Acute Spinal Cord Injury
Take home messages
- Half of patients with acute spinal cord injury will have an incomplete lesion
- The key is preventing secondary injury
- The first 72 hours are critical for determining long term prognosis
What is it?
"An insult to the spinal cord causing transient or permanent loss of spinal sensory, motor and autonomic function"
What are the two components of acute spinal cord injury?
- Primary injury due to direct compression, haemorrhage or traction forces
- Secondary injury due to haemorrhage, oedema, neurogenic shock, hypoperfusion and cord ischaemia
Who gets it?
Generally speaking it's young patients (average around 30-35 years) when talking about traumatic injury.
10-15% of spinal fractures will result in some form of cord injury:
- The incidence is around 13 per 1,000,000 in the UK
- Half of these are incomplete
- Half of these will be able to walk out of hospital
What are the causes of traumatic spinal cord injury in the UK?
- Motor vehicle accidents (40% ish)
- Falls (40% ish)
- Sports injury (10% ish)
- Assault and penetrating trauma (3%)
What are the non-traumatic causes of spinal cord injury?
It won't surprise you that these are generally seen in an older cohort of patients, but are still very much possible in young people as well.
- Infection
- Tumour
- Cyst
- Inflammation
- Stroke
- Congenital
- Degenerative disease
What factors determine the clinical outcome of spinal cord injury?
- Age
- Degree of injury
- Level of injury
- Associated complications
Sadly, most patients who die during the 'chronic' phase do so as a result of often avoidable complications such as respiratory and urinary tract infections, pressure sores and venous thromboembolism.
How to avoid the avoidable complications
- VTE prophylaxis
- Gastroprotection
- Early identification and treatment of infection
- High quality pressure area care (get them off the scoop asap)
- Psychological support
So what happens?
For what is on the surface often a very simple mechanism of injury, the pathophysiology of acute spinal cord injury is often complex and weird.
The primary injury
- The cord is physically damaged by compression and traction forces
- The usual culprit is subluxation of vertebral material
- Other injury patterns include hyperextension and retropulsion
- Don't forget direct penetrating injury as well
The secondary injury
- After the initial insult, there is bleeding into the central grey matter
- Spinal cord oedema then impairs local blood supply leading to ischaemia
- This is made doubly bad by any hypotension and autonomic dysfunction seen in high thoracic lesions
- Then much like a stroke, this damage will spread in both directions along the cord and worsen if left untreated
A patient with a C4 injury will still have diaphragmatic function (C3-5) but if not treated appropriately in the acute setting, the injury can spread north to C3 and higher, leaving the patient requiring permanent ventilation.
What is the difference between spinal shock and neurogenic shock?
- Neurogenic shock refers to the hypotension caused by loss of peripheral vascular resistance as a result of widespread loss of sympathetic tone, as seen after a high thoracic spinal cord injury
- Spinal shock is not 'shock' in the circulatory sense, it simply refers to the total loss of motor function and sensation distal to the spinal cord lesion
What are the stages of spinal shock?
- Areflexia - 0-1 days
- Initial reflex return days - 1-2 days
- Early hyperreflexia - 4-28 days
- Late hyperreflexia - 1-12 months
If you're wondering why monosynaptic motor reflexes are absent even though the lesion is higher up, it's because even monosynaptic reflexes rely on tonic descending facilitation to work.
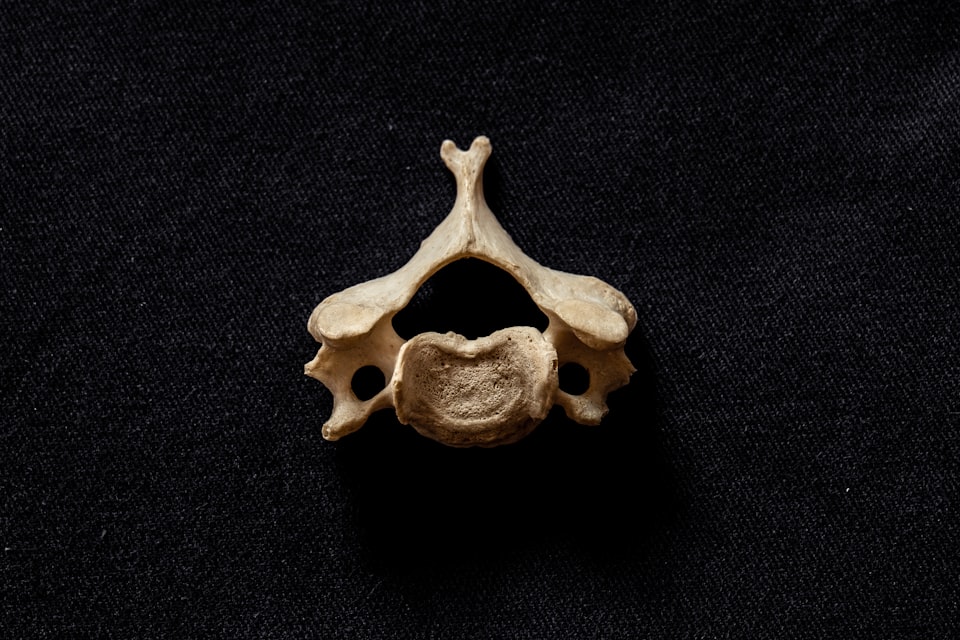
Some Anatomy
Spine bits you need to know
- The ligaments (flavum, interspinous, supraspinous)
- The processes (spinous, transverse)
- The complexes (anterior, middle, posterior)
- The joints (intervertebral, facets)
The posterior complex is the strongest, and if two complexes are disrupted then the column is deemed unstable.
