Anatomy - Hypothalamus and Pituitary
The amazing Dr Fox has kindly given us permission to share her wonderful quick draw anatomy videos with our readers.
We highly recommend you grab a copy of her book - link is below.
(This is not a sponsored post, nor do we here at Anaestheasier receive any commission from you purchasing through the link below - all proceeds go to the Author!)
Hypothalamus and Pituitary
FRCA Questions
Where is the pituitary found?
- The pituitary sits in the hypophyseal fossa of the sphenoid bone at the base of the skull, outside of the blood brain barrier
- This fossa with its boundaries form the sella turcica which literally translates as 'Turkish saddle' on account of its shape
- The anterior and inferior borders are formed by the sphenoid sinuses
- The posterior border is the clivus of the sphenoid bone
- Immediately superiorly is the diaphragma sellae, a fold of dura through which passes the infundibulum connecting the hypothalamus and pituitary
How big is the pituitary gland?
- 0.5 to 0.9 grams
- Usually around 0.5 x 1.0 x 1.5 cm
What structure lies superior to the pituitary?
- The optic chiasm containing decussating optic nerve fibres lies above the dural diaphragma sellae
What structures lie laterally to the pituitary?
The cavernous sinuses containing:
- Cranial nerves 3, 4, V1, V2 and 6
- Internal carotid artery
How is the pituitary gland divided?
- Two main lobes
- Neurohypophysis lies posteriorly (20% of the volume of the pituitary)
- Adenohypophysis lies anteriorly (80%)
The adenohypophysis is further subdivided into:
- pars distalis - contains the specialised secretory cells
- pars tuberalis
- pars intermedia
The neurohypophysis is divided into:
- pars nervosa
- infundibulum
What are the endocrine functions of the pituitary gland?
The anterior pituitary gland secretes six different hormones and two POMC derivatives:
- Adrenocorticotropic hormone - adrenal steroid and aldosterone production
- Follicle stimulating hormone - oocyte and sperm production
- Growth hormone - bone and muscle growth via IGF-1
- Luteinising hormone - oocyte and sperm production
- Prolactin - milk production and inhibition of gonadotrophins via GnRH
- Thyroid stimulating hormone - thyroid hormone production
- Beta-melanocyte stimulating hormone - skin pigmentation
- Endorphins - inhibition of nociception
The posterior pituitary secretes two:
- Oxytocin - uterine contraction and milk letdown
- Antidiuretic hormone - peripheral vascular resistance and fluid retention
How is pituitary function regulated?
- Directly controlled by the hypothalamus producing stimulatory tropic hormones
- Also via negative feedback - T3 and T4 inhibit release of TRH and TSH
Tell me about the blood supply to the pituitary
- Arterial supply is via branches of the internal carotid via superior and inferior hypophyseal arteries
- The superior hypophyseal artery forms a primary capillary plexus in the hypothalamus that then drains into hypophyseal portal veins that form a plexus around the pars distalis
This forms a hypothalamo-hypophyseal portal circulation that feeds hypothalamic hormones to the pituitary, and then carries pituitary hormones to the body.
What is a portal circulation?
- Any part of the systemic circulation in which blood drains from the capillary bed of one structure through larger vessels to supply the capillary bed of another
There are four portal circulations in the human body:
- Hepatic - (gut and spleen to liver)
- Pituitary - (hypothalamus to pituitary)
- Renal - (glomerulus to vasa recta)*
- Placental - (placenta to foetal liver)**
*People argue about this one, claiming it's a countercurrent exchange system rather than a true portal system, but by the strict definition of capillary bed --> bigger vessel --> capillary bed, it's a portal system.
**People argue about this one too, but technically speaking any blood that doesn't pass through the ductus venosus, and instead passes into the foetal liver, is heading through a portal system.
What can you tell me about pituitary disorders?
