Arterial Lines
Take home messages
- Arterial lines are super useful and relatively simple to insert
- You need to understand how to interpret the waveform and troubleshoot it when it doesn't work
- If in doubt, check with a non-invasive blood pressure
My favourite bit of kit.
I adore an arterial line, and require only the loosest indication to justify putting one in.
They're fabulous.
Not only can you monitor the patient's blood pressure from beat to beat without tourniqueting their arm to death, you can take repeated arterial blood gas measurements on demand.
What's not to love?
A spot of history
All the way back in 1733, when one could feasibly be a clergyman, botanist and pneumatic chemist all at the same time, a chap by the name of Hales planted 'fine tubes' straight into the arteries of some rather unfortunate mammals, in order to see how high the column of blood would climb, thereby measuring the 'force' of the heart.
He also let them slowly exsanguinate in the name of science, measuring their blood pressures as they succumbed.
"the Mare fell into cold and clammy sweats"
It wasn't until 1896, however, before we saw the first sphygmomanometer, devised (or at least credited to) Italian doctor Riva Rocci.
Then in 1905, along came Nicolai Korotkoff with his magical sounds.
Nowadays, invasive arterial blood pressure measurement is considered to be the gold standard, and for good reason.
It's awesome.
Indications for invasive blood pressure monitoring
Any time when you're expecting significant and rapid changes in blood pressure, such as:
- Cardiovascular instability
- Vasopressor/inotrope use
- Fluid management
