I failed a spinal

‘Two conditions are, therefore, absolutely necessary to produce spinal anesthesia: Puncture of the dura mater and subarachnoid injection of an anesthetic agent.’
Gaston Labat, 1922
Please believe me, dear reader, when I say I am well versed with the delicate art of completely messing up a spinal anaesthetic.
While I'm pleased to say that I am now generally becoming rather more proficient at the dark art of injecting heroin into the spines of the elderly, every so often along wanders an opportunity to thoroughly humble myself once more.
Invariably this is in front of a new consultant who has obviously already decided I'm a completely incompetent individual.
So now for your entertainment, information and reassurance - here are some of the ways my spinals have 'deviated' somewhat from the original plan.
Ways in which I've messed up a spinal include:
- Knocked the whole tray on the floor
- Dropped the spinal needle
- Dropped the introducer
- Dropped the spinal needle, followed by the introducer
- Dropped the spinal needle and instinctively picked it up, rendering myself unsterile so I had to start all over again
- While injecting the local anaesthetic, disconnected the needle and sprayed local anaesthetic into my consultant's eye
- Sprayed local anaesthetic in my own eye
- While injecting the spinal mixture, disconnected the needle and sprayed half the bupivacaine mixture up the patient's back
- Spent a good thirty seconds staring at my tray, looking for the loss of resistance syringe, forgetting I'm supposed to be doing a spinal and not an epidural
But this time it was different
I take zero issue with admitting the fact that sometimes it's a case of 'operator error'.
Throughout the last few years I have spent many sweaty minutes bouncing my needle off laminae and vertebral bodies, praying the consultant would just hurry up and slap some gloves on to take over.
Maybe I hadn't positioned the patient correctly, or I was feeling rushed, or didn't use enough force, or used too much - either way most of the time I can understand why it didn't work out.
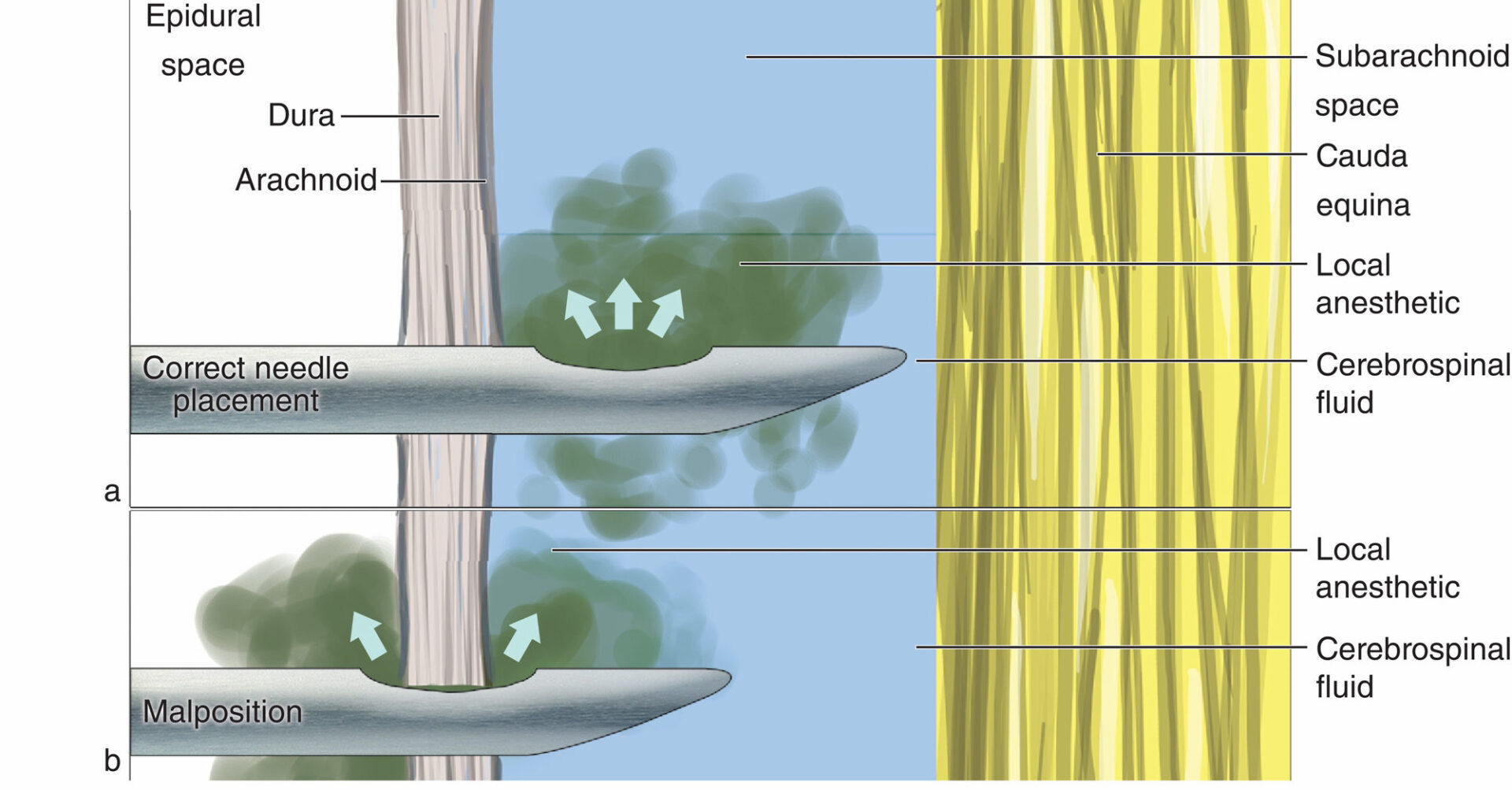
But on this occasion I had found the right space and experienced that delectable moment of watching crystal clear CSF trickle back along the needle, before injecting the anaesthetic with no trouble at all.
Here's what happened
- 50 year old woman with well controlled epilepsy, hypertension and reflux
- Scheduled for elective right hip replacement
- Previously had a left hip replacement under spinal anaesthesia with sedation, and so happy to do the same today
- Position optimised, sat up awake on the side of the bed
- Midline easy to locate
- Introducer needle inserted and spinal needle advanced through reassuringly resistant ligaments
