Awake Craniotomy
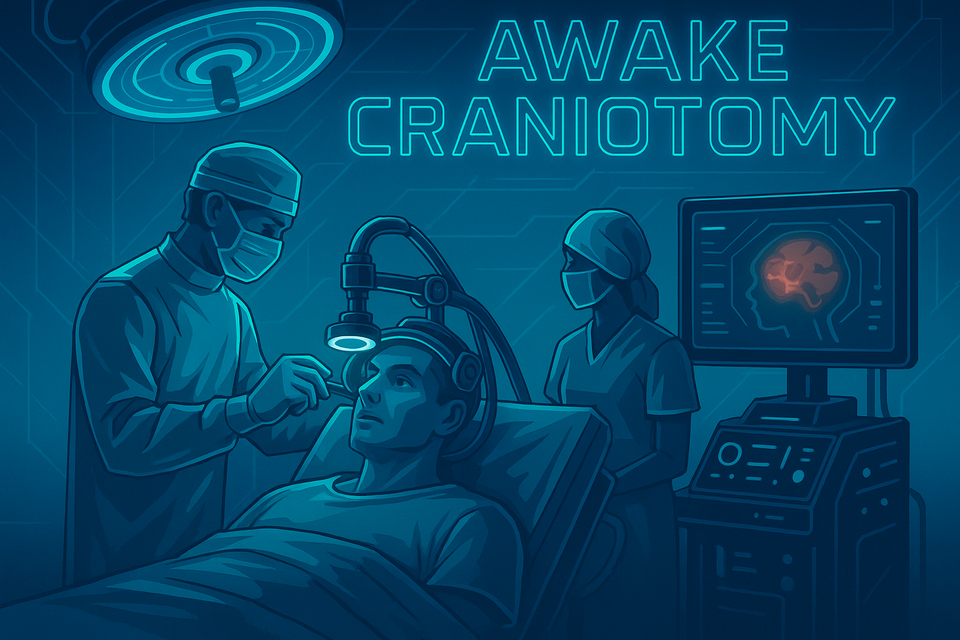
Take home messages
- Awake craniotomy allows real-time assessment of eloquent cortex during high risk resections
- Get good at scalp blocks
- Ensure there's a big bucket of ice cold saline available
A spot of history
Over seven thousand years ago, we decided that it would be a simply splendid idea to drill holes in the heads of the afflicted, in order to release 'evil air' in a process known as trepanning.
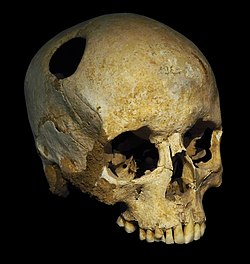
They must have really believed it worked, because they were doing it all the way from France to Peru.

Given there was no general anaesthesia available at the time, this would have technically counted as an awake craniotomy.
Then in 1886 Sir Victor Horsley did brain surgery for epilepsy properly for the first time.
Under general anaesthesia (chloroform since you ask) he excised a post-traumatic cortical scar that was acting as an epileptic focus in a twenty-three year old man.
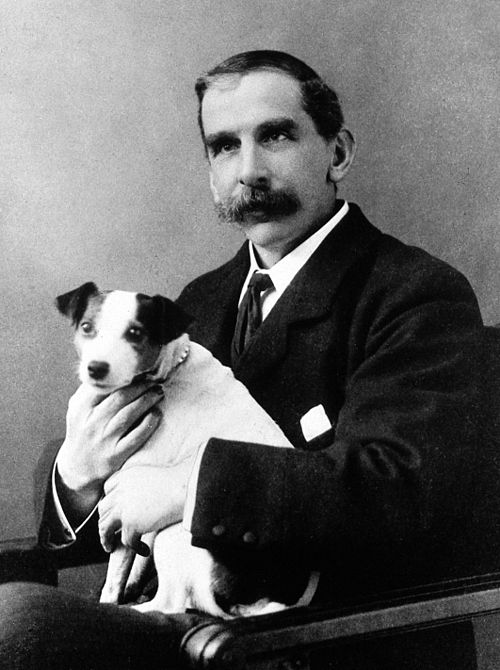
Horsley was the first ever neurosurgeon appointed to the National Hospital for Neurology and Neurosurgery in Queen Square, and hence the department is named in his honour.