The mid-thoracic spinal canal is narrowest, with highest risk of injury from retropulsion of vertebral bone or disc material.
Injury usually occurs at locations where there is a change in curvature or vertebral type:
- Craniocervical junction
- Cervicothoracic junction
- Thoracolumbar junction
- Lumbosacral junction
The cord itself
A full review of spinal cord anatomy is beyond the scope of this post, but we'll quickly tick off the bits that score you marks in the exam.
A brief review of spinal cord anatomy
The spinal cord extends from the brainstem to L1/2 in 90% of adults (some as low as L3) and L2/3 in the neonate.
Sensory pathways
- Posterior columns - ipsilateral vibration, fine touch, proprioception
- Spinothalamic tracts - contralateral pain, temperature and coarse touch
Motor pathways
- Corticospinal tracts - descending motor control
Arterial supply
- 1 anterior spinal artery, from the vertebral artery
- 2 posterior spinal arteries, from the posterior inferior cerebellar arteries
- Radicular arteries (artery of Adamkiewicz)
The anterior spinal artery is at risk from retropulsion of vertebral bone or discs, particularly around C7.
What are the anaesthetic concerns?
Well, rather a lot really, given it can have a profound impact on virtually every system in the body, not least the cardiovascular and respiratory systems that we hold so dear in our hearts (and lungs?).
When answering this question, as always it's best to break it down by organ system, and drift through in a logical fashion.
Airway concerns
- First of all, don't get distracted by people talking about a spinal cord injury, and make sure you're happy with airway, breathing and circulation
- It is not uncommon for c-spine injury patients to also have max-fax injuries and blood in the mouth
- Manual inline stabilisation is key, especially in suspected cervical cord injury, and will make your intubation harder
- Trauma patients are more likely to aspirate for many reasons, so definitely RSI if intubating
- Using a hyperangulated videolaryngoscope blade may help reduce mechanical strain on the neck during intubation, as well as the concomitant haemodynamic effects of laryngoscopy*
*Flexion is thought to be more dangerous to a c-spine injury than extension, and remember to keep their head stable once they're paralysed and intubated.
Cardiovascular concerns
- Huge initial catecholamine release with sudden hypertension and tachycardia
- Then paralysis of sympathetics causes hypotension - usually ending up with a systolic around 80mmHg
- Arrhythmia
- Vasodilatation
- Bradycardia - especially with bladder distension so catheterise early
- Hypotension may be fluid-resistant and require vasopressors
- Risk of ischaemic heart disease due to immobility
- Autonomic dysreflexia (more of a chronic issue but often gets a mark)
If you're intubating a patient with a high cord lesion, consider atropine to prevent profound bradycardia on laryngoscopy.
Oh, and definitely put in an arterial line.
Respiratory concerns
- Intercostal failure leads to reduced tidal volume
- Vital capacity reduced to 30-80% of original
- Breathing worse in sitting position as abdomen pulls diaphragm down, reducing room for expansion
- Worse V/Q mismatch and atelectasis
- Poor cough and secretion clearance
- May require short or long term ventilation
- Oxygenation is key to prevent hypoxic secondary neuronal death
How do different lesion levels affect respiratory function?
- Above C3 - diaphragmatic failure, needs immediate and ongoing ventilation
- C3-C5 - variable diaphragm function - 80% require ventilation
- C5-T8 - loss of intercostals - weak cough, may require short term ventilation, usually don't require longer term support
- Below T8 - weak cough due to loss of abdominal muscles so may need short term support
GI concerns
- Reduced gastric motility
- Delayed gastric emptying (increased risk of aspiration)
- Constipation
- Paralytic ileus
- Pseudo-obstruction
- Increased incidence of gallstones
- Stress ulceration*
*Unopposed vagal activity stimulates gastric acid production. Gastroprotection with a PPI for six weeks substantially reduces incidence of ulceration.
