Hyperoxia

Take home messages
- Oxygen is good if you need it, and terrible if you don't
- Aim for sats of 92-94% unless otherwise directed
- Prescribe your oxygen
Alicia Keys was right
This girl is on fire.
We all are - technically speaking - a bit on fire when you consider the fact that our cells are producing energy via the heat-generating oxidation of hydrocarbons.
Either that or we're rusting, but that doesn't sound nearly as cool.
Even at its point of discovery in 1771, Carl Wilhelm Scheele called oxygen 'fire air' such was its propensity for ignition and destruction, so you won't be surprised to discover that oxygen can end up doing rather a lot of damage if not used carefully by our intracellular mechanisms.
Using oxygen for intracellular energy generation is rather like using a nuclear reactor to heat your living room.
It works - and very well indeed - but it's rather hazardous, so you'll probably want some safety mechanisms in place.
- The key problem is those dastardly reactive oxygen species
- Unsurprisingly the lungs take the hardest hit, because they're the organ that receives the most oxygen
- It usually takes more than 24 hours for clinical effects to show up
What is Hyperoxia?
There's no specific formal definition of what constitutes hyperoxia, other than 'a state of excess oxygen in the tissues' or 'higher PaO2 than normal', but it's not a particularly complex concept to get your head around.
A key thing to note is there are two types of hyperoxia:
- Normobaric hyperoxia - normal atmospheric pressure, high inspired O2%
- Hyperbaric hyperoxia - higher than atmospheric, but can still only be 21% O2
(If you're breathing 21% oxygen at 2 atmospheres of pressure, your lungs are exposed to 42 kPa of oxygen - which is still hyperoxia)
The cascade
We know that oxygen moves down its partial pressure gradient as it moves through the body, which explains why the lungs are the most affected by high partial pressures of oxygen, because they take the biggest whiff of the ol' fire air.
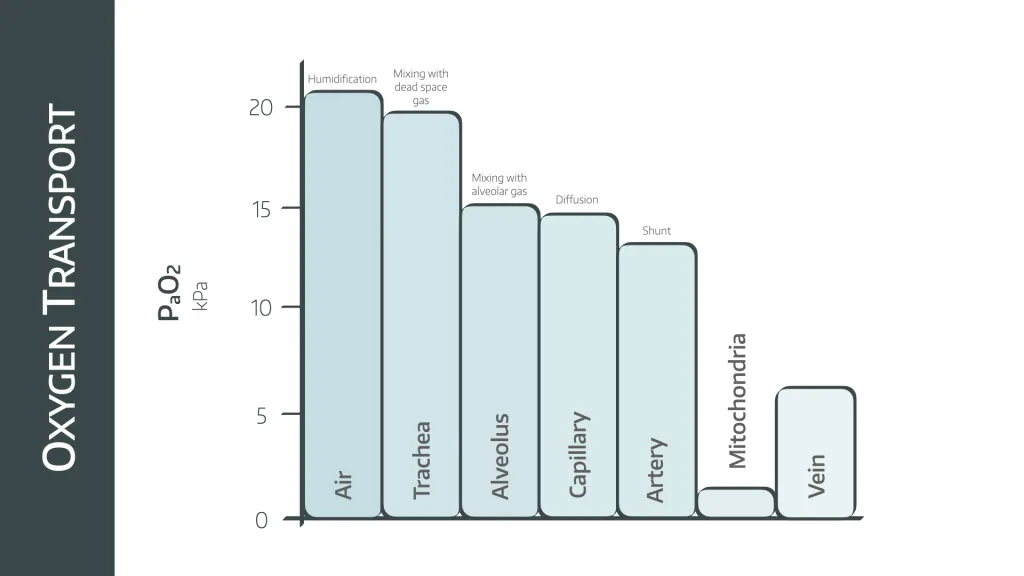
- You can only really become hyperoxic by receiving a greater FiO2
- Yes, according to the alveolar gas equation, you can increase PaO2 by hyperventilating and decreasing PaCO2
But this isn't nearly as clinically significant as whacking someone on 60-100% oxygen for hours or days at a time, as you're only looking at about 16 kPa maximum by hyperventilating, and you wouldn't be able to keep that up for very long anyway.