- Critical illness on intensive care (to avoid continuous cuff inflation and potential limb damage)
- Any time repeated blood gas analysis is indicated, such as DKA
Also when NIBP is unlikely to be accurate, such as:
- Obesity
- Non-pulsatile blood flow (cardiac bypass/ECMO)
- Arrhythmias
Just note that with invasive measurement, the systolic value is usually slightly higher, and the diastolic slightly lower, than NIBP, however the mean arterial pressures are the same.
You can gather a lot of information from that trace
Aside from being a pretty little red line to watch gently bouncing across the screen, it's actually rather useful for a surprisingly large amount of data.
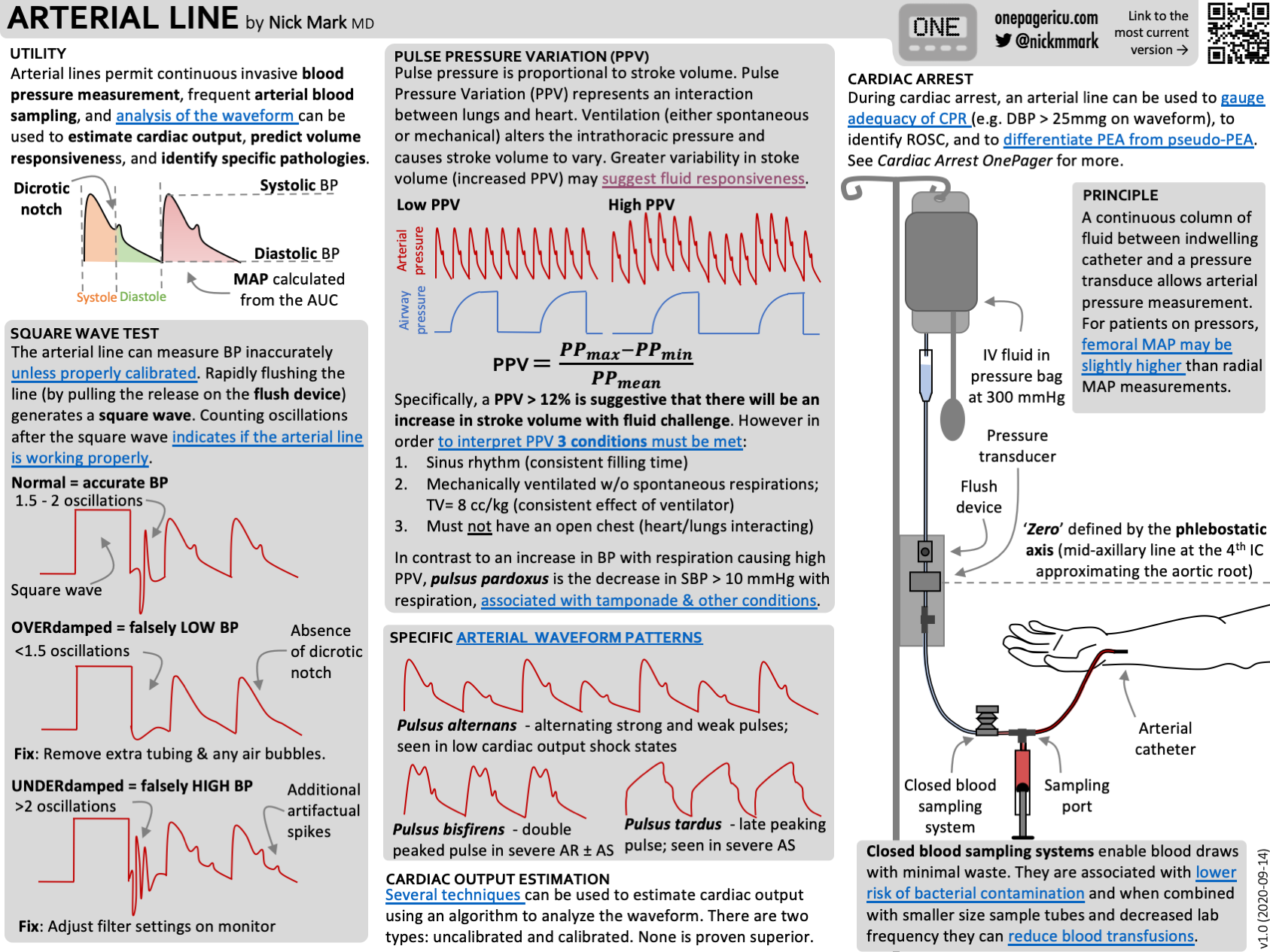
Information in the waveform
- Heart rate
- Systolic pressure
- Diastolic pressure
- Mean arterial pressure
- Pulse pressure and pulse pressure variability
- Gradient of anacrotic limb - important in aortic stenosis
- Systemic vascular resistance - position of dicrotic notch
- Also how well your arterial line is working, obviously
The wave itself
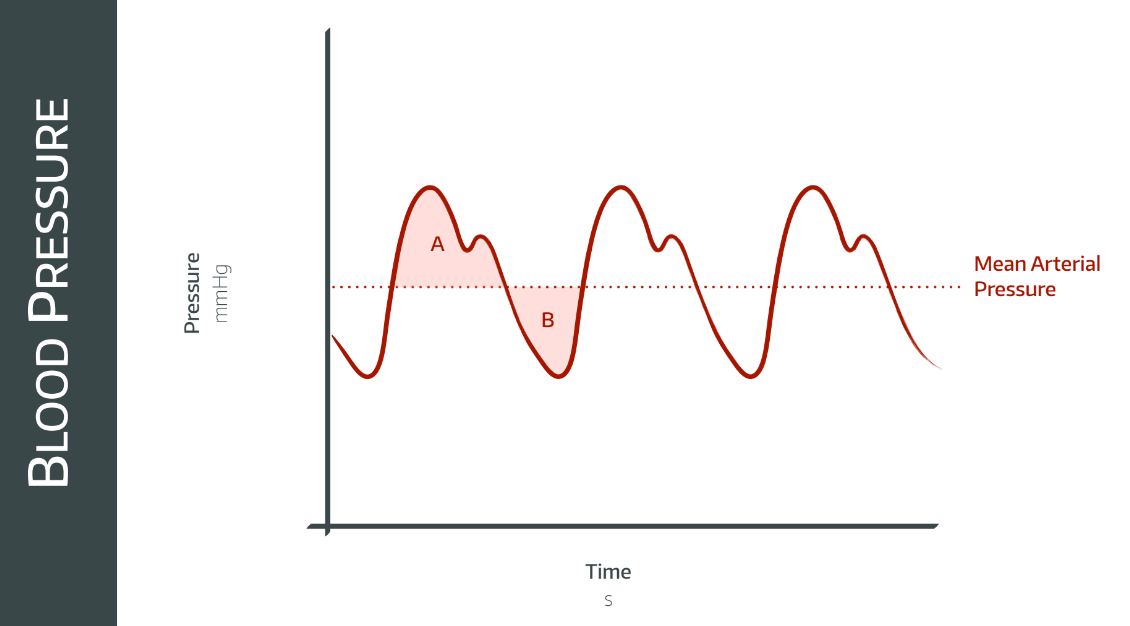
The arterial waveform has three basic components:
- The systolic phase - from aortic valve opening to left ventricular emptying
- The dicrotic notch - closure of the aortic valve*
- The diastolic phase - From aortic valve closure, through diastole, until the next beat
*Technically, the dicrotic notch is distinct from the incisura. The incisura is the sudden uptick in pressure seen in the aorta when the valve closes. The dicrotic notch, meanwhile, is seen more in the distal vasculature, and is a combination of reflected waves bouncing off the peripheral blood vessels and is only loosely related to the aortic valve.
