortality
Autoimmune
- Usually gets better during the relatively immunosuppressed period of pregnancy
- Immunosuppressive medication should be continued
- Tacrolimus, ciclosporin and azathioprine are all safe
- Mycophenolate is teratogenic
Cirrhosis
- Cirrhosis in pregnancy brings a high mortality of around 10%
- Pregnancy makes portal hypertension worse
- This makes varices worse
- C-section is advised as straining during labour increases risk of rupture
There's also the additional complications to consider such as ascites, decompensation and encephalopathy, as well as a raised mortality overall.
Transplant
- You can essentially treat a woman with a liver transplant as you would any other parturient
- Assuming their liver function and coagulation are normal
- They should keep their immunosuppression going throughout pregnancy
- They're at higher risk of PET, gestational diabetes and pre-term delivery
Budd-Chiari
- The hepatic vein is obstructed, most of the time by thrombosis
- This leads to hepatomegaly and ascites
- There may also be right upper quadrant pain
- There is increased risk of early foetal loss
Drugs
- Drugs can cause liver injury
- Methyldopa
- Paracetamol
- Retrovirals
- Hormones
- Psychotropics
- Carbamazepine
What to do about it?
This is going to surprise you, but women with severe liver disease who are also pregnant should probably have an individualised, multi-disciplinary care plan with adequate antenatal assessment and discussion.
Crazy, we know.
Things to think about:
- A damaged liver will process drugs differently - both metabolism and excretion
- This will be compounded by concomitant renal dysfunction
- This doesn't tend to have a dramatic impact on your anaesthetic plan
- Liver disease = less plasma cholinesterase = less suxamethonium metabolism however this is largely academic, especially if you're not using sux in the first place
- Liver disease = prolonged and unpredictable duration of rocuronium = irrelevant if you're using sugammadex
- Inhaled agents are as safe as we can make them, and no worse in the context of liver disease for a general anaesthetic caesarean section
- Avoid NSAIDs for renal and coagulopathy reasons
- Your uterotonics should be given at standard dose
- Cell salvage is fine for cases with non-malignant liver disease
