Aortic Dissection
Take home messages
- The mortality for untreated type A dissection increases by 1% per hour in the first 48 hours.
- Most commonly seen in males 50 - 70 years of age
- The tragedies of life are largely arterial - Sir William Osler
A spot of history
In 1760 this chap died rather suddenly on the toilet.

His name was King George II, and he's probably the first properly well-documented case of a fatal aortic dissection.
His personal physician Dr Frank Nicholls performed the post-mortem and found his ascending aorta had split and there was blood in the pericardium, consistent with a Type A dissection.
"… the pericardium was found distended with a quantity of coagulated blood, nearly a pint; the whole heart was so compressed as to prevent any blood contained in the veins from being forced into the auricles; therefore the ventricles were found absolutely void of blood …"
His risk factors likely included:
- Being 76 years old
- Being male
- Probably being hypertensive, what with living the life of a King and all that
- Straining on the loo
Dissection was originally included under the umbrella term of aortic aneurysm until the 1930s, after which it became recognised as its own condition.
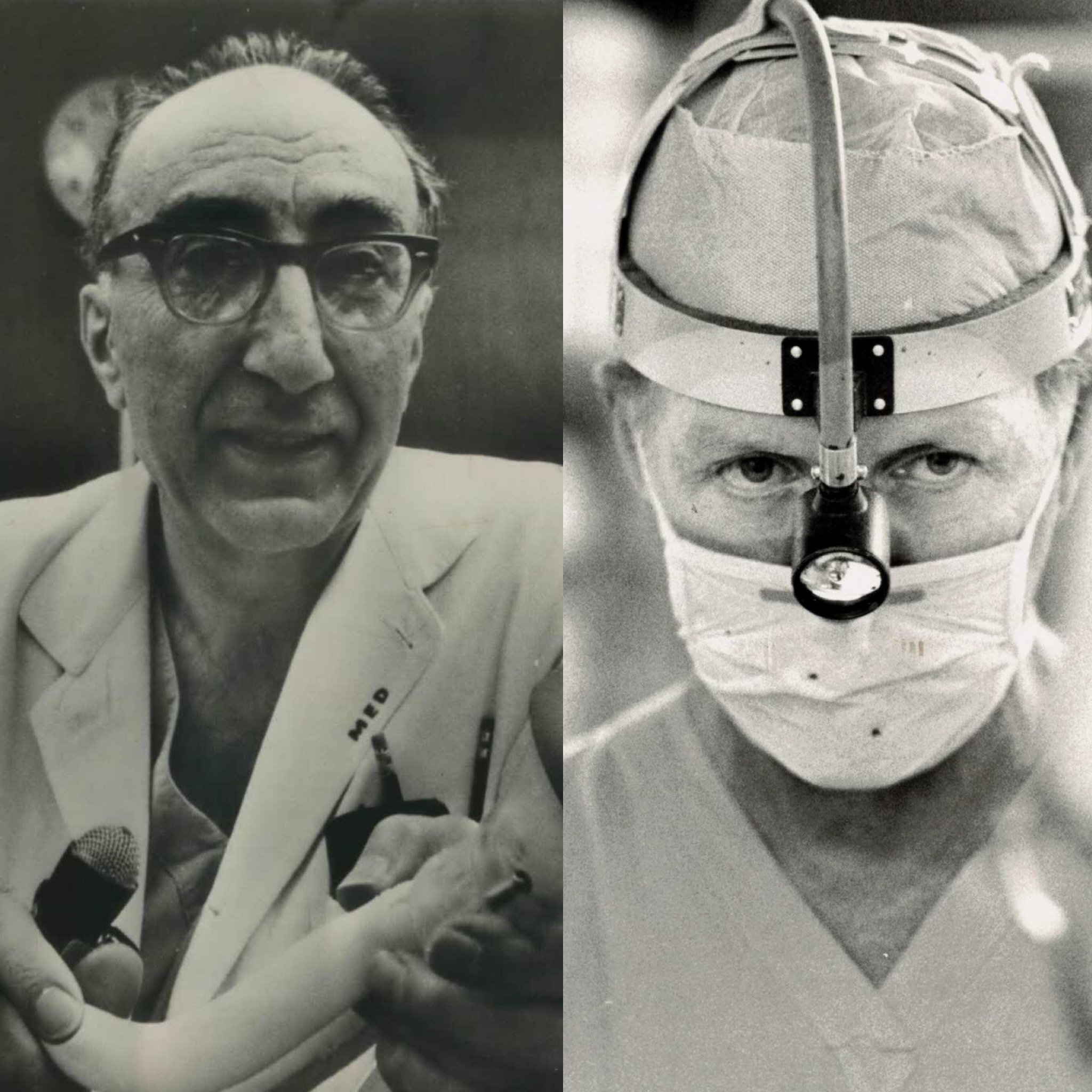
On 7th July 1954, soon-to-be rivals DeBakey and Cooley, and their colleague Creech, successfully repaired an acute ascending aortic dissection for the first time.