A brief reminder
Of course you'll remember exactly how the electron transport chain works without even having to think about it, in case you'd like a quick reminder...
- Oxygen as an element is reduced to water by the electron transport chain in the mitochondria
- This process drags protons kicking and screaming across the mitochondrial membrane against their concentration gradient
- They're then allowed to fly back down their concentration gradient, driving the inner workings of ATP synthase and hey presto - energy
But there's a problem.
Some of these 'high energy' protons and electrons effectively 'leak' out and start generating all sorts of other nasties called 'reactive oxygen species' (a.k.a. oxygen free radicals).
The two to be able to list in an exam are:
- Superoxide (O2 with an extra electron)
- Hydrogen peroxide
Not only do these two do damage themselves, they then go on to produce even more free radicals as well, including:
- Singlet oxygen
- Hydroxyl radical
Like an orthopod holding an ECG, the hydroxyl radical is extremely unstable, and immediately interacts with any nearby species it can find.
This sets up a continuous cycle of free radical production, and you can imagine how that ends.
Now don't get me wrong, these free radicals are useful for their antimicrobial properties, they're just a little troublesome because they're well, anti-everything.
- They tear apart DNA and RNA
- They impair DNA repair machinery
- They damage cell membrane structure
- They mess with protein function by oxidising random amino acids
You don't live very long if they're allowed to hang around.
Antioxidants
Rather than merrily bleaching itself into oblivion, the cell has fortunately developed some rather splendid methods of defending itself from said aforementioned nuclear reactor, by producing and employing antioxidants.
Some antioxidants
These can by enzymatic or non-enzymatic
Enzymatic
- Superoxide dismutase
- Glutathione peroxidase
- Catalase
Non-enzymatic
- Beta-carotene
- Uric acid
- Ascorbic acid
- Glutathione
These ROS-busting superheroes are the multi-talented guardian angels of the body:
- They can prevent ROS production in the first place
- They can scavenge and inactive ROS molecules
- They prevent damage to DNA and RNA
- They can also make Gwyneth Paltrow very rich indeed
That's probably all you need to know for the FRCA*
*not the Gwyneth Paltrow bit.
What happens in hyperoxia?
The main issue is that the delicate balance of oxidants and anti-oxidants is disrupted, with potentially disastrous consequences to which we probably don't pay sufficient heed.
We'll start with the pulmonary toxicity aspect of hyperoxia, as usually this is the most dangerous bit for your patient.
If you sit with an inspired oxygen concentration of greater than 60% for more than 24 hours then you start to see damage to the epithelium of the upper airways.
This can produce chest pain, shortness of breath and a sense of retrosternal tightness.
You also start to see the first measurable lung parameter changes - a drop in vital capacity.
Pulmonary toxicity occurs in four stages:
- To start with, in the initiation phase, the increased partial pressure of oxygen starts churning out enormous quantities of reactive oxygen species, setting up an oxidant:antioxidant imbalance
- This triggers the inflammatory phase, featuring surfactant disruption as well as epithelial and endothelial damage in the alveolus and capillary respectively, leading to pulmonary oedema, increased cytokine production and activation of the immune system
- We then saunter gracefully into the proliferative phase, with increased type II pneumocyte secretions and activation of the clotting cascade and widespread production of microthrombi
- Finally we end up in the fibrotic phase, where permanent lung damage is caused by deposition of collagen and fibrotic lung changes
Other organs
So here it gets rather interesting, because there's a strange paradoxical phenomenon where hyperoxia induces both hyperventilation and vasoconstriction in much of the systemic vasculature.
As a result, the resulting DO2 to vital organs including brain and heart can actually end up being lower than if you hadn't given any supplemental oxygen in the first place.
Neurological effects
These are mainly due to reduced cerebral blood flow as a result of vasoconstriction.
