Lambert-Eaton Myasthenic Syndrome
This is a quick-fire revision post aimed at the Final SOE exam, but it can come up in the Primary too.
The classic history you're going to get in the exam, particularly the Final SOE, is of an elderly patient with suspected lung cancer, who has weird neurological symptoms as well - in particular proximal weakness.
Definition
- A rare autoimmune neuromuscular disorder
- Affecting the neuromuscular junction
- Usually associated with malignancy
Clinical features
- Proximal limb weakness
- Can also have bulbar and ocular symptoms, but less common
- Weakness improves with repeated activity (opposite of myasthenia)
- Lambert's sign = improved power with repeated hand grip
- Deep tendon reflexes are often reduced or absent.
There's often autonomic involvement too:
- Dry eyes
- Dry mouth
- Constipation
- Blurred vision
- Slow gastric transit
- Postural hypotension
Explain the pathophysiology of Eaton-Lambert Syndrome
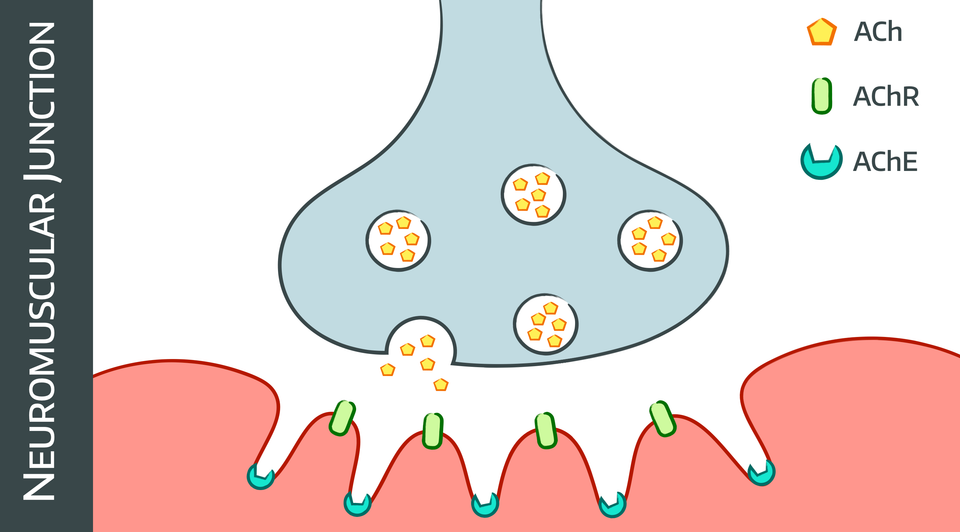
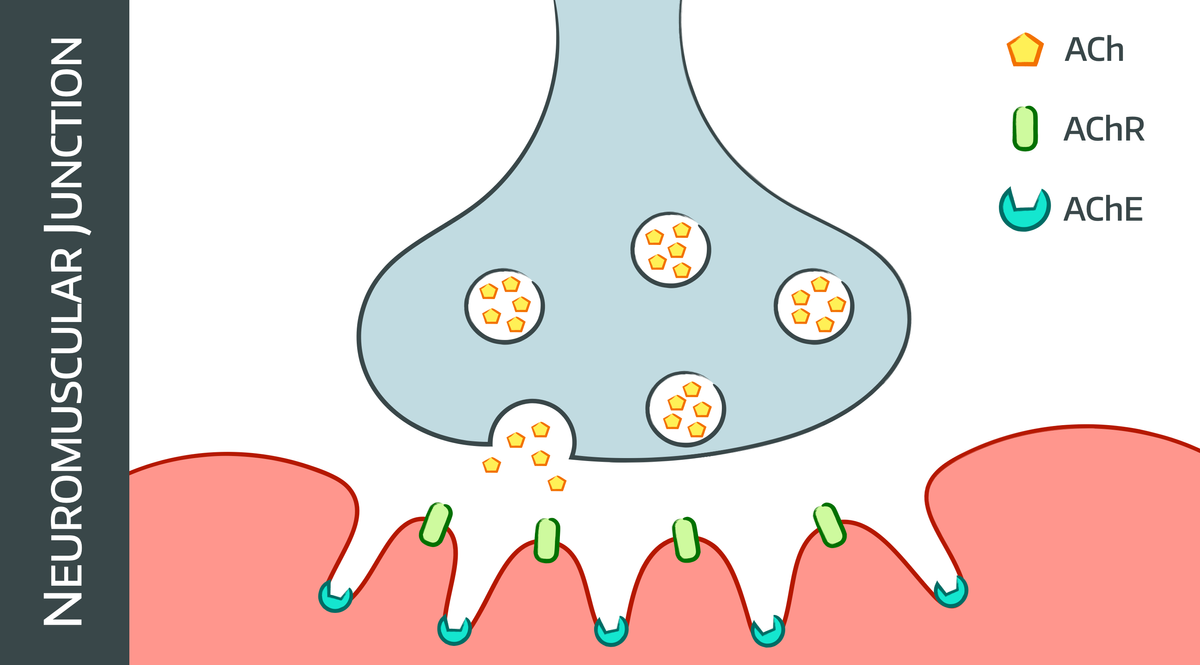
- IgG antibodies agains the pre-synaptic voltage gated calcium channels at the neuromuscular junction*
- Reduces calcium entry with each action potential
- This means less acetylcholine is released with each action potential
- This causes reduced muscle activity and weakness
- Repeated stimulation allows more calcium in, and increases force of contraction
*Meanwhile in MG, autoantibodies are raised against either the acetylcholine receptor itself or muscle specific kinase
What are the treatment options?
- Supportive management - ABC as per any disease ever