- Encephalopathy can be insidious and tricky to spot - forgetfulness and terrible sleep are also symptoms of pregnancy and having a small baby
Can I use regional anaesthesia in parturients with liver disease?
- Yes if the disease is relatively mild and crucially stable
- The risks and benefits, as always, need thorough discussion with the mother
- Avoid in a haemodynamically unstable coagulopathic emergencies with dubious ability to provide fully informed consent
Useful resources
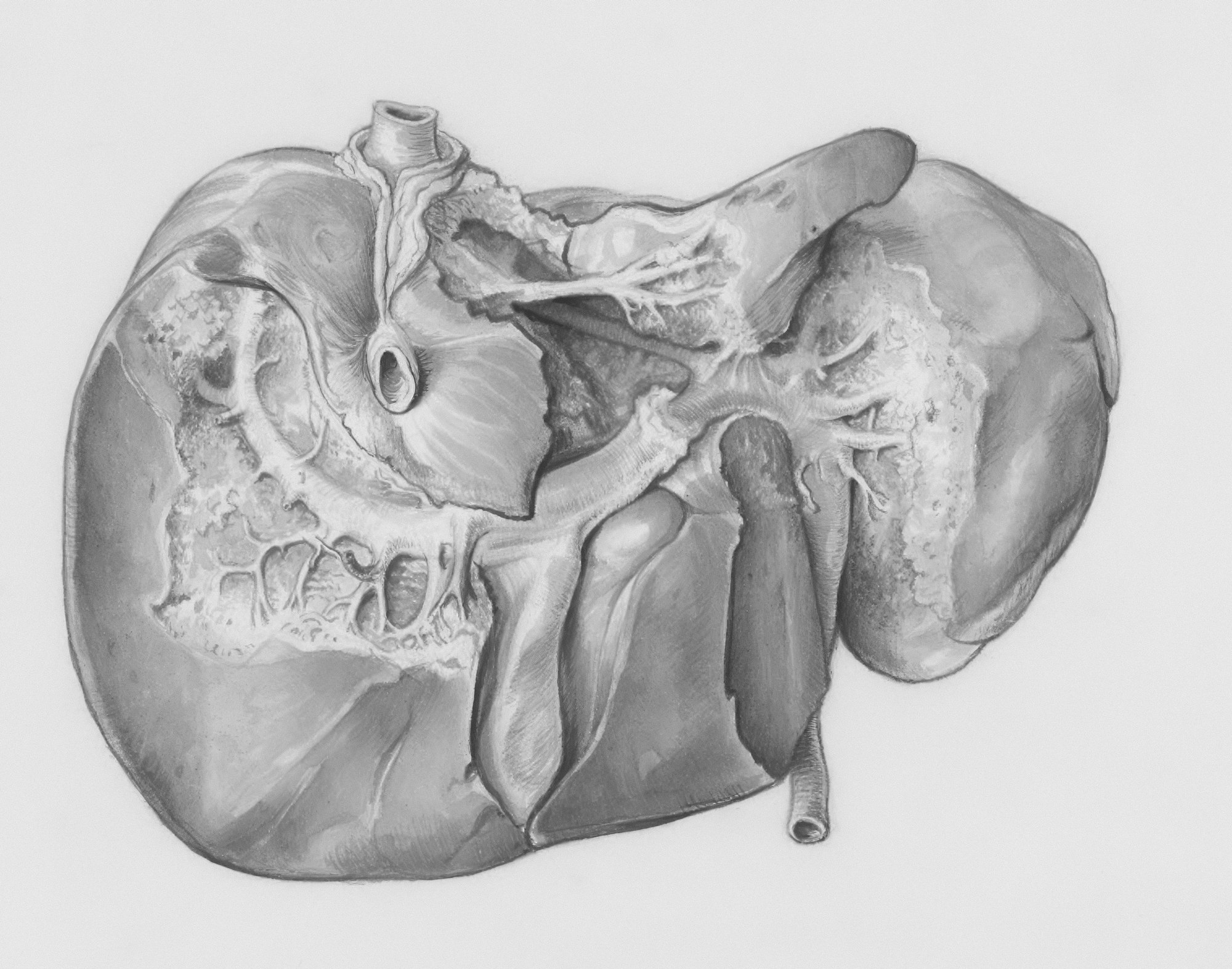
HELLP Syndrome Post Partum with Liver Bleed and Infarction pic.twitter.com/WYMNbHY9gZ
— Elliot K Fishman / CTisus.com (@ctisus) December 15, 2025
Pregnancy and the liver
— Elliot Tapper (@ebtapper) February 13, 2025
A masterclass by @MussaratRahim in @TheLancet
1. Comorbid disease
2. Liver disease caused by pregnancy
3. Drug safety
4. Ongoing trials pic.twitter.com/Qe1cJCsPro
Here are our other liver posts


References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
Anaestheasier® is a registered trademark.
Members Area
Test your knowledge!
Member downloads
Brainscape Flashcards
Freely available to Anaestheasier members, this is a live set of flashcard decks, meaning we're continuing to add to them and improve them over time.
Rather than building the decks and then releasing them later, we wanted to make them immediately available for you to start using, and also for your feedback.
If you spot any errors or have any comments then please do get in touch and let us know!

If you're already a user of Brainscape and have decks that you'd like to share with us, please email us at anaestheasier@gmail.com (financial compensation and teaching certification available).
FRCA Questions
What is the differential diagnosis for deranged LFTs in pregnancy?
This can be broken down into those conditions that are directly related to the pregnancy, and those that can happen at any time.
Pregnancy related
- Acute fatty liver of pregnancy
- HELLP syndrome
- Obstetric cholestasis
- Pre-eclampsia with liver dysfunction
Not pregnancy related
- Hepatitis - viral, autoimmune, drug induced
- Budd-Chiari syndrome
- Acute on chronic liver disease - alcohol, drugs, autoimmune
What are the most common causes of hepatic complications in pregnancy?
