Hyperthermic syndromes

You have a hot, agitated and rigid patient in front of you.
What is causing it and what do you do?
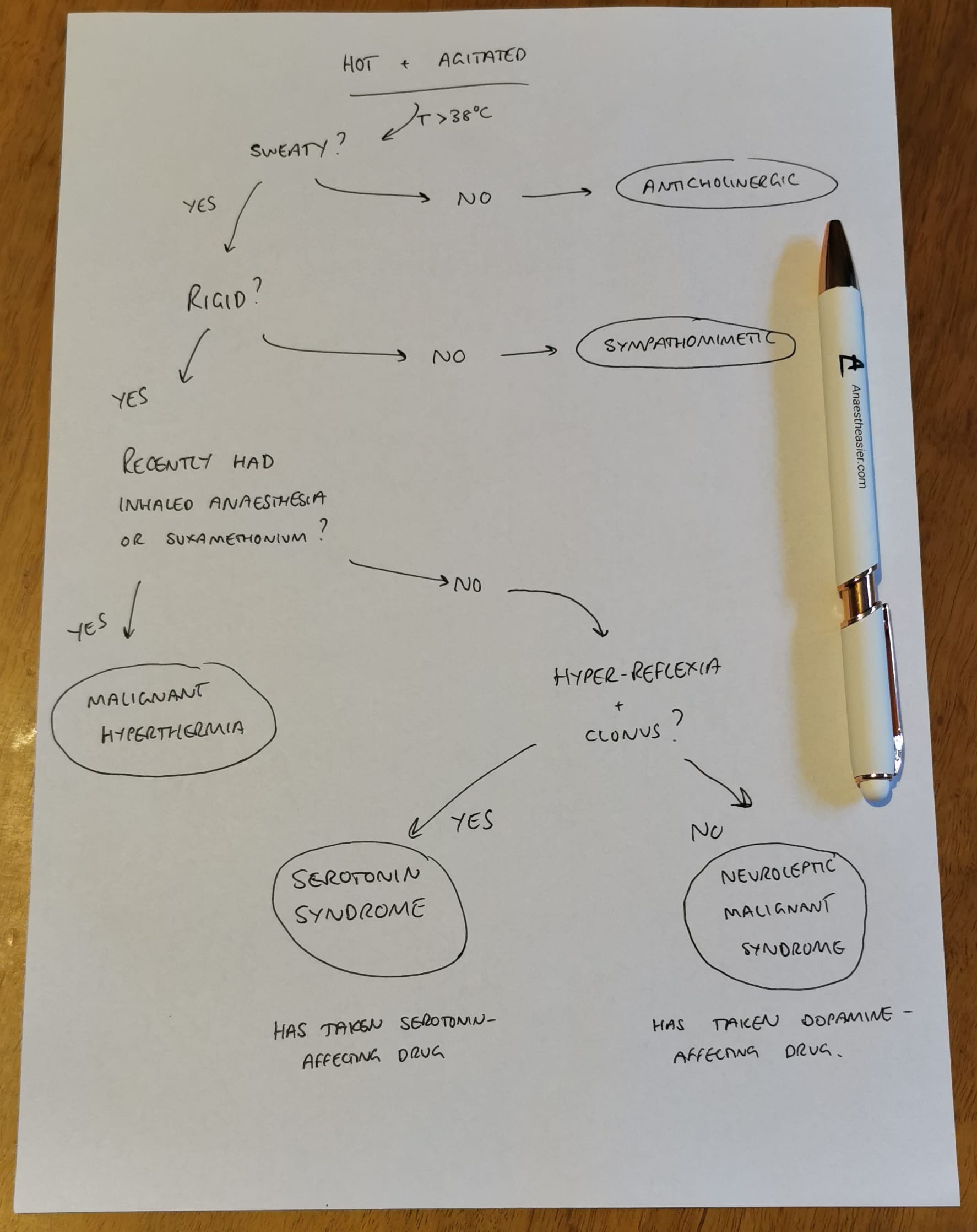
A quick reference flow chart
As you amble towards resus, hopefully you've been given enough history over the phone to work through this rather simplified flow chart to figure out what might be going on.