Pituitary disorders can be divided into three categories:
- Hyposecretion
- Hypersecretion
- Mass effect
Hyposecretion
- Hypopituitarism
Deficiency in an individual hormone is more common than panhypopituitarism, however pituitary apoplexy can be caused by, haemorrhage or ischaemia such as in Sheehan's syndrome - pituitary infarction caused by peripartum haemorrhage.
Hypersecretion
- Microadenomas
These are less than 10mm and usually result in excessive secretion of a single hormone, rather than all of them.
- Cushing's disease
This is excessive ACTH secretion with increasing glucocorticoid production leading to hyperglycaemia, hypertension and all of the other features of chronic steroid use.
- Acromegaly
This is excessive GH secretion that will lead to either gigantism or acromegaly depending on whether bone growth plates have already fused. The key issues for the anaesthetists are upper airway soft tissue hypertrophy, obstructive sleep apnoea, ischaemic heart disease and cardiomyopathy.
- Prolactinoma
These lead to menstrual dysfunction in females, galactorrhoea and hypogonadism in males. Treatment is with cabergoline or bromocriptine.
Mass effect
- If a macroadenoma (defined by >1cm) expands towards the optic chiasm it can cause a characteristic bitemporal hemianopia
- It needs to get seriously enlarged before it starts causing raised intracranial pressure symptoms
What are your anaesthetic concerns for transsphenoidal hypophysectomy?
- Preoperative endocrine dysfunction
- Bleeding from intentional nasal septal fracture
- Venous air embolism from sitting position
- Limited access to airway
- Rapid emergence to allow neurological assessment
- Post-operative complications include meningitis, CSF rhinorrhoea, cranial nerve damage, diabetes insipidus and panhypopituitarism
More pituitary stuff
Buy the book here
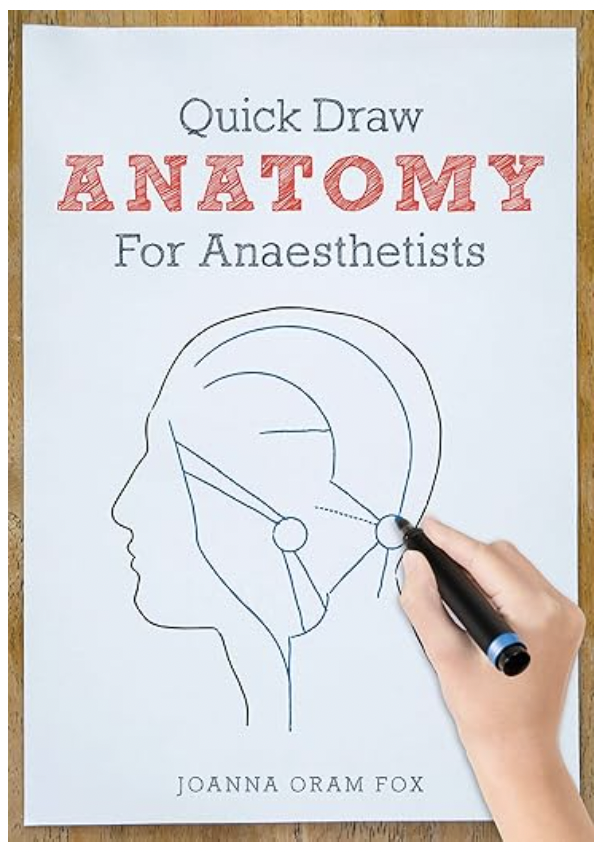
About the Author

Dr Joanna Oram Fox graduated in medicine from Cardiff University in 2007.
She obtained certificates of clinical excellence in medicine, surgery and general practice and won the prestigious Willie Seager surgery prize.
Dr Fox worked four general years as a junior doctor covering medicine, surgery, obstetrics and gynaecology, paediatrics and emergency medicine. During this time she worked in Australia and developed an interest in anaesthetics.
She commenced anaesthetic training in 2011. Dr Fox has been a Consultant Anaesthetist since 2018 and works in Cardiff and Vale NHS trust.
Find her YouTube Channel here