- On the first attempt contacted bone, and despite adjusting the angle of approach, wasn't able to locate the subarachnoid space
- Second attempt at a higher spinal space, easily located the space with reassuring flow of CSF back through the spinal needle
- Attached syringe with spinal injectate mixture, aspirated to confirm free flowing CSF, then slowly and smoothly injected
- At the end of the injection, aspirated gently again to confirm CSF still flowing, and needle therefore in the correct space, before removing the needle and applying a dressing
There is no way that drug did not go into the subarachnoid space.
But fifteen minutes later, the woman was still lifting her legs up, fully sensate, and clearly thought I was a moron.
So I did some reading.
Maybe this happened
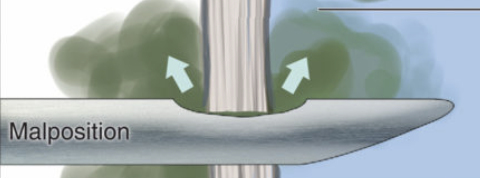
Unsurprisingly the vast majority of the time a spinal fails due to procedural issues, meaning no drug actually enters the intended space. However apparently, on average, a spinal fails to do what it says on the tin about 3% of the time even when the technique has been performed correctly.
Factors affecting spread of local anaesthetic throughout the CSF include:
- Spinal canal anatomy*
- Injection speed
- Use of hyperbaric local anaesthetic solution
- Positioning of the patient
Cysts, ligaments, adhesions, previous injuries and surgery can all affect how CSF, and therefore local anaesthetic, flows throughout the spinal canal
So what did we do next?
You can try another injection after a failed spinal - just as you might try another vertebral level when you can't find the space - but you need to be cautious about the fact that you've already tried once:
- There is a risk of local anaesthetic toxicity
- There is the increased risk associated with performing a neuraxial procedure twice
- There is potential for a delayed effect from the first dose resulting in a high spinal
The other option is to abandon neuraxial blockade and use general anaesthesia or more regional techniques as appropriate.
In our case, we hadn't yet started any sedation, so we could maintain a coherent conversation with the patient. We explained the situation, the fact that the spinal went as expected but for some reason wasn't working, and we came to an agreement to go off to sleep.
Some sevo and an IGEL later, the hammering could commence, and we noted that during the more stimulating parts of the procedure, her heart rate was increasing confirming that the block wasn't sufficient, and we had probably made the right call with a general anaesthetic.
After the procedure she woke up relatively comfortable and her pain was well managed with a fentanyl PCA.
So what did I learn?