- Nausea
- Headache
- Muscle twitching
- Dizziness
- Visual changes
- Confusion
- Seizures*
*This is thought to be due to a combination of reduced cerebral blood flow, as well as the interactions of GABA and nitric oxide, and only really occurs with hyperbaric hyperoxia
Respiratory effects
- Direct oxygen toxicity - mucositis, tracheobronchitis
- Haldane effect - increased PaCO2
- Impaired hypoxic pulmonary vasoconstriction - increased PaCO2
- Absorption atelectasis - no nitrogen to hold the airways open
- Absorption atelectasis can also encourage post operative respiratory infections
- The oxidative damage is likely to worsen any pre-existing disease
- Hyperoxia makes a post-operative patient with a PCA more likely to have respiratory suppression
- Hyperoxia reduces pulmonary vascular resistance in the short term*
*This is good for the acutely hypoxic patient with a low V/Q ratio as it improves gas exchange in perfused but not well ventilated areas.
Cardiovascular effects
- Systemic and coronary vasoconstriction
- Reduced skeletal muscle blood flow during exercise
- Hypoxia increases systemic vascular resistance and impairs coronary blood flow
- The resultant increased afterload, reduced coronary perfusion and reduced preload all lead to a drop in cardiac output
- It also messes with their carotid bodies, and their blood pressure ends up swinging all over the place, particularly if it was high to start with
Haematological
- Impaired RBC production
- Immunosuppression
So what's the highest safe dose?
We don't know, but we do know that early space craft used hypobaric pure oxygen, giving a PaO2 of around 35kPa for several days without any issue.
Interestingly the fact that we can't produce our own vitamin C means we've had to develop other enzymatic antioxidant processes, and as a result humans are pretty good at tolerating high partial pressures of oxygen when compared to other species.
What is the treatment of pulmonary oxygen toxicity?
I'm afraid we're going to have to disappoint you somewhat here.
- Pretty much just supportive care
- Assisted ventilation (which can make things worse)
The most important bit is ruling out other causes of lung injury that you can actually treat.
Sometimes it's helpful
As with many things in medicine, there is the odd occasion when bad becomes good and we can actually use something harmful as a useful therapeutic intervention (as long as it's done properly).
Some examples of hyperoxia as a therapy
- Hypoxia - obviously, but the aim is to achieve normoxia ASAP
- Carbon monoxide poisoning - to displace high affinity CO from Hb
- Pneumothorax - denitrogenates lungs and aims to shrink pneumothorax
- Cluster headache - 12 litres per minute improves symptoms
- Decompression sickness - hyperbaric hyperoxia
Completely useless fact
- Assuming a patient has an oxygen consumption of 200ml per minute
- And a cardiac output of 5 litres per minute
- You need 5ml of oxygen in 100ml of blood
- With no haemoglobin, and just saline, Henry's law says you'd need around 2200 kPa of oxygen to get 5ml to dissolve per 100ml
- So with 100% oxygen in a hyperbaric chamber at 22 atmospheres
- You could theoretically keep someone alive with no blood
Theoretically.
Why is the surgeon telling me to give more oxygen?
So some early evidence suggested that an FiO2 of 80% reduced postoperative nausea and vomiting, but this has subsequently been shown to not be a thing.
Apparently a very small subset of patients, who'd had a gas induction and no other antiemetics found a bit of benefit, but that's it.
Certainly not worth all the damage it does.
Some others thought that lots of oxygen helped reduce wound infections, and this chain of thought even reached the point where the WHO in 2016 advised that every intubated patient having surgery should be treated with hyperoxia, and we should all ignore the adverse effects of the oxygen.
Our issue with this point
Okay, so let's entertain the idea that increasing oxygen delivery to the wound improves its healing - it's a logical suggestion after all.
But there are many factors that affect oxygen delivery to the wound:
- The surgery itself, and what vessels they've slashed in the process
- Hypothermia
- Oedema
- Hypovolaemia
- Anaemia
- Pain and sympathetic drive
- Cardiac output
If any of these are preventing adequate perfusion of the wound, then just throwing more oxygen into the blood isn't going to do anything helpful.
Plus, we know that you end up getting a paradoxical reduction of DO2 with hyperoxia anyway!
Rant over.
As you can imagine this has been widely criticised, and more recent studies disagree vehemently with this conclusion.
The only thing that maybe benefits from hyperoxia is anastomotic integrity, with some evidence suggesting fewer cases of dehiscence and breakdown in patients given more oxygen, but it's not solid evidence and you really want to consider whether it's worth all the potential harm.