The highest point on the waveform is the systolic peak pressure, and the lowest point is the diastolic pressure.
The mean arterial pressure (MAP) is calculated from the area under the curve.
The diastolic pressure is important, because this is when the coronary arteries are perfused, so don't ignore it!
How does one do them?
To be fair it only gets marginally more technical than 'clean the skin and put a line in the artery rather than a vein'.
Ideally use an artery that has a collateral (e.g. radial artery) that can supply the distal tissues in case your arterial line causes damage or thrombosis:
There are two types of arterial line:
- Cannula style

- Seldinger style
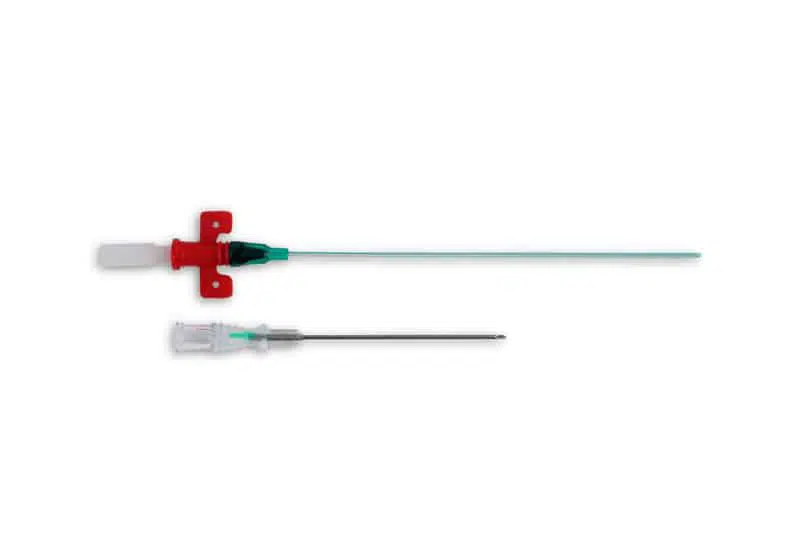

In the same way that iPhone and Android users will stubbornly refuse to accept that the other is pretty much equally as good, there are those anaesthetists who will insist that the Flowswitch is superior, and there are those that insist the Leadercath is better (who are wrong).
- If you're putting a Flowswitch into the radial artery, you can pretty much treat it like a cannula, and use strict aseptic non-touch technique
- If you 're putting a Seldinger (Leadercath or PiCCO) line in, using an endovascular guidewire, you should use full-on sterile technique as you would for a central line
Blind vs Ultrasound
It's hard to justify doing anything without ultrasound these days, but you can put arterial lines in using a 'landmark' technique - palpating the pulse and aiming straight at it - but most people usually like to whip out the magic eyes and do it properly.