- Always consent for general anaesthesia as a back up plan
- No matter how much science you learn, there is always some unexplained magic at play
- Don't beat yourself up when it doesn't go to plan
Other interesting facts about spinal anaesthesia
- The concentration of anaesthetic in the cerebrospinal fluid varies enormously and doesn't correlate at all with block height
- The concentration of anaesthetic in the CSF in failed spinals is often still considered enough, so the cause of the failure is thought to be due to distribution failure of the drug throughout the spinal canal
- The less csf you have in the lumbar spine, the higher the block is likely to go
- There isn't a correlation between height, age or weight and the height or density of the block
Useful Resources
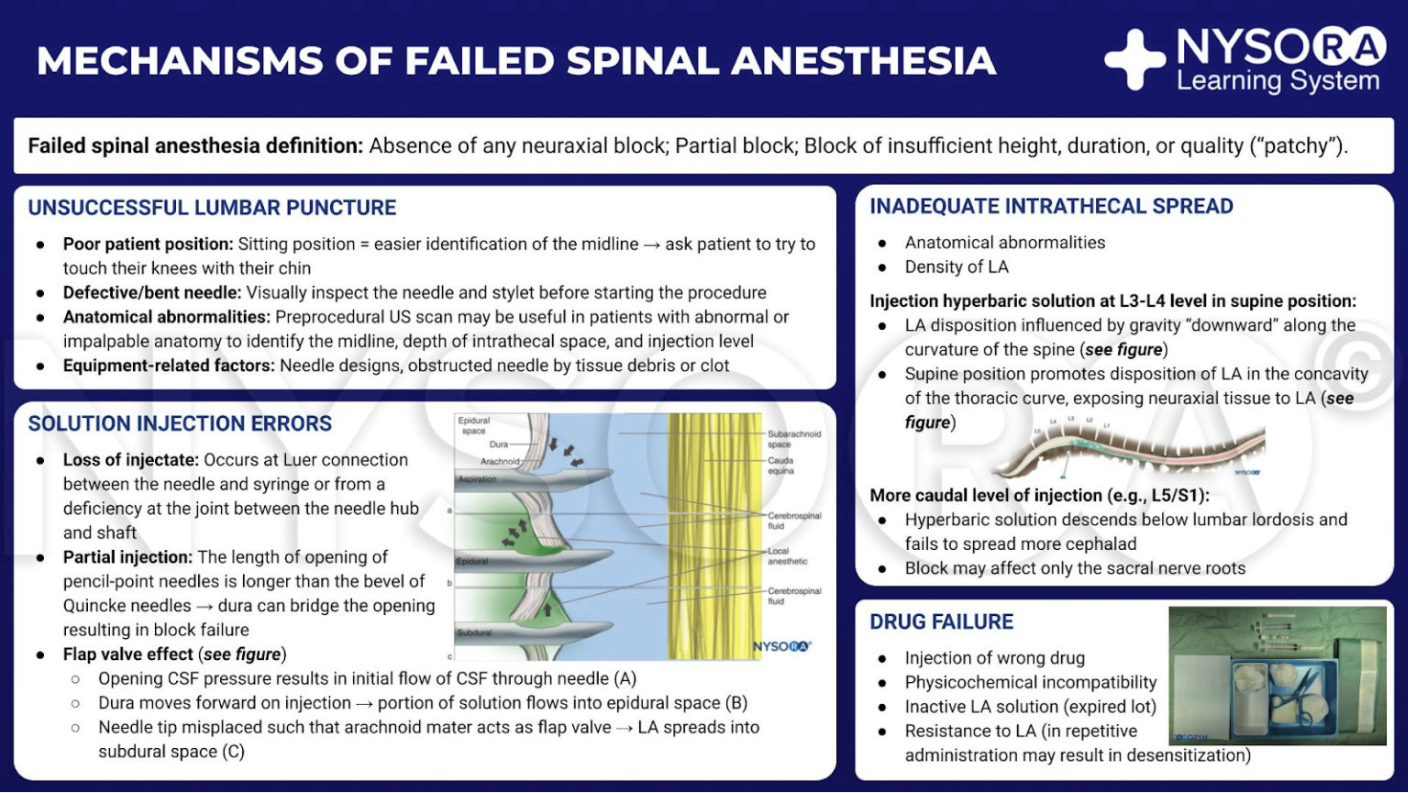
This infographic from the following article written by the wonderful people at NYSORA contains all you need to know and more so definitely go and check it out.
#Infographics MANAGEMENT OF FAILED SPINALS
— Shiv Kumar Singh (@ShivRoyal) May 21, 2023
"Two conditions are, therefore, absolutely necessary to produce spinal anaesthesia: puncture of the dura mater and subarachnoid injection of an anaesthetic agent."
Gaston Labat, 1922 pic.twitter.com/eZtbowjzP0
Reference