Drama time
DeBakey had been slaving away for years trying to build an artificial heart.
In 1969, Cooley nabbed a prototype from DeBakey's lab and popped it into a dying patient without any form of approval or DeBakey's permission.
The two subsequently fell out for decades, refusing to speak and working completely separately.
Then in 2005, DeBakey suffered an aortic dissection himself and aged 98 he became the oldest person to undergo the very operation he had pioneered.
Then in 2007 DeBakey and Cooley appeared in public together and Cooley presented DeBakey with a lifetime achievement award.
After DeBakey died in 2008, Cooley said of the legend:
“He was the greatest surgeon of the 20th century.”
It's pretty bad
Of all the bad things that can happen to our lovely patients, one of the really bad ones is when the main blood pipe stops piping and starts splitting itself apart.
This is distinctly suboptimal.
One option is for the pipe to rupture, as seen in abdominal aortic aneurysm rupture, but it's up to three times more common for this high pressure, wide bore blood vessel to dissect instead.
The mortality data for an untreated Type A dissection looks a bit like this:
- 25% in first 24 hours
- 50% in 72h
- 80% in 2 weeks
- 90% in first month
So yeah - bad.
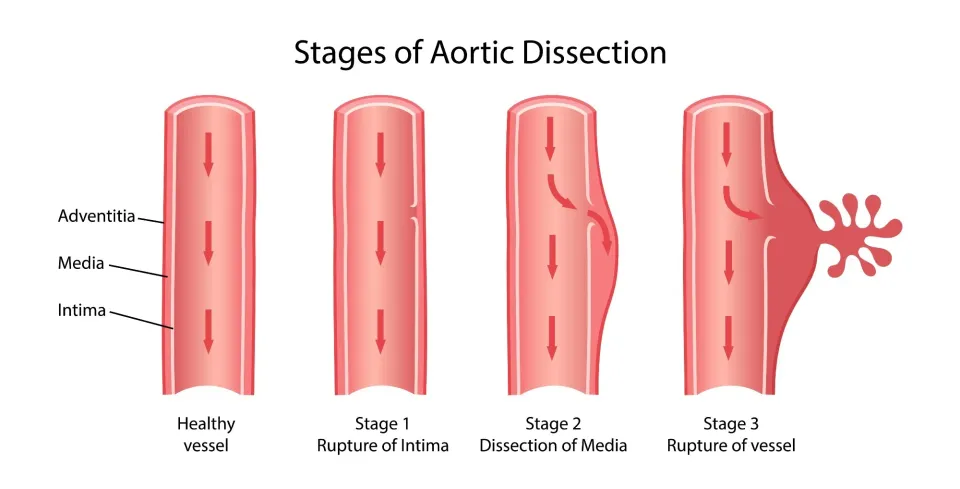
So what happens?
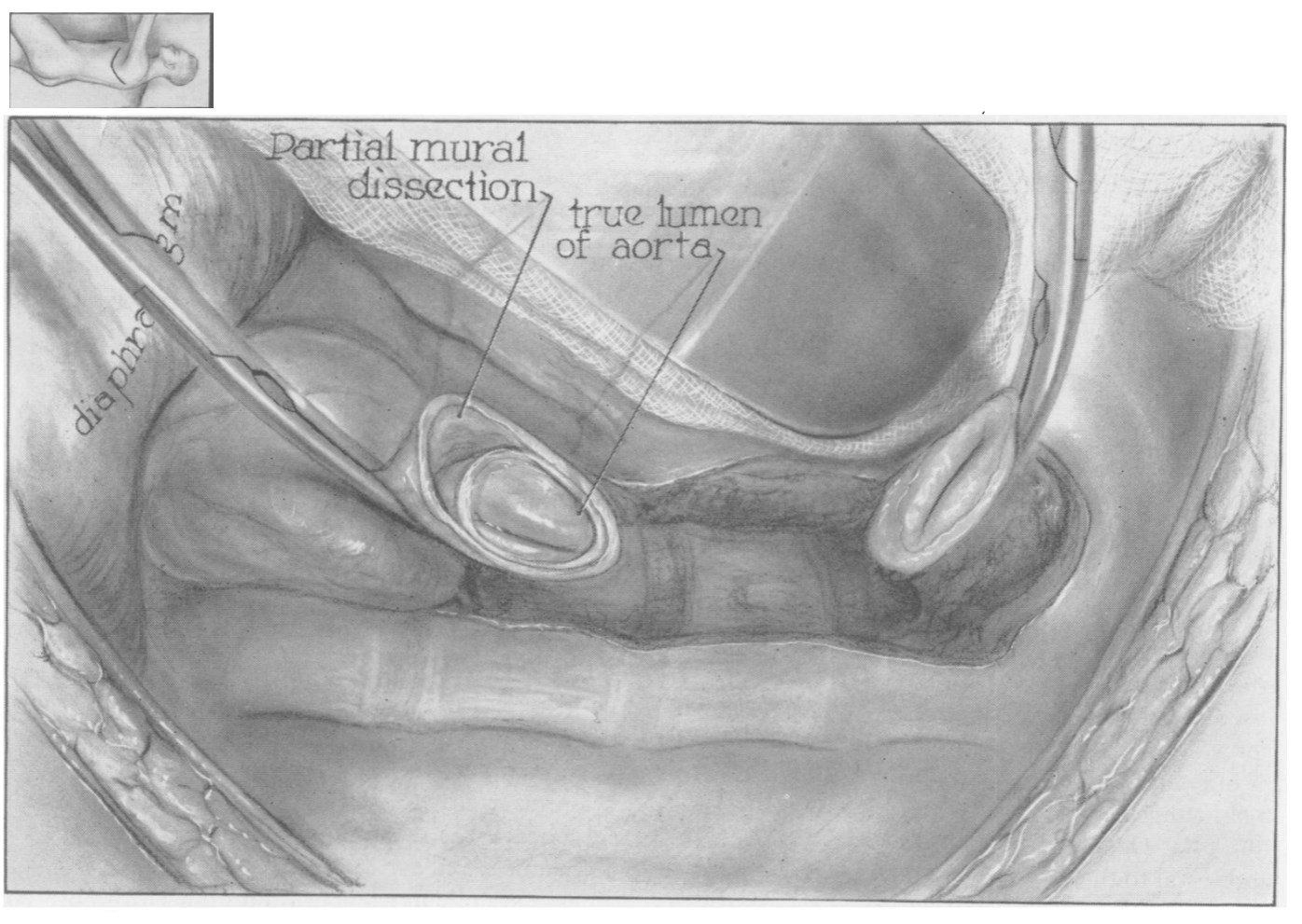
The most common precipitating factor is an intimal tear, usually within 10cm of the aortic valve along the greater curvature of the aorta, where blood peels the tunica intima away from its companion layers and generates a false lumen.
Frequently there is some form of weakening or degeneration of the tunica media, which makes dissection far more likely.
What are the risk factors for aortic dissection?
- Hypertension
- Age
- Smoking
- Hyperlipidaemia
- Cocaine use