- 3,4-diaminopyridine (amifampridine) enhances ACh release by prolonging depolarisation
- Pyridostigmine (AChE inhibitor) not as useful as in myasthenia gravis
How does Eaton-Lambert differ from Myasthenia Gravis?
Eaton-Lambert
- Proximal limbs
- Power improves with repeated action
- Most patients have autonomic symptoms
Myasthenia Gravis
- Usually eyes and face affected
- Commonly bulbar as well
- Fatiguable weakness, worsens with repeated action
- Generally no autonomic involvement
Which malignancies are classically associated with Eaton-Lambert syndrome?
- Small cell lung carcinoma
Rare:
- Non-small cell lung cancer
- Thymoma (malignant)
- Breast
- Gallbladder
- Prostate
- Bladder
- Stomach
How does Eaton-Lambert syndrome affect your anaesthetic plan?
- Delayed gastric emptying - high aspiration risk, use RSI
- Autonomic instability - cardiovascular support, arterial line
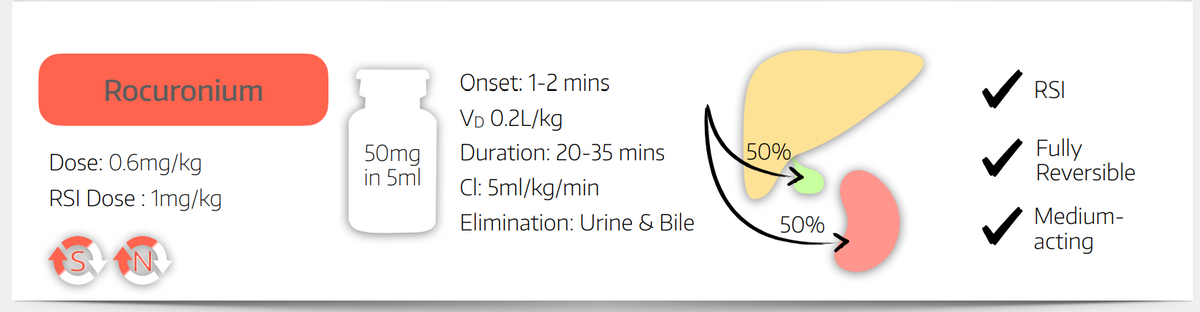
- Sensitivity to both depolarising and non-depolarising neuromuscular blocking agents - reduce dose significantly, neostigmine is safe to use
- Weakness - may need post op ventilation
References and Further Reading


Here's a relevant RCOA example video
More Anaestheasier articles
Myasthenia Gravis
and Lambert-Eaton syndrome
Muscle Relaxants
Take home messages * If in doubt, rocuronium is rarely a bad idea * Avoid suxamethonium in malignant hyperthermia, burns and spinal cord injury (conditions apply) * Make sure your patient is adequately anaesthetised Why paralyse a patient? It sounds terrifying, and we’d strongly advise not using the word ‘paralyse’ around your patient,