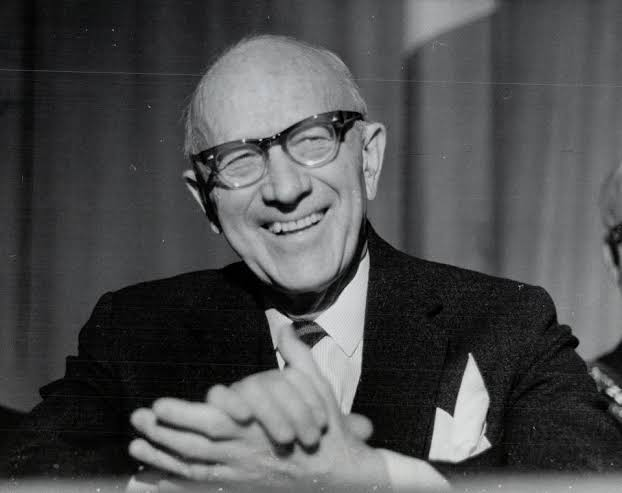
It took until the 1930s, however for Wilder Penfield to do the first awake craniotomy with cortical mapping, using a combination of local anaesthesia and light sedation.
Remind me why we're doing this?
Aside from the fact it makes for awesome YouTube videos:
There are also genuine medical reasons as to why we do major brain surgery with the patient awake.
Advantages of awake craniotomy:
- Maximises amount of tumour resected without damaging neurological function
- Less nausea and vomiting
- Quicker recovery
- Patients seem to prefer it and report less pain
Indications
You don't do awake brain surgery for every neurosurgical procedure, just the ones where you really want to know that the delicate nearby cortex is still doing its job.
- Resection of tumours next to eloquent cortex (speech, sensory, motor, cognition)
- Deep brain stimulation - Parkinson's and dystonias
- Epilepsy surgery requiring electrocorticography
- Resection of vascular lesions (AVMs and mycotic aneurysms) right next to important areas
- Stereotactic brain biopsy
As fMRI gets better, we might be needing to do less intra-operative awake mapping in future, but for now, it's still very useful.
Who can't have it?
My common senses are tingling - anyone who really doesn't want it, or isn't going to sit still safely.
Your surgeon - rather reasonably - wants a perfectly still surgical field, so the patient is going to have their head in some sort of clamp (usually a Mayfield clamp).
Therefore they ideally need to not be moving the rest of their body (consciously or as a result of seizure activity).
Contraindications
Absolute
- Patient refusal
- Inability to remain still
- Prone positioning* (low occipital tumours)
Relative
- Obesity class III
- Sleep apnoea
- Poorly controlled seizures
- Anxiety
- Difficult airway
Lots of dural resection can be extremely painful, and so may represent a contraindication in certain cases.
*Patients will usually only tolerate supine or slightly sat up.
How to do it
There are three different techniques at your disposal that you need to be able to blurt out in the exam:
- Awake
- Asleep - awake
- Asleep - awake - asleep
That's it.
Oh, and a scalp block - see below.
Depending on the operation, the surgeon, the anaesthetist and the patient, you can either keep the patient awake throughout, or have them asleep for the bits where they don't need to be awake and following instructions.
Awake
- You need a really good scalp block
- You need a really motivated patient
You can also employ a smidge of light sedation.
Asleep-awake
- General anaesthetic, usually with TIVA for a smooth wake up
- Wake up for mapping or functional assessment
- Consider some sedation for closure
Avoids need for airway manipulation in a Mayfield frame.
Asleep-awake-asleep
- General anaesthetic, usually with TIVA for a smooth wake up
- Wake them up for mapping or functional assessment
- Off to sleep again for closure
Requires airway manipulation while in a Mayfield frame.
Second generation LMAs are preferred for the usual reasons:
- Less stimulating and risky than trying to intubate
- Better airway protection and ventilation than standard LMA
What do anaesthetists choose?
Hey guess what, no surprises here - it's a fairly even split
35% asleep–awake–asleep
30% awake
As always - it's about doing your anaesthetic really well, rather than using the 'best' technique.
And whichever one you do end up using, you're going to need a scalp block too.
Pre-op concerns
Much of the pre-operative preparation is in selecting the right patient and ensuring they are psychologically prepared for what to expect.