A vascular surgeon might ask you to give lots of oxygen to a patient with chronic diabetic foot ulcers to try and reduce the risk of amputation, but with all the harmful side effects and the lack of power in these studies - probably best not.
Interestingly, cancer patients seem to survive better (at 3 years) if given 30% oxygen compared to 80%, suggesting the oxygen might have an impact on seeding of metastatic cells.
How can accidental hyperoxia be avoided?
- Prescribe oxygen properly
- Titrate to a saturations target
- Check whether they're a CO2 retainer
- By all means use 15 litres via a non rebreathe mask for resuscitation, but as soon as possible, wean oxygen supply down to hit target saturations of 92-94%
What about ICU?
Yeah there are no surprises here either - avoid hyperoxia wherever possible.
Essentially, unless there are extenuating circumstances or a very weird and wonderful pathology that requires a specific oxygen target - you should aim for oxygen levels of 94-96% or 9-13 kPa.
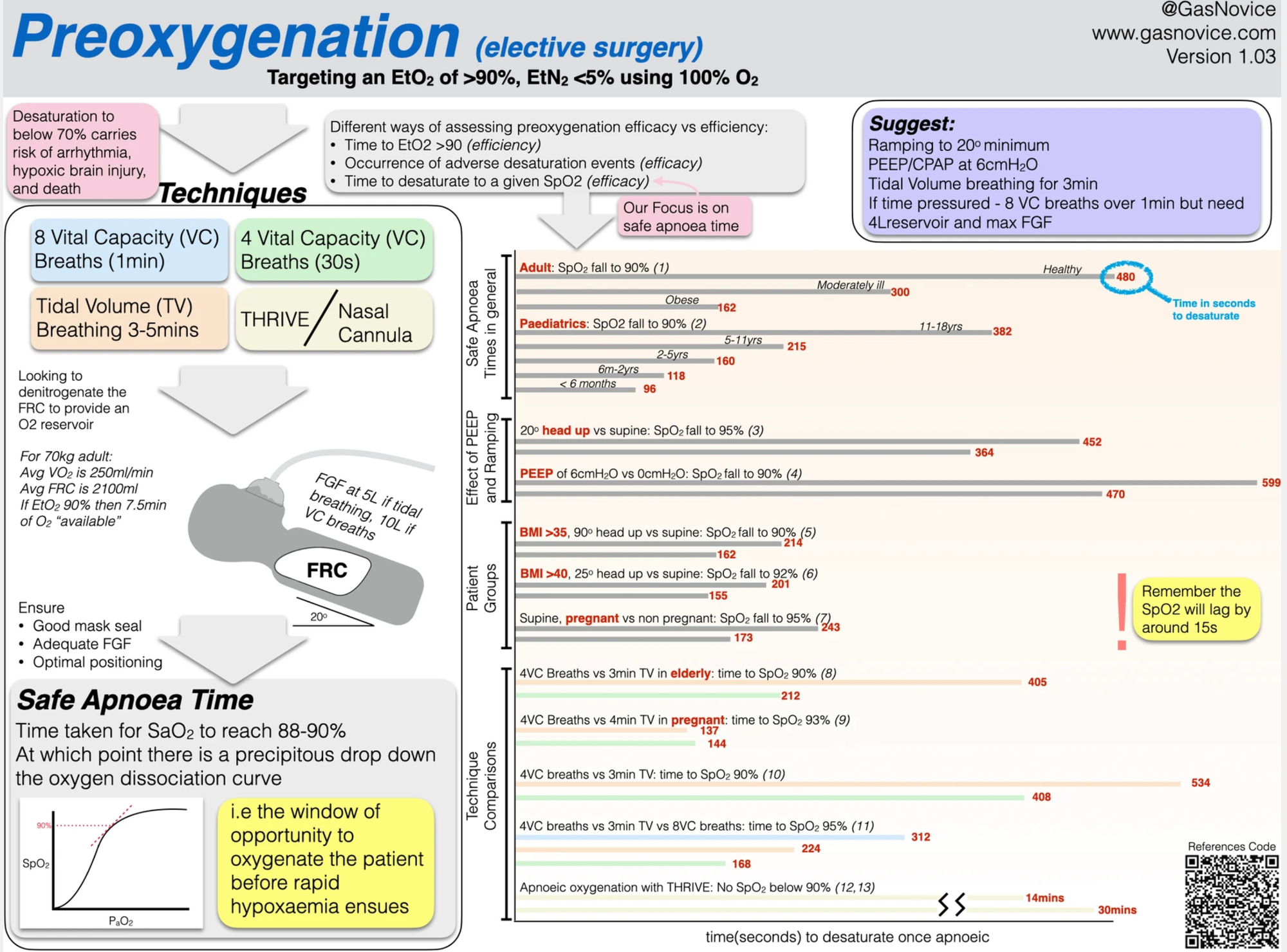
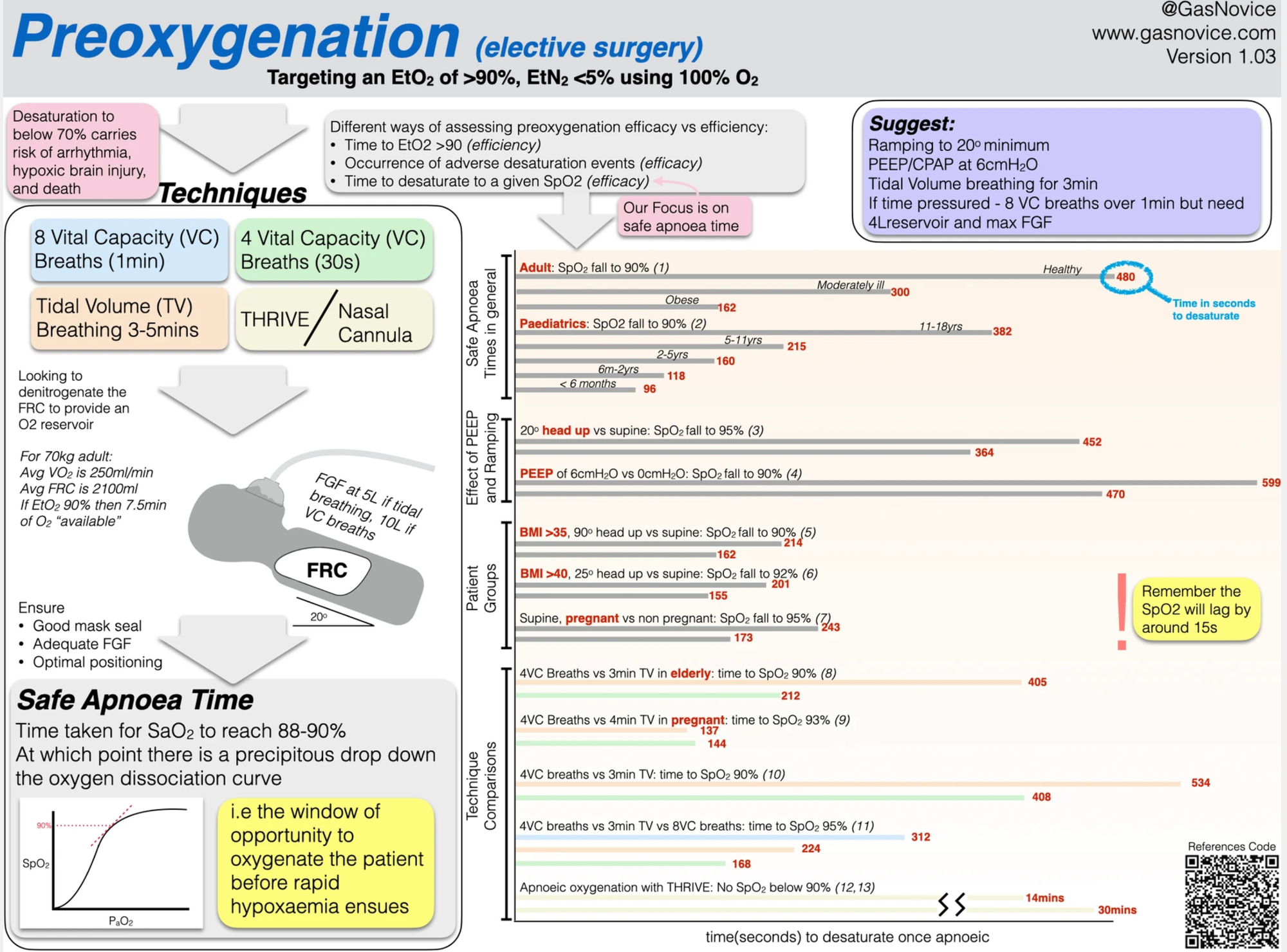
I can still preoxygenate though right?