In plane vs out of plane:
- It doesn't matter really, it's more important to use what you're skilled with
- The gold standard is probably both - switching between the two to be doubly-sure you're in the right place
Check out these two tweets for a perfect demonstration:
I love to toggle to see in both planes. My goal is avoid the vessel for hyper selective blocks pic.twitter.com/lM2d76UwLa
— Paul Winston MD - Restoring Movement is the goal. (@drpaulwinston) May 27, 2023
How do they work?
Fluid isn't compressible, generally speaking, so if you have a continuous column of fluid in a reasonably stiff tube, then if you apply pressure at one end, this will be conducted along the column to the other end.
Your arterial line and the stiff transducer tubing set connect the blood in the artery to your transducer, which then converts the mechanical pressure signal into an electrical signal, and sends it to the computer for filtering, amplification and display on the monitor.
To do this it uses a strain gauge - a length of wire whose electrical resistance increases when stretched. Simply attach this to a diaphragm that the column of fluid pushes against, and you have a direct mechanical-force-to-electrical-energy conversion.
This electrical signal is tiny however, so it needs amplification, which historically has been via a Wheatstone Bridge (OSCE FODDER!).
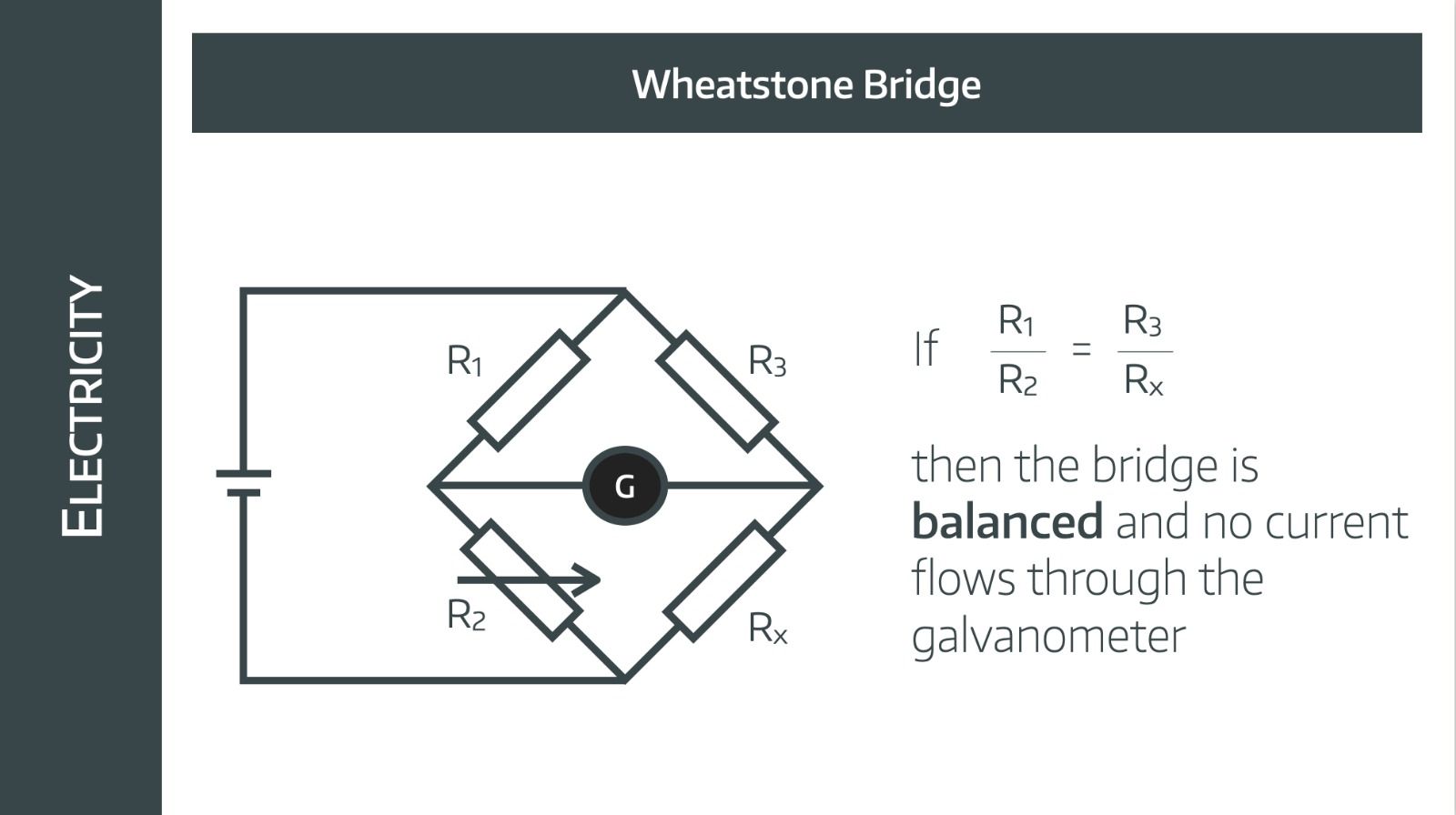
How does a Wheatstone bridge work?
- The Wheatstone bridge has a DC supply to two parallel circuits each with two known resistors
- One of the circuits also has a variable resistor, and the other has the unknown resistance to be tested (in this case the strain gauge)
- A voltmeter or galvanometer between the two parallel circuits very sensitively and accurately detects any difference between the sum total resistances between the two circuits
- As the arterial blood pressure moves the diaphragm and changes the resistance of the strain gauge, it changes the voltage across the voltmeter, and this is then amplified and plotted as a waveform on the monitor after Fourier analysis
Which leads us nicely to another classic Primary FRCA OSCE question:
What are the features of an ideal arterial line?
- Stiff
- Short
- Wide bore
- Non-tapered