- Visit to theatre to see the environment as a dress rehearsal for the big day
- Neuropsychologist input to establish baseline function, particularly language
- Decide whether day case surgery is feasible or appropriate
Monitoring
All the usuals here (AoA minimum standard monitoring) plus:
- Capnography
- BIS or equivalent if asleep
- Invasive arterial line
- Big cannula
- Neuropsychologist (or neurophysiologist)
- Temperature
Extra bits for the awake patient:
- Minimise noise
- Keep the patient positioned comfortably
- Maintain a sensible temperature
- Ensure the patient can see and communicate with the team - no drapes over face, or clear drapes if needed
Scalp block
Whatever technique you decide to employ with regards to sleepiness, you're almost always using a scalp block as well.
In some elderly patients who are high risk for GA or sedation, you can often get away with just a scalp block if it's done well.
The seven magnificent nerves and where to find them
- Supraorbital - supraorbital notch, top of the eyebrow
- Supratrochlear - 1cm medial to the supraorbital nerve
- Zygomaticotemporal - half way between tragus and orbit
- Auriculotemporal - 1cm anterior to tragus
- Great auricular - mastoid process
- Greater and Lesser occipitals - 1/3 and 2/3 of the way from occiput to mastoid
The surgeon may also need to infiltrate local anaesthetic to the dura, as this is also highly sensitive.
Can I sedate them?
Well of course you can, provided they're not required to be completely compus mentus to demonstrate the ongoing integrity of their valuable eloquent cortex.
Again, as with all anaesthesia ever, the techniques used will vary depending on the hospital, the patient, the anaesthetist and the surgeon.
Options include:
- Propofol and remifentanil TCI remains very popular in the UK
- Dexmedetomidine is increasingly used for its sedation and analgesic properties without significant respiratory depression - 0.2 - 0.7 mcg/kg/hour
- Clonidine
- Benzodiazepines
- Fentanyl
The benefits of short-acting, titratable agents are enormous here, as it allows sedation for the distressing noisy bits, and then a rapidly awake patient for the talk-y move-y bits.
Remember lots of antiemetics as well - having your brain tugged about is rather nauseating, especially the temporal lobe.
What could go wrong?
An awake patient, with a brain tumour, head clamped à la Mayfield, and a surgeon holding a drill.
I can't forsee any problems at all.
Complications of awake craniotomy
Airway and Breathing
- Airway obstruction
- Hypoxia
- Hypercapnoea - causes 'tight brain'
- Aspiration
- Conversion to GA
Cardiovascular
- Hypotension
- Hypertension
- Arrhythmia
- Local anaesthetic toxicity
Neuro
- Pain
- Over/undersedation
- Venous air embolism*
- Seizures - focal or generalised**
- Brain swelling
- Local anaesthetic toxicity
- Nausea and vomiting
- Failure of procedure
Psychological
- Anxiety
- Fatigue
- Agitation
- Reversal of consent
*Venous air embolism is a higher risk when oversedated and hypovolaemic, especially if there is significant negative intrathoracic pressure and the patient is sat up.
**The best treatment for intraoperative seizures is to pour ice cold saline over the brain.
#brainfreeze
Post operative concerns
Unsurprisingly a patient who has just had their head temporarily hard-boiled-egged requires rather close monitoring afterwards, preferably on a dedicated high dependency unit.
- Neuro obs for 6 hours post op
- Post op imaging
- Day case awake craniotomy is possible in the right patient with the right support
Useful Tweets and Resources
Very basic steps of cracking open the skull aka craniotomy. pic.twitter.com/uS5w1VQUDf
— Oren Gottfried, MD (@OGdukeneurosurg) January 24, 2023
1/3
— Scientissimum (@scientissimum) January 4, 2023
Good morning #medtwitter! Today #scientissimum would like to show you a neurosurgical emergency case of decompressive hemicraniectomy by Scientissimum’s own Dr. Yashar. Decompressive craniectomy is a neurosurgical procedure in which part 🧠#neuro #neurosurgery #wednesday pic.twitter.com/RteX0LvBIL
Second Awake craniotomy this month already.
— Pratyusha (@AnotherParadox0) February 9, 2024
Wasn't so sure of using Dexmedetomidine initially with baseline pulse of my pt being 56-58/min.Got great results with combined Effects of sedation, counselling and scalp nerve block however. pic.twitter.com/dL6vto4M9Y
Here's another good one, but you have to watch on YouTube as it's age restricted.
References and Further Reading


Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
Anaestheasier® is a registered trademark.