- HELLP syndrome (haemolysis, elevated liver enzymes, low platelets)
- Acute fatty liver of pregnancy
- Intrahepatic cholestasis of pregnancy
- Pre-eclampsia with hepatic dysfunction
The first two are the most common causes of intensive care admission for liver failure.
What is the definition of acute liver failure?
- Rapid onset severe liver injury
- With impaired synthetic function (coagulopathy)
- And hepatic encephalopathy
- In a patient without pre-existing chronic liver disease or cirrhosis
What features are particularly concerning for liver disease in pregnancy?
- A lactate of more than 2.8
- Encephalopathy
This signifies an impaired ability of the liver to clear lactate, and severe end organ dysfunction.
How is encephalopathy graded?
- Grade 1 = mild confusion, slurred speech
- Grade 2 = lethargy, moderately confused
- Grade 3 = sleepy but rousable
- Grade 4 = coma
What is the definition and pathophysiology of acute fatty liver of pregnancy?
- Progressive fat accumulation within hepatocytes during third trimester
- Eventually leads to liver dysfunction and multiple organ failure
- Historically associated with 85% maternal and foetal mortality
- Current maternal mortality estimated at 10 to 20%
- Perinatal mortality remains around 20 to 30%
- Presumed to be due to dysfunctional fatty acid metabolism
- Incidence is approximately 1 in 7,000 to 20,000 pregnancies
How is acute fatty liver of pregnancy diagnosed?
- Clinical diagnosis of exclusion
Swansea criteria (6 of the following needed)
- Vomiting
- Polydipsia or polyuria
- Abdominal pain
- Encephalopathy
- Bilirubinaemia
- Hypoglycaemia
- Raised urate
- Raised WCC
- Raised transaminase count
- Ascites
- Coagulopathy
- Renal failure
- Microvesicular steatosis seen on biopsy
What investigations are of value when suspecting acute fatty liver of pregnancy?
Liver function tests
- Transaminases elevated 3–10x in AFLP
- Raised alkaline phosphatase
- Hyperbilirubinaemia is more marked than in HELLP
Urea and electrolytes
- Hyperuricaemia often disproportionate to other pre-eclampsia signs, helping to differentiate from pre-eclampsia
Other parameters may also be raised
- Amylase
- Lipase
- Ammonia
Full blood count
- Haemolysis
- Thrombocytopaenia
Others
- Coagulation studies
- Blood sugar
Imaging
- Ultrasound
- MRI
Biopsy
- Definitive diagnosis but invasive and high risk if coagulopathic
- Microvesicular steatosis
- Fibrin deposits
- Haemorrhage
What are the risk factors for acute fatty liver of pregnancy?
- Multiparity
- Diabetes
- Pre-eclampsia
- Cholestasis
- Family history
- Low BMI <20
- Male baby
- Long chain acetyl CoA dehydrogenase deficiency
What effects of obstetric cholestasis are of interest to the anaesthetist?
- Impaired excretion of bile acids leads to uncomfortable pruritus
- Vitamin K malabsorption can affect coagulation
- It can herald more severe liver disease, so needs close monitoring
What are the classes of acute liver failure?
This is generally accepted as the time interval between jaundice and encephalopathy.
- Hyperacute - <7 days - high cerebral oedema risk but relatively good prognosis
- Acute - 8 - 28 days - moderate risk and prognosis
- Subacute - 5 - 12 weeks - low oedema risk but poor prognosis
Hyperacute is usually caused by paracetamol, hepatitis or ischaemia.
Acute is usually caused by drug reactions or viral hepatitis (A and B).
Subacute is caused by autoimmune disease, Wilson's disease, Budd-Chiari, malignancy or Hep B and C
What are the risk factors for undiagnosed chronic liver disease?
- Alcohol excess
- Ascites
- Platelets <160
- Spider Naevi
- ALT/AST ratio <0.7
- INR >1
What are the most severe complications of PET?
- Pulmonary oedema
- Eclampsia
- Subcapsular liver rupture
- Intracranial haemorrhage
- Cerebral oedema
- Hypertensive encephalopathy