- Non-thrombogenic
- Cheap and easy to manufacture
Remember you need to use 0.9% Sodium Chloride for the transducer fluid, not Dextrose - otherwise you'll start giving insulin for spuriously high blood sugars on the blood gas measurements and the patient won't thank you.
Where to put the transducer
Level with the right atrium.
The clue is in the unit - millimetres of mercury. The pressure in a column of fluid is related to its height, so if the transducer is at a different height to the heart, this difference in height will cause the column of fluid in the tubing to exert its own pressure on the transducer membrane.
So if there's a systolic of 220mmHg on the monitor, just check the transducer isn't on the floor.
Damping and Resonance
Two physics concepts that are useful to understand, both for exams and for troubleshooting, are damping and resonance.
Damping
This is essentially the loss of energy from the system between the source and the point of measurement:
- Kinetic energy is lost as heat to the walls of the cannula and tubing, hence they are made as short and as stiff as possible to reduce this
- It can also be due to the presence of bubbles and any occlusion of the cannula or tubing
You want some damping, because otherwise you get uncontrolled feedback ricocheting back and forth, producing an incomprehensible signal.
The right amount of damping is given by the damping factor.
- Damping factor <0.7 - An underdamped system will resonate, causing a bouncy oscillating signal with lots of overshoot
- Damping factor 0.7 - An optimally damped system will give you a nice quick response to a change in the signal, with just a little overshoot allowed, to increase the speed
- Damping factor 1.0 - A critically damped system won't have any overshoot, but takes much longer to respond, and isn't useful for rapid beat-to-beat measurement of blood pressure because the next impulse has already started before it has finished transmitting the previous one
- DF >1.0 - An overdamped system will take far too long to respond and isn't useful
To test how well damped your system is, you can do the square wave test. Pull the little toggle on the transducer to open the tap and make the screen display 300mmHg or so, then release the toggle.