How to tell them apart
Anticholinergic
- The key distinguishing factor here is they're hot and dry, not sweaty
- They've usually taken antihistamines, antimuscarinics or TCAs in the last few hours
- This is also how deadly nightshade kills you
- They'll also have urinary retention, which none of the other conditions will cause
Red as a beet, dry as a bone, mad as a hatter, blind as a bat and hot as a hare.
Don't forget eye drops can cause this in kids.
Sympathomimetic
- They've recently taken some fun stuff and thrown themselves into adrenergic overdrive - think meth, cocaine, MDMA
- They're desperately sweaty and very hypertensive but not rigid
- Pupils, muscle tone and reflexes are generally normal
- Use non-selective beta blockers (labetalol) to bring down the blood pressure, temperature and heart rate
This is how body packers can present, when one of the packs ruptures and they overdose immediately on whatever they're smuggling - consider a CT to confirm.
Theophylline can also cause this, and can be removed with haemofiltration.
Malignant hyperthermia
- More likely to be seen in theatre than resus
- They've had recent exposure to volatile anaesthetics or suxamethonium
- Hot, sweaty, and rock hard rigidity
- CO2 and temperature both climbing rapidly
- Treatment is switching to TIVA, active cooling and dantrolene
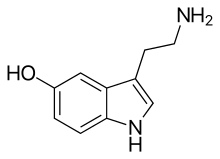
Serotonin syndrome
- They need to have taken something that triggers serotonin release, and usually more than one drug is involved (like an SSRI and then cocaine)
- It's pretty quick onset - a few hours after taking something
- Look for clonus and hyperreflexia
- Pupils are dilated and they may have ocular clonus too
- Use the Hunter or Sternback criteria
- Treatment is supportive, benzos and cyproheptadine
Neuroleptic malignant syndrome
- They're taking drugs that affect dopamine (antipsychotics and Parkinson's meds, some antiemetics)
- Slower onset - a few days after taking or stopping something
- Pupils are normal
- There is no clonus, and slow reflexes, with a lead pipe rigidity
They need some form of dopamine agonist such as bromocriptine fairly pronto.
What to do next
The treatment for all of these is largely the same - supportive optimisation of physiology until they sort themselves out.
So even if you can't figure out which is the actual diagnosis, you can still help make them better.
Airway
- No surprises here, if it's compromised, uncompromise it
- For conditions where muscle tone is causing the heating issue, rocuronium is going to be extremely therapeutic
Avoid suxamethonium, for hopefully obvious reasons.
Breathing
- In all of these cases the patient is relatively or severely hypermetabolic, and churning out vast quantities of carbon dioxide
- You will almost certainly need to hyperventilate them, both to blow off the CO2, and to counteract the steaming metabolic acidosis brewing beneath
Circulation
- Active cooling - cold wet towels, IV fluids, remove layers, fans
- Often hypertensive and very dehydrated
- Ensure adequate filling before induction of anaesthesia
- Support with pressors as required
Paracetamol is going to do nothing for this temperature.