YES.
Using 100% (or 95% if you're one of them) to denitrogenate the lungs before high risk airway interventions such as intubation and extubation remains crucially important, and the benefits of having an FRC full of oxygen massively outweigh any potential harms of a few minutes of hyperoxia.
This is largely because you're doing it for a matter of minutes rather than hours, and 100% oxygen is considered safe if you're giving it for less than a few hours.
Check out this brilliant infographic from Novice Anaesthesia
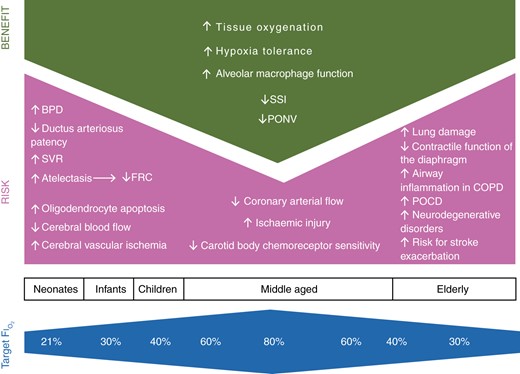
Kids too?
Maybe not...
The infant respiratory system is a tricky pickle.
They have very compliant chests and very bouncy lungs, meaning there's an increased tendency for their airways to collapse, so their apnoeic FRC's are even more tiny than you'd expect.
This means they don't benefit nearly as much as adults from solid preoxygenation prior to induction of anaesthesia.
Because they collapse their airways with such enthusiasm, they're much more reliant on effective V/Q matching, and much more sensitive to atelectasis, both of which are made worse by lots of oxygen.
A word to the wisened
There are some key things to be aware of in elderly patients.
Older lungs produce more free radicals and express more pro-inflammatory cytokines, and develop permanent fibrotic damage sooner than younger lungs.
Older skeletal muscle deteriorates due to myofibril damage over time, and this process is worsened by hyperoxia - the diaphragm is no exception to this rule, so they suffer worse diaphragmatic contractile dysfunction.
And then there's the brain.
This is particularly important in elderly patients who already have an impaired NO-mediated cerebral vasodilatation response, and reduced cerebral blood flow to begin with.
So their finger sats can be great, but their cerebral sats not so much.
There are also suggestive studies that link hyperoxia with worsening and even development of Alzheimer's and other neurodegenerative disorders.
Oxygen and COPD
We've covered this here, but in summary:
- Lots of oxygen impairs hypoxic pulmonary vasoconstriction
- Lots of oxygen also messes with the Haldane effect
- Lots of oxygen also reduces hypoxic drive (but this isn't as important as the other two)
As a result, too much oxygen in patients known to retain CO2 results in rapidly worsening hypercapnoea, narcosis and respiratory failure.
Useful Tweets and Resources
🔐"Hyperoxia in all intubated surgical patients to prevent surgical site infections is not supported by convincing evidence. Accumulating evidence suggests a dose- and time-dependent relationship between hyperoxia and significant complications."
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 (@Anaes_Journal) September 23, 2020
🔗https://t.co/RWkySGOtqB pic.twitter.com/GwaAueMcA0
Today's Paper of the Day is by Mervyn Singer on the dnagers of hyperoxiahttps://t.co/JKgcYjlUQ5
— Critical Care Reviews (@CritCareReviews) July 3, 2023
Join us to read 1 paper per day and stay up-to-date as we cover the spectrum of critical care across 2023 pic.twitter.com/RYDfbE3iBC
Check out this awesome infographic on pre-oxygenation from Novice Anaesthesia
References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