The signal should 'bounce' back down to normal value with only one small period of overshoot.
Resonance
- The arterial pressure wave is a combination of sine waves each with their own frequency
- These waves all combined together form the familiar arterial trace that you see on the monitor
- Any physical system will have a specific frequency at which it will resonate - this is called the natural frequency or resonant frequency
- If the natural frequency is applied to a system, then it will resonate, forming a positive feedback loop that can spin wildly out of control, kind of like the Tacoma Bridge disaster
- Therefore our transducer, cannula and tubing are all specifically designed and manufactured to have a natural frequency higher than 40 Hz, far higher than anything that the blood pressure waveform is likely to throw at it
If you're in any doubt whatsoever during the exam, then just say the phrase 'Fourier Analysis' and everything will be okay.
Troubleshooting
Sometimes the waveform doesn't look right, or the number doesn't match your clinical suspicion, and you have to figure out if it's a patient problem or equipment problem.
Number too high
Patient problem
- Stressed or pain response
- Too light
- Vasopressor response
Equipment problem
- Transducer on the floor (or below level of heart)
- Not zeroed properly
- Under-damped
Number too low
Patient problem
- Hypotension - hypovolaemia, septic shock, anaphylaxis...
Equipment problem
- Transducer too high
- Not zeroed properly
- Severe peripheral vascular disease if peripheral artery used
Flat waveform
Patient problem
- Hypotension
Equipment problem
- Air bubble
- Clot in line
- Screen not scaled appropriately (optimise waveform)
What are the risks?
As with anything vaguely useful in medicine, it's a procedure that doesn't come without risk. Fortunately these are both relatively infrequent and generally not life threatening, but arterial lines do warrant a certain degree of respect to ensure they're done properly.
Risks of arterial lines
- Trauma to tissue
- Blood loss if disconnected
- Thrombus formation
- Infection
- Air embolism
- Infarction of distal limb
- Accidental intra-arterial injection
- Human error of overreacting to a reading that wouldn’t have been noticed with interval NIBP, such as the transducer falling onto the floor
Accidental intra-arterial injection
Can I inject stuff down it?
No.
But what if I already did?
Ah.
We'd recommend you read the anaesthesia tutorial below, but the short answer is:
- Large quantities of saline washout
- Anticoagulation, often with heparinised saline, to reduce thrombogenesis
- Early referral to plastic surgery if required
As with many incidents in anaesthesia, the best management is prevention - such as by labelling your giving set and taping over the bung on the arterial transducer so that you can't easily administer drugs via the wrong line.
New #anaesthesia tutorial published. #ATOTW 498 - Management of Accidental Intra-Arterial Injectionshttps://t.co/mMYuDD1Y3P
— WFSA (@wfsaorg) May 30, 2023
examining the aetiology, pathophysiology and management as well as considering steps which can be taken to prevent accidents from happening. #anesthesia… pic.twitter.com/MVQlZSoylA
Syllabus
- PC_BK_42 Wheatstone bridge: principles, uses
- PC_BK_51 Fourier analysis
- PC_BK_56 Transducers and strain gauges
- PC_BK_64 Pressure transducers
- PC_BK_65 Resonance, damping, frequency response
Podcast Episode
Useful Tweets and Resources
Key determinants of the arterial line tracing.
— NephroPOCUS (@NephroP) January 22, 2023
🔗 https://t.co/aI2hVtyyk9
Click ‘ALT’ for figure description #MedEd #FOAMcc #CriticalCare pic.twitter.com/x5HFokO5Ne
Low one is the radial arterial line and high one is the femoral. Patient was on huge doses of pressors which we rapidly titrated down! pic.twitter.com/kZivacJe8H
— Edward Bezant (@EBezant) June 3, 2022
Check out this great video by Dr Ken Hoffman who explains arterial lines beautifully.
References and Further Reading


Primary FRCA Toolkit
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.