Disability
- They may be agitated, confused, seizing or comatose (or all of the above)
- This may require intubation in its own right
- Either way you want to give benzodiazepines
Exposure
- Don't forget to check for injuries, rashes, bleeding and other external clues
- Only consider activated charcoal if airway secure, very recent ingestion and toxin known to bind (check toxbase)
- You might consider an NG tube for cyproheptadine
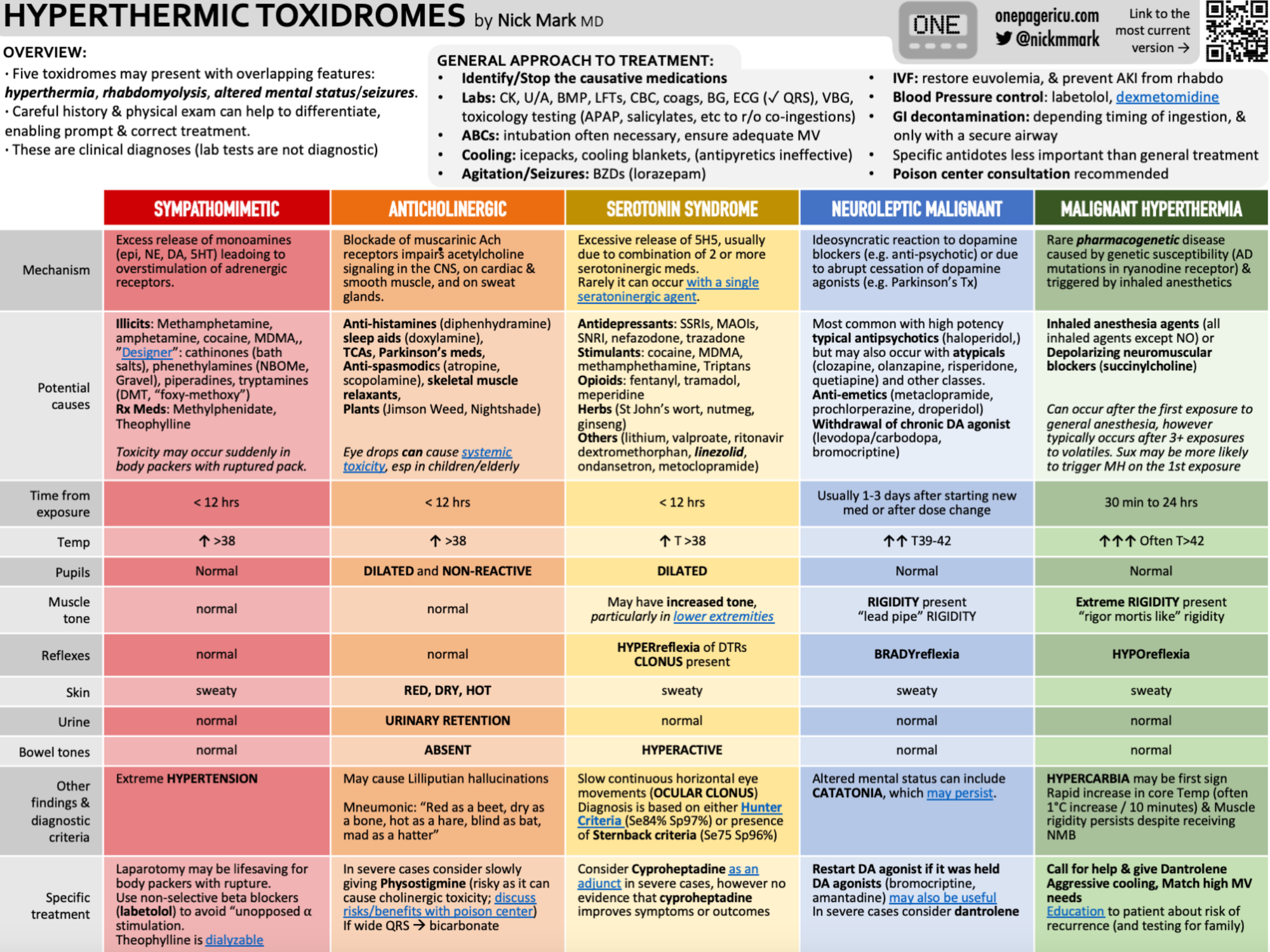
An awesome infographic
Here's all the information in one hot infographic shared with permission from the legendary Dr Nick Mark over at ICU one pager.
Related posts and further reading


Toxins and treatments
Here's a great summary of toxins and antidotes from Dr Yartsev at Deranged Physiology.
Coffee?