- Bicuspid aortic valave
- Marfan's
- Ehlers-Danlos
- Turner's syndrome
- Congenital vascular disease
- Vasculitis
- Trauma
- Coarctation
- Pregnancy
- Instrumentation/catheterisation of the aorta
How it's classified
We love eponymous classifications in medicine, don't we?
Here are the ones you need to trot out in the exam:
Stanford Classfication
- Type A = ascending aorta involved - needs surgery
- Type B = descending aorta only - medical management
The DeBakey Classification
- Type I = ascending aorta, arch and descending aorta
- Type II = ascending aorta only
- Type IIIa = descending as far as diaphragm
- Type IIIb = descending beyond diaphragm
European Society of Cardiology Task Force on Aortic Dissection
These classify conditions that fall under the name of 'acute aortic syndromes' and include:
- Class 1 - Classical aortic dissection
- Class 2 - Intramural haematoma or haemorrhage
- Class 3 - Subtle-discrete aortic dissection
- Class 4 - Plaque rupture or ulceration
- Class 5 - Traumatic or iatrogenic aortic dissection
Acute vs Chronic
There's no such thing as a cute dissection, but there's 'acute' dissection and 'chronic' dissection.
- Acute if <2 weeks
- Chronic if >2 weeks
Simples.
What does it look like?
The medical school description is sudden tearing chest pain that radiates through to the back, and to be fair this is generally pretty accurate.
- Type A dissections usually hurt more in the chest
- Type B dissections are more back or abdomen
- Unsurprisingly they're usually tachycardic and hypertensive from - you know - the agony
- If they're hypotensive then they're probably having some sort of complication, such as tamponade, concomitant MI or rupture
You need to rule out acute MI, largely because you need to manage them very differently, and you really don't want to thrombolyse a dissection.