Temperature control concerns
- Vasodilatation below the level of injury
- Anhidrosis below the injury
- Reflex hyperhidrosis above the injury
- Inability to shiver below the injury
- Loss of sensation to heat or cold below injury
- Reduced muscle mass and metabolic rate
What features may indicate spinal cord injury in a low GCS patient?
- Unexplained hypotension
- Warm dry feet
- Priapism
- Inappropriate bradycardia
- Flaccidity in legs but not arms
- Areflexia in legs but not arms
- No response to pain in legs but response to pain higher up
And the big question we're going to be asking in resus
What are the indications for intubation in acute cervical spinal cord injury?
- High cervical cord injury
- Rapid shallow breathing
- Vital capacity less than 15ml/kg
- Worsening vital capacity trend
- Hypercapnoea
- Poor cough
- Exhaustion
What should I do with my drugs?
Much the same as you'd usually do for any other patient, but pay particular attention to the haemodynamics, especially if intubating and positive pressure ventilating, as these patients tolerate hypovolaemia very poorly.
Suxamethonium
This is prime exam fodder, so make sure you know it.
Autonomic dysreflexia
This is associated with chronic spinal cord injury, and generally won't happen in a patient with an acute injury, but it gets examined so frequently we'd be doing you a disservice if we didn't at least mention it here.
Stimuli that aren't usually all that painful, below the level of the lesion, can trigger an excessive sympathetic reflex response and severe peripheral vasoconstriction.
This triggers headache, flushing and severe hypertension with risk of stroke, seizures and retinal haemorrhage.
There is usually a reflex bradycardia and vasodilatation above the lesion, but the blood pressure remains very high without active management.
Classically the cause is a distended bladder, which is why early catheterisation is a good idea in chronic spinal cord injury patients.
Patients are generally very will informed about this condition and may well have dealt with it many times before - so ask them about it and how they usually manage it.
What are the signs and symptoms?
- Pounding headache
- Blurred vision
- Flushing above the level of the spinal cord injury
- Profuse sweating
- Goosebumps and chills (but no fever)
- Bradycardia*
- Severe hypertension
*This is a baroreceptor reflex due to the sudden hypertension - the same as is seen with metaraminol
What are the common causes?
- Bladder irritation - distension, UTI
- Bowel irritation - constipation, suppositories
- MSK - pressure sores, burns, ingrown toenail, ulcers
- Uterine contractions
- Fractures
- Acute intra-abdominal pathology
What's the treatment?
- Figure out what's causing it and treat that
- If systolic >170mmHg then start emergency medical management
- Glyceryl trinitrate NB: DO NOT use glyceryl trinitrate if sildenafil (Viagra) or vardenafil (Levitra) has been taken in the previous 24 hours or tadalafil (Cialis) in the previous 4 days. Give one spray of glyceryl trinitrate (Nitrolingual Pump spray) under the tongue. During administration the canister should be held uptight and the spray should not be inhaled. OR Apply 5 mg, transdermal patch to chest and upper arms according to manufacturer’s instructions. Remove patch once BP settles or if the BP drops too low.
- Blood pressure should start to drop within 2 minutes of GTN administration and last around half an hour
- Give another dose if inadequate response after 5 to 10 minutes
Note the contraindication to GTN:
- Sildenafil (or vardenafil/tadlafil) within last 24 hours
- If so then consider hydralazine, clonidine or something like captopril - check your local guidelines
Probably best to contact your local spinal service as well for ongoing advice.
Can we fix it?
Currently the main focus is on preventing that critical secondary neuronal damage, but there are avenues investigating actively repairing damaged nerve pathways, including:
- Antioxidants
- Anti-inflammatories
- Calpain-inhibitors
- Stem cell therapy
- Gene therapy
- Electrotherapy
Oh and there's also Neuralink, which looks awesome, but that's probably not going to be on any FRCA mark schemes any time soon.

Free CRQ from FRCA-revision.com
Useful Tweets
🔓How to manage acute cervical spinal cord injury in the non-specialist ICU?@STHJournalClub and @frantait85 take us through all the current evidence, including airway management, weaning, autonomic dysreflexia and rehabilitation👇
— 𝘈𝘯𝘢𝘦𝘴𝘵𝘩𝘦𝘴𝘪𝘢 (@Anaes_Journal) February 8, 2024
🔗https://t.co/4OR8pe68Lm pic.twitter.com/RAL5gJaYeN
References and Further Reading

Primary FRCA Toolkit
While this subject is largely the remit of the Final FRCA examination, up to 20% of the exam can cover Primary material, so don't get caught out!
Members receive 60% discount off the FRCA Primary Toolkit. If you have previously purchased a toolkit at full price, please email anaestheasier@gmail.com for a retrospective discount.

Discount is applied as 6 months free membership - please don't hesitate to email Anaestheasier@gmail.com if you have any questions!