Imaging
The usual slew of pictures are available to you, but CT angio is first line if your patient is sufficiently stable:
- CT angio - demonstration of true and false lumens
- CXR - wide mediastinum, haemothorax, cardiomegaly
- TTE - intimal flap, tricky in obese patients
- TOE if unstable - intimal flap, aortic regurgitation
- MRI - best pictures but completely unreasonable in unstable patients
What do I do about it?
You're an anaesthetist. You don't fix this - you keep them alive so that someone else can.
Treat their pain, get that blood pressure down, and try to stop the tear from extending by reducing the stress on the wall of the aorta
- Beta blockers (esmolol, labetalol)
- Target a systolic of 110 - 120 mmHg
- Heart rate <70
- Monitor end organ perfusion
Then get in a lift, truck or helicopter and take them to a cardiothoracic surgeon.
Unless it's a type B, in which case management is usually entirely medical with tight blood pressure control and a whole lot of hoping.
Mortality
- Type A = 26% surgical, 58% medical
- Type B = 10.7% medical, 31.4% surgical
This is why we do what we do.
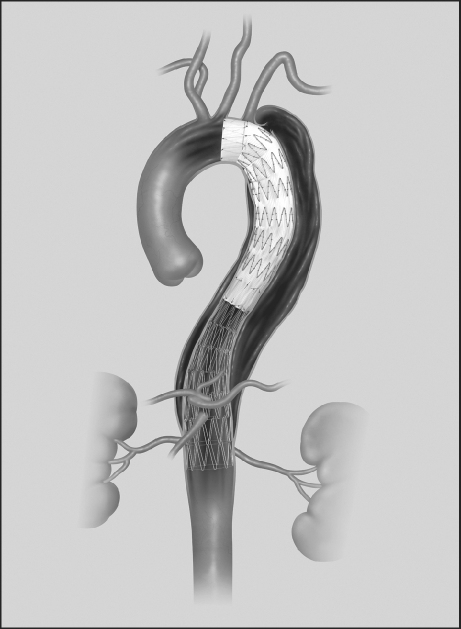
The fix
Type A dissections need urgent surgical repair because rupture is potentially imminent.
The aims of surgery are:
- Prevent dissection extending
- Remove the intimal tear
- Replace the damaged section of aorta
- Fix or replace the aortic valve
If the aortic valve isn't salvageable, then a combined valve and ascending aortic replacement with coronary artery re-implantation is performed.
Basically - big median sternotomy and bypass.
When is surgery indicated for a type B dissection?
- Intractable pain
- Aneurysm expansion
- Ischaemic complications
- Rupture
Basically if they're unstable and medical management isn't working, start cutting.
How to anaesthetise for repair
Not overly complicated here - fairly standard cardiac surgery stuff:
- Careful cardiostable anaesthetic
- Avoid hypertension
- Treat pain
- Optimise perfusion but avoid too much fluid
- Treat coagulopathy
- Use TOE
- Deep hypothermia 18–20°C for cerebral protection
- Left radial artery blood pressure monitoring, as innominate artery may be affected by the dissection
- If you are repairing a Type B dissection surgically, you're looking at one lung ventilation and a left sided thoracotomy
Options for managing blood pressure
- Beta blockers
- Sodium nitroprusside
- Glyceryl trinitrate
- Hydralazine
Free CRQ
Here's a free CRQ shared with permission from the wonderful FRCA Revision
Useful Tweets and Resources
For more DeBakey business, check out:
AORTIC DISSECTION
— Sam Ghali, M.D. (@EM_RESUS) July 10, 2016
Look for a flap. Make a diagnosis. Save a life!#FOAMed #FOAMcc pic.twitter.com/X8Wi6CcGCa
Aortic dissection if not repaired ;mortality can reach up to 50 % in 48 hours. See heart surgeons fixing one below
— Mujeeb Zubair, MD (@MujeebZubair) August 10, 2024
It occurs when an injury to the innermost layer of the aorta allows blood to flow between the layers of the heart.
pic.twitter.com/HIQF0TmgdS
Beautiful repair for chronic aortic dissection with aneurysmal degeneration from June! 4 vessel visceral re-implant seen here. #aorta #aneurysm @JEFFAortic @AorticSurgeonMD @mnooromid pic.twitter.com/kdVDhmf6ih
— Babak Abai (@DrBabakAbai) July 16, 2022
References and Further Reading
Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
Just a quick reminder that all information posted on Anaestheasier.com is for educational purposes only, and it does not constitute medical or clinical advice.
Anaestheasier® is a registered trademark.